Acute fatty liver of pregnancy is a rare but severe liver disorder that occurs in late pregnancy. It causes sudden fat buildup inside liver cells. This buildup blocks normal liver work. Without fast care, both you and your baby face serious risk. Early delivery and hospital treatment greatly improve survival. Many early signs look in liver, which makes awareness critical.
Table of Contents
ToggleAcute fatty liver of pregnancy often appears in the third trimester. It can worsen within hours or days. The liver controls blood sugar, clotting, and toxin removal. When it fails, the body shuts down quickly. Fast diagnosis and urgent delivery remain the most effective steps.
What Causes Acute Fatty Liver of Pregnancy
Acute fatty liver of pregnancy develops when fat metabolism breaks down during late pregnancy. The liver becomes overloaded with fatty acids it cannot process, leading to sudden liver dysfunction. This failure is driven mainly by genetic and metabolic factors, not lifestyle or diet.
Genetic Factors and Fatty Acid Oxidation Defects
Your body uses enzymes to break down fats. Some pregnancies expose hidden enzyme problems. These defects affect fatty acid oxidation, which means fat cannot be converted into energy.
Key points you should know:
- The defect often comes from the baby, not you
- Fat breakdown slows or stops
- Toxic fat byproducts enter your blood
- Liver cells fill with fat droplets
These inherited issues explain many causes of acute fatty liver of pregnancy . You may have no symptoms until late pregnancy stress reveals the problem.
Role of Fetal LCHAD Deficiency
LCHAD stands for long-chain 3-hydroxyacyl-CoA dehydrogenase. It is an enzyme needed to process fats. Some babies lack this enzyme.
When the fetus cannot process fats:
- Fat byproducts pass through the placenta
- Your liver must handle the overload
- Liver damage begins rapidly
This link explains why symptoms improve after delivery. Removing the placenta removes the trigger. This mechanism represents one of the best-studied causes of acute fatty liver of pregnancy .
Hormonal and Metabolic Triggers
Late pregnancy changes how your body handles fat. Estrogen levels rise. Fat breakdown increases. The liver works harder than usual. If fat handling fails:
- Blood sugar drops
- Ammonia levels rise (ammonia is a toxic waste product)
- Liver cells swell and malfunction
These changes do not cause the disease alone. They push an already stressed system toward failure.
Risk Factors in Pregnancy
Certain factors raise concern but do not guarantee disease:
- First pregnancy
- Twin or multiple pregnancy
- Male fetus
- Low body weight before pregnancy
- History of liver problems
These factors increase stress on fat metabolism. They contribute to causes of acute fatty liver of pregnancy but do not act alone.
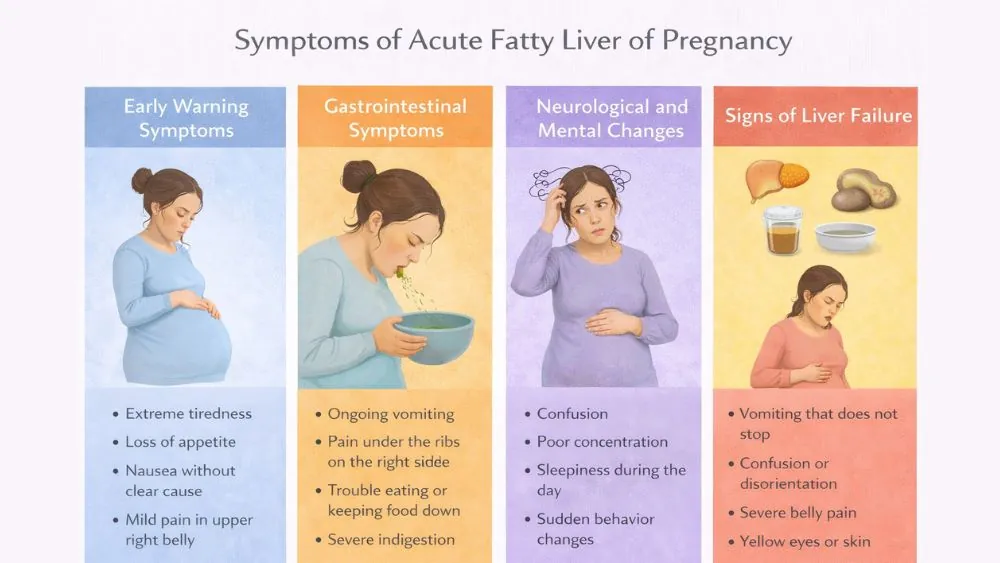
Symptoms of Acute Fatty Liver of Pregnancy
The symptoms of acute fatty liver of pregnancy often start mild but worsen quickly. Early signs may resemble common pregnancy discomforts, which delays care. As liver function drops, toxin buildup and clotting failure cause serious, life-threatening symptoms.
Early Warning Symptoms
Early signs often appear between weeks 30 and 38. Common early signs include:
- Extreme tiredness
- Loss of appetite
- Nausea without clear cause
- Mild pain in the upper right belly
These early symptoms of acute fatty liver of pregnancy often lack fever or high blood pressure. That makes them easy to ignore.
Gastrointestinal Symptoms
As liver stress increases, stomach symptoms worsen. You may notice:
- Ongoing vomiting
- Pain under the ribs on the right side
- Trouble eating or keeping food down
- Severe indigestion
These signs occur because the liver cannot process fats or toxins properly.
Neurological and Mental Changes
The liver clears toxins from your blood. When it fails, toxins reach the brain. Watch for:
- Confusion
- Poor concentration
- Sleepiness during the day
- Sudden behavior changes
These neurological signs mean toxins like ammonia are rising. They are serious symptoms of acute fatty liver of pregnancy .
Signs of Liver Failure
Advanced disease shows clearer danger signs. These include:
- Yellowing of skin or eyes (jaundice means bilirubin buildup)
- Dark urine
- Pale or gray stool
- Easy bruising or bleeding
Bleeding occurs because the liver makes clotting proteins. When liver cells fail, clotting drops fast.
Symptoms That Require Emergency Care
You should seek emergency care if you have:
- Vomiting that does not stop
- Confusion or disorientation
- Severe belly pain
- Yellow eyes or skin
These symptoms of acute fatty liver of pregnancy indicate rapid liver failure. Delay can be fatal.
How Is Acute Fatty Liver of Pregnancy Diagnosed
Doctors diagnose this condition based on symptoms, blood tests, and exclusion of similar disorders. No single test confirms acute fatty liver of pregnancy . Diagnosis requires careful evaluation.
Clinical Evaluation and Physical Findings
Doctors assess:
- Mental alertness
- Blood pressure
- Belly tenderness
- Signs of jaundice
Your pregnancy stage matters. Late pregnancy symptoms raise suspicion. Rapid worsening increases urgency.
Blood Tests and Liver Function Tests
Blood work reveals liver damage and metabolic failure. Common findings include:
- High liver enzymes causes (signals liver cell injury)
- Low blood sugar (hypoglycemia means low glucose)
- High ammonia levels
- Low platelets (cells that help clot blood)
These results support diagnoses of acute fatty liver of pregnancy when combined with symptoms.
Imaging Studies
Ultrasound may show fatty liver. Results vary. A normal scan does not rule out disease. CT scans can detect fat, but doctors avoid them unless necessary during pregnancy. Imaging supports but does not confirm diagnoses of acute fatty liver of pregnancy .
Swansea Criteria for AFLP
Doctors often use the Swansea criteria. This system lists clinical and lab features. Examples include:
- Vomiting
- Abdominal pain
- Low blood sugar
- High bilirubin
- Kidney impairment
Six or more features suggest a diagnosis of acute fatty liver of pregnancy when no other cause explains the findings.
Differentiating AFLP From HELLP Syndrome
AFLP and HELLP can look similar. They differ in key ways.
AFLP usually shows:
- Low blood sugar
- High ammonia
- Severe liver failure
HELLP usually shows:
- High blood pressure
- Red blood cell breakdown
- Severe platelet loss
Clear testing helps separate diagnoses of acute fatty liver of pregnancy from other pregnancy emergencies.
Treatment for Acute Fatty Liver of Pregnancy
Treatment for acute fatty liver of pregnancy focuses on stabilizing your body and delivering the baby as soon as safely possible. Supportive hospital care protects the liver, brain, kidneys, and blood clotting system while the underlying trigger is removed.
Immediate Stabilization of the Mother
Doctors first focus on keeping you stable. Your blood sugar often drops because the liver cannot release glucose. Low sugar can damage the brain.
Key actions include:
- Giving glucose through IV to correct low blood sugar
- Managing fluids to avoid swelling or shock
- Correcting electrolyte imbalance (salt and mineral levels in blood)
- Monitoring breathing and heart rate closely
This step forms the foundation of treatment for acute fatty liver of pregnancy and begins as soon as the condition is suspected.
Emergency Delivery Planning
Delivery is the only way to stop disease progression. The placenta plays a central role in triggering liver failure. Doctors decide the safest method based on:
- Your stability
- Bleeding risk
- Fetal condition
Vaginal delivery may be possible if labor is already progressing. Cesarean delivery is used when speed matters. Ending the pregnancy removes the metabolic stress driving acute fatty liver of pregnancy .
Intensive Care Management
Many women need care in an intensive care unit. This allows constant monitoring and fast response to complications. ICU care often includes:
- Blood products to correct bleeding risk
- Oxygen or breathing support if needed
- Frequent lab tests to track liver and kidney function
This stage of treatment for acute fatty liver of pregnancy prevents organ failure from worsening.
Management of Liver and Kidney Complications
The liver and kidneys work together. When the liver fails, kidney injury often follows. Doctors manage this by:
- Adjusting fluids carefully
- Using dialysis if waste products build up
- Avoiding medicines that stress the liver
Liver transplant remains rare. Most women recover once the trigger is removed.
Post-Delivery Monitoring and Recovery
After delivery, recovery begins, but risk remains. Liver function usually improves within days. Doctors continue to:
- Monitor liver enzymes
- Check blood clotting levels
- Track mental alertness
Full recovery often takes weeks. This completes active treatment for acute fatty liver of pregnancy .
Complications of Acute Fatty Liver of Pregnancy
Without rapid treatment, acute fatty liver of pregnancy can cause multi-organ failure. The liver, kidneys, brain, and blood clotting system may all be affected.
Acute Liver Failure
Liver failure is the most serious complication. The liver stops filtering toxins and making clotting proteins. This leads to:
- Toxin buildup in blood
- Confusion or coma
- Severe bleeding risk
Prompt delivery reduces this risk greatly.
Kidney Failure
Kidney injury occurs due to toxin buildup and low blood flow. Urine output may drop sharply. In severe cases:
- Dialysis supports kidney function
- Recovery may take weeks
Most kidneys recover once liver function improves.
Coagulopathy and Bleeding
The liver produces clotting factors. When it fails, blood does not clot properly. This causes:
- Internal bleeding
- Excessive bleeding during delivery
- Bruising without injury
Doctors manage this with plasma and clotting factor support.
Infection and Sepsis
Low immunity and invasive procedures raise infection risk. Bacteria can enter the bloodstream. Signs include:
- Fever
- Low blood pressure
- Rapid heart rate
Early antibiotics reduce severe outcomes.
Maternal and Fetal Outcomes
With early care:
- Maternal survival exceeds 90 percent
- Fetal survival improves significantly
Delayed care raises death risk for both mother and baby in acute fatty liver of pregnancy .
Prevention of Acute Fatty Liver of Pregnancy
True prevention of acute fatty liver of pregnancy is limited because genetic factors play a major role. However, early symptom recognition, close monitoring of high-risk pregnancies, and fast hospital evaluation reduce severe outcomes.
Can AFLP Be Prevented?
There is no guaranteed way to prevent AFLP. Diet, exercise, and supplements do not stop it. What helps:
- Early symptom reporting
- Rapid hospital evaluation
These steps reduce complications and improve outcomes.
Genetic Counseling and Screening
Families with prior AFLP benefit from genetic counseling. Testing can identify fatty acid oxidation disorders. This helps plan:
- Future pregnancies
- Early monitoring
It supports informed decisions about the prevention of acute fatty liver of pregnancy risks.
Monitoring High-Risk Pregnancies
High-risk women need closer follow-up in late pregnancy. Monitoring includes:
- Frequent blood tests
- Symptom tracking
- Early admission if concerns arise
This reduces the late diagnosis of acute fatty liver of pregnancy .
Early Symptom Recognition
You should report nausea, vomiting, or confusion promptly. These symptoms are not normal late pregnancy signs. Early recognition remains the most effective tool in the prevention of acute fatty liver of pregnancy complications.
Outlook and Prognosis
With timely care, most women recover fully from acute fatty liver of pregnancy . Liver function often returns to normal within weeks. Long-term liver damage is uncommon when treatment and delivery occur early.
Maternal Recovery Timeline
Liver enzymes often normalize within weeks. Energy and appetite return gradually. Most women:
- Leave the hospital within two weeks
- Regain full strength in months
Long-term disability is uncommon.
Long-Term Liver Health After AFLP
Permanent liver damage is rare. The liver regenerates well once stress ends. Follow-up tests usually show:
- Normal liver function
- No chronic disease
This reassures long-term health after acute fatty liver of pregnancy .
Future Pregnancy Considerations
Recurrence risk exists but remains low. Careful planning improves safety. Future pregnancies should include:
- Early specialist care
- Genetic review
- Close third-trimester monitoring
When to See a Doctor
Any unexplained nausea, vomiting, confusion, or jaundice in late pregnancy requires urgent medical attention. Early evaluation prevents rapid progression of acute fatty liver of pregnancy and protects both mother and baby.
Symptoms That Should Never Be Ignored
You should seek care for:
- Persistent vomiting
- Confusion or sleepiness
- Yellow eyes or skin
These signs suggest worsening acute fatty liver of pregnancy .
When to Go to the Emergency Room
Go immediately if symptoms escalate quickly. Emergency care prevents organ failure.
FAQs
Is acute fatty liver of pregnancy life-threatening?
Yes. Acute fatty liver of pregnancy can become fatal within days if untreated. Early delivery and intensive care greatly reduce the risk of death for both mother and baby.
How rare is acute fatty liver of pregnancy?
Acute fatty liver of pregnancy occurs in about 1 out of 7,000 to 15,000 pregnancies. Despite being rare, it requires urgent care due to its rapid progression.
Can AFLP happen in early pregnancy?
No. Acute fatty liver of pregnancy almost always occurs in the third trimester or early postpartum period because late pregnancy increases fat metabolism stress.
How is AFLP different from HELLP syndrome?
AFLP causes severe liver failure and low blood sugar, while HELLP involves high blood pressure and blood cell breakdown. Correct diagnosis guides proper care.
Can acute fatty liver of pregnancy recur?
Recurrence is possible but uncommon. Women with prior acute fatty liver of pregnancy should receive close monitoring in future pregnancies.
Does AFLP affect the baby after birth?
Some babies may have fatty acid oxidation disorders. Early testing helps guide feeding and care after birth.
How long does liver recovery take after AFLP?
Most women recover liver function within weeks. Full physical recovery may take several months after acute fatty liver of pregnancy .
Can AFLP be detected before symptoms start?
There is no reliable screening test. Awareness of risk factors and early symptoms improves early detection.
Is vaginal delivery possible with AFLP?
Yes, if the mother remains stable and labor progresses safely. Delivery choice depends on urgency and bleeding risk.
Should future pregnancies be closely monitored?
Yes. Women with past acute fatty liver of pregnancy need early specialist care and frequent monitoring to reduce risk.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.