If you or someone you love has primary sclerosing cholangitis (PSC), you’re looking for treatment. PSC is a liver disease that keeps getting worse. It causes the bile ducts to get inflamed and scarred. This can block the flow of bile, damage the liver, and cause severe health problems if not treated. This article will dive into the various ways to treat PSC. We want to help you and your medical team choose the best path for your care.
Table of Contents
ToggleThis article covers everything from what causes sclerosing cholangitis to its symptoms. We’ll also look at the newest medical and surgical treatments available. It’s designed to give you the info you need to deal with this tough condition. Whether you’re dealing with sclerosing cholangitis symptoms or just want to improve your quality of life, you are in the right place. The tips here will point you to the best sclerosing cholangitis treatment for you.
Understanding Primary Sclerosing Cholangitis
Definition and Causes
Primary sclerosing cholangitis or PSC is a chronic, progressive liver disease. It causes inflammation and scarring of the bile ducts. This occurs both inside and outside the liver. The exact cause is unknown, but it might be due to an autoimmune response. This response mistakenly attacks the bile ducts. Genetic and environmental factors could also be involved in PSC.
Epidemiology and Risk Factors
PSC is rare, affecting 0.9 to 1.3 people per 100,000 yearly. It’s more common in men and occurs in adults aged 30 to 50. If you have inflammatory bowel diseases like ulcerative colitis or Crohn’s disease, your risk of getting PSC is higher. Factors like genetics and the environment can also raise your PSC risk.
Pathogenesis and Genetic Factors
The exact causes of PSC are not fully understood. It’s thought to involve both genetics and the environment. Research has found several genetic factors linked to PSC. These genes affect our immune system and the health of bile ducts. Changes in the gut’s bacteria and environmental elements may also influence PSC’s development and impact.
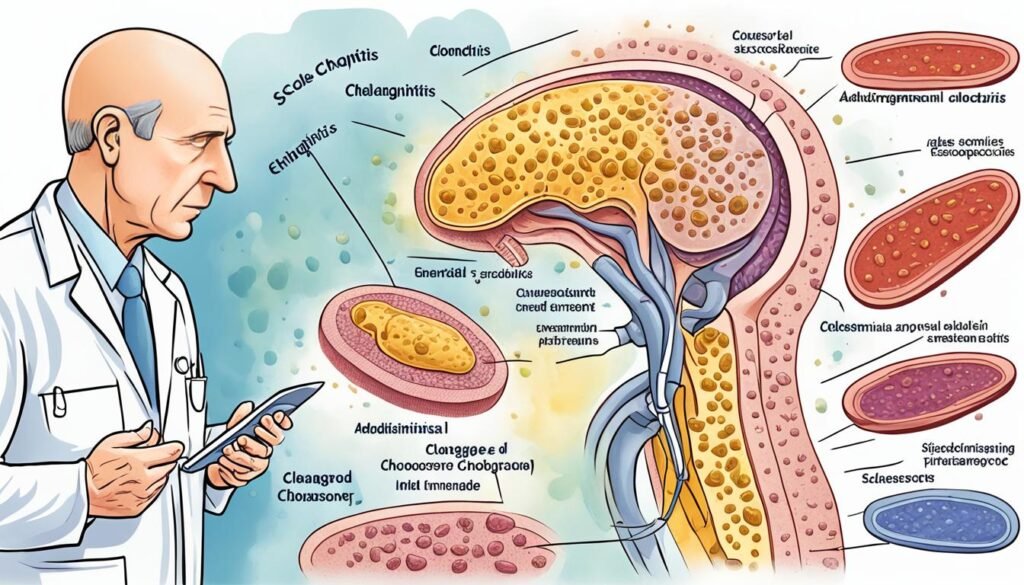
Diagnosis of Primary Sclerosing Cholangitis
Diagnosing primary sclerosing cholangitis involves several tests and procedures. Each diagnostic tool plays a crucial role in making an accurate assessment. These steps are vital in guiding the right treatment for patients.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP uses a flexible tube with a camera to see inside the bile and pancreatic ducts. A dye is then injected to make these ducts visible on X-rays. This method is key in recognizing PSC by noting the “beading” or narrowing of these ducts, a sign of the disease.
Liver Biopsy
A liver biopsy may be done to confirm PSC and check liver damage. A thin needle takes a tiny piece of liver tissue for examination. Doctors look for specific signs like bile duct inflammation and scarring during the biopsy.
Liver Function Tests and Imaging
Blood tests that check liver enzyme levels can hint at PSC. Imaging tests like MRCP or CT scans help doctors see the bile ducts’ condition. These tests are crucial in spotting PSC traits.
Medical Management of Primary Sclerosing Cholangitis
People with primary sclerosing cholangitis (PSC) often deal with severe itching, called pruritus. Many medical treatments can help control this. Medicines like bile acid sequestrants, antibiotics (like rifampin), antihistamines, and opioid antagonists lessen the itch. For itching linked to liver disease, ursodeoxycholic acid (UDCA) may also offer relief.
Treatment for Itching
The intense itching known as pruritus can be overwhelming for those with sclerosing cholangitis. Bile acid sequestrants, including cholestyramine or colestipol, are usually the first choice for treatment. Rifampin, antihistamines, and naltrexone can also help. UDCA has been found to decrease itching from liver conditions.
Antibiotic Therapy for Infections
Bacterial infections, especially in the bile ducts, are common complications for PSC patients. Doctors may give prophylactic antibiotic therapy to avoid these infections. Antibiotics might also be used around certain procedures, like ERCP, to lower infection risks and help heal faster.
Nutritional Support
PSC patients can have trouble absorbing vitamins and nutrients because of liver and bile flow issues. They need vitamin and mineral supplements, and sometimes dietary changes, for good nutrition. This is very important for managing their liver condition.

Endoscopic and Surgical Interventions
People with primary sclerosing cholangitis (PSC) often face blocked bile ducts. Endoscopic approaches are key in addressing these issues. Balloon dilation uses a balloon to make small bile ducts wider. This helps bile flow better. Another method is stent placement. A tube, either plastic or metal, is put in a bile duct to keep it open.
For those with severe liver disease or complications, a liver transplantation might be needed. Here, a sick liver is removed and replaced with a healthy donated one. This can offer a cure for PSC. Yet, the disease might come back in the new liver for some people.
Sclerosing Cholangitis Treatment
Sclerosing cholangitis (SC) treatment involves different steps. It aims to manage symptoms, slow down the disease, and deal with complications. This includes medicine, procedures, and sometimes surgery. The plan depends on the person’s symptoms, health, and disease stage.
Medical therapy is crucial for SC. It involves drugs that bind bile acids, easing itchiness. Doctors might also use antibiotics for infections.
When the bile ducts are blocked, they may do a procedure called ERCP. This opens the ducts and places stents to keep them open. It improves bile flow and decreases complications. They might also suggest medicines to reduce itchiness.
If SC leads to serious liver issues, more steps are necessary. This could be a combination of drugs, procedures, or surgery. A liver transplant is an option if needed.
Treating SC needs a team effort. Specialists such as liver doctors, GI doctors, surgeons, and transplant experts work together. They watch closely for any cancer signs or other issues. This helps in the ongoing care.
The main aim is to help manage symptoms, slow the disease, and better life quality. Working with experts lets patients understand their treatment choices. This helps them make the best decisions for their health.
Lifestyle and Complementary Therapies
Your lifestyle choices are key in handling primary sclerosing cholangitis (PSC). It’s crucial to steer clear of alcohol since it harms your liver more. Also, make sure you’re vaccinated against hepatitis A and B. This stops more harm to your liver.
Reducing stress and being active can improve how you feel with PSC. Things like meditation, yoga, and other ways to relax can lower your stress. This makes it easier to deal with PSC. Exercising a bit can keep you fit and ease some PSC symptoms.
Alcohol Avoidance and Hepatitis Vaccination
Avoiding alcohol is a must if you have PSC to protect your liver from more harm. Keep your vaccinations up to date, including those for hepatitis A and B. Safeguarding your liver is vital for your care plan.
Stress Management and Exercise
Reducing stress helps manage PSC symptoms and might slow down the disease. Try stress-relief methods like meditation or yoga every day. And regular, light exercise supports your health and might ease PSC symptoms.
Complications and Associated Conditions
Living with primary sclerosing cholangitis (PSC) comes with many difficulties. These issues can greatly change life quality. It’s crucial to understand these challenges for better patient care.
Fatigue and Depression
Debilitating fatigue is a common problem for PSC patients. They feel tired all the time, even after resting. This exhaustion, along with the chronic disease, can lead to depression. Doctors need to talk about these issues with patients. They should consider using medicine, therapy, or lifestyle changes to help.
Osteoporosis and Bone Disorders
PSC might increase the risk of osteoporosis and other bone problems. A lack of calcium and vitamin D from poor bile flow and liver issues is often to blame. Getting regular bone density tests and taking supplements can help maintain bone health.
Colorectal Cancer and Cholangiocarcinoma
People with PSC are more likely to get certain cancers, like colorectal or bile duct cancer. It’s essential they have screenings like colonoscopies for early cancer detection. Regular checks and quick treatments are key to better outcomes for these patients.
Prognosis and Monitoring
The outlook for people with primary sclerosing cholangitis (PSC) varies a lot. This is based on how bad the disease is and what stage it’s at. Getting alkaline phosphatase levels back to normal is really good news for patients. It’s related to a better prognosis for sclerosing cholangitis. Doctors will watch your liver function, especially alkaline phosphatase, to see how the disease is moving. They use these tests to decide on the best treatments.
Cancer Surveillance
Having PSC also means a higher risk of cancer. That’s why keeping up with cancer checks is vital. You might need regular colonoscopies to look for colorectal cancer. And doctors will also keep an eye out for cholangiocarcinoma. This involves using imaging tests and checking your CA 19-9 levels. Early cancer identification through this cancer surveillance for sclerosing cholangitis is key to treating these cancers.
Emerging Therapies and Clinical Trials
Researchers are looking into new ways to help people with primary sclerosing cholangitis (PSC). They’re exploring new drugs and treatments. This means the field of new treatments for sclerosing cholangitis is growing fast.
By joining clinical trials for sclerosing cholangitis, you can try these new treatments. You also help improve care for this liver disease. These trials test the safety and impact of different options like curcumin, cilofexor, and more.
Ongoing work is also creating models to better understand PSC. This includes tests with biliary cell organoids. They compare how genes in PSC and non-PSC patients differ. Studies look at how certain drugs and natural medicines help the liver and slow disease.
Keeping up with clinical trials for sclerosing cholangitis and talking to your doctors is important. This keeps you involved in finding new treatment paths. Together, we’re moving towards better and personalized care for PSC patients.
Multidisciplinary Approach and Patient Education
Treating primary sclerosing cholangitis (PSC) involves many doctors working together. Experts from fields like hepatology, gastroenterology, and surgery join forces. This team approach makes sure every part of your care is looked after, from symptoms to treatment.
Educating patients about PSC is key. You, as a PSC patient, have an important role in your care and treatment choices. Your healthcare team will educate you on PSC. They will give you the info you need to care for yourself well.
Being part of your healthcare team is vital. By working closely with your doctors, you can improve your PSC care. A tailored plan will be designed with your wants and needs in mind.
Pediatric Considerations
While mostly seen in adults, primary sclerosing cholangitis (PSC) can affect children too. Kids with this condition need special care as their symptoms and treatment can differ from adults’. So, it’s key for them to see specialists in pediatric liver diseases.
About 8.6% of kids with inflammatory bowel disease may develop sclerosing cholangitis. And for many children with PSC, there seems to be an issue with how chloride channels work. This knowledge points to the need for close monitoring and targeted treatments.
There’s a tool called the Sclerosing Cholangitis Outcomes in Pediatrics (SCOPE) Index. It can give a rough idea of how long a child might go without needing a liver transplant. Knowing this can help doctors make the best choices and families understand what to possibly expect.
ERCP is often used to diagnose and treat pediatric sclerosing cholangitis. However, this procedure can have complications in up to 24% of cases. So, selecting patients carefully and using a gentle touch during ERCP is crucial.
Transplants for kids with primary sclerosing cholangitis have a 94% success rate, as found in a study. Besides this, medicines like ursodeoxycholic acid and immunosuppressants have shown good results in managing the disease.
Recurrent Primary Sclerosing Cholangitis
Recurrent sclerosing cholangitis can happen after a liver transplant. This adds new challenges for management. Doctors need to watch closely for the disease returning. They might need to change the medicines used to lower immune responses or try other treatments.
After a liver transplant, PSC can come back in 8 to 27% of people. It usually occurs again about 4.7 years later. The effect on a patient’s life is not clear, as some studies show different results.
Studies used special models to look at how recurrent sclerosing cholangitis affects life of patient’s new liver. They found that if PSC came back, it had a very bad effect on how long the new liver lasted (Hazard Ratio – HR 6.7; and how long the patient lived (HR 2.3).
People with recurrent sclerosing cholangitis might need more than one transplant. They’re about 3.6 times more likely to need another one. Also, PSC coming back makes the liver’s chance of survival after 10 years go down by 33%.
Caring for recurrent sclerosing cholangitis post-liver transplant needs many experts. They work together to see if the disease returns and to decide on treatment. It’s a complex process that requires a team approach for better patient outcomes.
Conclusion
Treating sclerosing cholangitis successfully needs a full team approach. This includes using medicine, certain procedures, and sometimes surgeries. Knowing your treatment choices and handling any complications can help improve your outcomes. By working closely with your doctors, you can better your life. Always keep an eye on new research and take part in studies to help find better care for this liver disease.
[conclusion on sclerosing cholangitis treatment] is always improving. Even though it can be tough, working with a team of experts can make a difference. Stay alert, manage your symptoms, and join in research whenever you can. Doing this can help lead to better care for you and others with PSC, improving everyone’s well-being.
You’re not alone in dealing with PSC. Reach out to support groups and resources that are ready to guide you. With everyone working together, you can manage your condition well and live a better life.
FAQ
What is primary sclerosing cholangitis (PSC)?
Primary sclerosing cholangitis (PSC) is a liver disease caused by inflammation. It makes the bile ducts hard and narrow, leading to blockages. If not treated, it can damage the liver or cause life-threatening problems.
What are the causes and risk factors for sclerosing cholangitis?
The cause of PSC isn’t totally clear. It seems to be related to the immune system attacking the body’s bile ducts. Factors like genetics and environment can also influence its development. People with certain bowel diseases, like ulcerative colitis, are at higher risk.
How is sclerosing cholangitis diagnosed?
Doctors can use a procedure called ERCP to look inside the ducts with a camera. They also use blood tests and imaging scans to diagnose PSC.
What are the treatment options for sclerosing cholangitis?
Treating PSC involves several methods. Doctors focus on relieving symptoms, slowing down the disease, and dealing with any problems it causes. This might need medicine, procedures through an endoscope, or even a liver transplant.
How can lifestyle and complementary therapies help manage sclerosing cholangitis?
Avoiding alcohol and getting certain vaccines is important for those with PSC. Managing stress, doing yoga or meditation, and staying active can also help.
What are the potential complications and associated conditions of sclerosing cholangitis?
PSC patients are at higher risk for some cancers, like those affecting the digestive system or the bile ducts. They might also feel very tired, get sad, or have problems with their bones.
How is the prognosis and monitoring of sclerosing cholangitis managed?
The outlook for people with PSC can be different for each person. Doctors check the liver’s health and watch for cancer often. This early attention is key to keeping the disease in check.
What are the considerations for pediatric sclerosing cholangitis?
Although PSC mostly affects adults, kids can get it too. Treating children with PSC means looking at the disease in a special way. The ways to treat and what to expect over time might be different.
How is recurrent sclerosing cholangitis after liver transplantation managed?
Sometimes, PSC comes back after a liver transplant. Doctors will carefully watch for this and possibly change the patient’s medications. They might need to do more procedures to help with the problem.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.





