Sclerosing cholangitis is a liver disease that gets worse over time. It causes the bile ducts to become inflamed, harden, and scar. It is very important to know the key symptoms of sclerosing cholangitis. This knowledge helps in finding it early and treating it. Common symptoms include stomach pain, feeling tired, and yellow skin and eyes. If not caught early, it can lead to bile duct cancer and liver failure.
Table of Contents
ToggleDoctors use tests and scans to diagnose it, sometimes needing a small piece of the liver to check. Catching it soon means you can start treatment fast. This can help in easing symptoms and slowing down the progress of the disease. Recognizing these signs early is key to getting medical help. This way, you can work on a plan with your doctors to manage the disease.
What is Sclerosing Cholangitis?
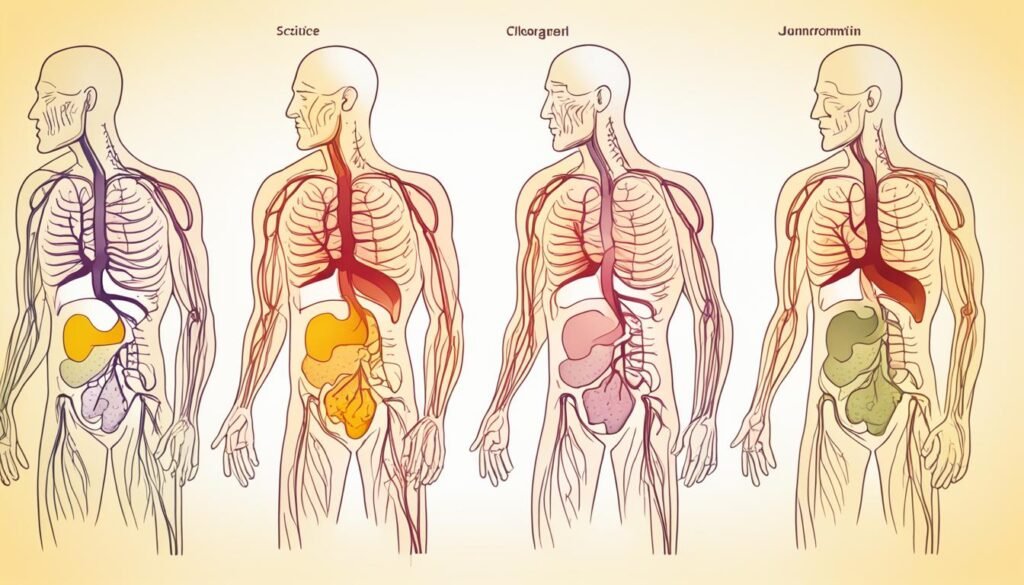
Sclerosing cholangitis is a long-term liver illness. It causes the bile ducts to get inflamed and scarred. The bile ducts are tubes that carry bile, a yellow-green fluid from your liver to the gallbladder and then to the small intestine.
With this illness, these ducts can become narrow or blocked. Because of this, bile starts to build up. This buildup can hurt your liver over time.
Primary vs Secondary Sclerosing Cholangitis
Two main types of this disease are there: primary and secondary sclerosing cholangitis. Primary sclerosing cholangitis is the more common one. Sometimes, doctors can’t find the root cause for it. Secondary sclerosing cholangitis happens when other conditions harm the bile ducts.
Difference Between Primary Biliary Cholangitis and Sclerosing Cholangitis
Primary biliary cholangitis and sclerosing cholangitis are different liver diseases. PBC focuses on the tiny ducts inside your liver. Meanwhile, SC harms both the small ducts and the ones outside the liver.
Another key difference is that PBC is tied to your immune system. SC, however, doesn’t have a fully known cause yet.

Prevalence and Risk Factors
Sclerosing cholangitis is very uncommon, with a low number of new cases yearly. The number of people alive with it is also low. These rates change from place to place. Researchers don’t know the exact cause yet. But, they have found a few things that might make someone more likely to get this disease.
Who Does Sclerosing Cholangitis Affect?
This illness mainly strikes those in their 30s and 40s. The average age when people get diagnosed is 41. It affects men more than women. Men are twice as likely to get it. People from Northern Europe are more at risk too.
Association with Inflammatory Bowel Disease
Sclerosing cholangitis often happens with inflammatory bowel disease. This includes conditions like ulcerative colitis and Crohn’s disease. Most people with sclerosing cholangitis also have one of these bowel diseases. Doctors are still studying how the two are related.

Sclerosing Cholangitis Symptoms
In the start, sclerosing cholangitis might show no symptoms. Yet, as it grows, you might notice several signs. Knowing these signs early can make a big difference and help you get treatment when needed.
Early Signs and Symptoms
Early clues of sclerosing cholangitis are important to watch for:
- Abdominal pain, especially in the right upper area
- Feeling tired and under the weather
- Your skin and eyes turning yellow (jaundice)
- Skin that feels itchy
- Issues with regular bowel movements, like diarrhea
- Fevers and getting the chills
Many people with this disease don’t feel its effects at first. Doctors often find it by accident during routine tests or scans meant for other issues.
Late Symptoms and Complications
As time goes on, sclerosing cholangitis can bring more severe problems:
- Bile duct infections that cause fever, chill, and pain
- Thinning of bones (osteoporosis), which increases fracture risk
- Chances of getting bile duct cancer, a very serious issue
- Higher risk of colon cancer, especially with inflammatory bowel disease
- Liver disease and failure, sometimes requiring a liver transplant
Spotting the early signs and understanding the possible outcomes is key. It helps in getting medical help quickly and managing the disease well with your doctors.
Diagnosis of Sclerosing Cholangitis
Diagnosing sclerosing cholangitis includes blood tests, imaging, and a liver biopsy. These tests help find the problem and plan the right treatment. This process is detailed and thorough.
Liver Function Tests
First, doctors check your liver with blood tests. They look at things like alkaline phosphatase and bilirubin. If these are high, it might mean your liver or bile ducts are harmed.
Imaging Tests for Bile Duct Evaluation
Your doctor may also order imaging tests to see inside more clearly. These tests could be MRCP, ERCP, or a CT scan. Each one helps find out if sclerosing cholangitis is there.
- Magnetic resonance cholangiopancreatography (MRCP): A special imaging method without surgery. It shows clear pictures of your ducts using powerful magnets.
- Endoscopic retrograde cholangiopancreatography (ERCP): This test uses a tiny camera to see inside your ducts. Doctors use X-rays to guide the camera.
- Computed tomography (CT) scan: A detailed X-ray test that looks at your liver and ducts. It can show what’s happening inside them.
Liver Biopsy
Sometimes, a liver biopsy is needed. It involves taking a small piece of the liver. This piece is checked in close detail to confirm sclerosing cholangitis.
All these tests together help doctors make sure of the diagnosis. With a confirmed diagnosis, they can plan the best care for you. This care aims to treat sclerosing cholangitis and any problems it might cause.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
Endoscopic retrograde cholangiopancreatography (ERCP) is key for both diagnosis and treatment in patients with sclerosis in their bile ducts. Sclerosis is a tightening or scarring found in primary sclerosing cholangitis (PSC) cases. A long, thin tube with a camera at the end goes through the mouth, the esophagus, and into the small intestine during ERCP.
This tube, called an endoscope, is joined by a small catheter. This catheter is placed into the bile ducts and shoots a special dye into them. This dye lets doctors see inside the ducts on X-ray machines.
ERCP is crucial for both finding and managing ERCP for sclerosing cholangitis. It’s the best way to look at the bile and pancreatic ducts. For people with endoscopic retrograde cholangiopancreatography sclerosing cholangitis, it’s a top choice.
This procedure helps spot problems like strictures, which are narrowings, and other irregularities.
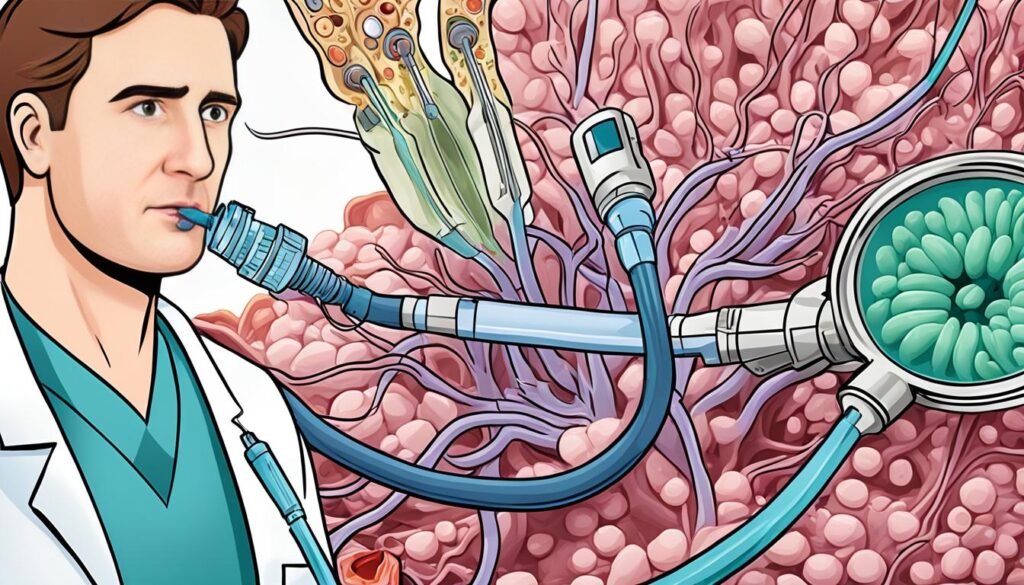
Besides its diagnostic role, ERCP can treat patients with sclerosis in their bile ducts. Doctors may put in stents to open blocked ducts. They can also remove blockages like stones and sludge. Furthermore, they sometimes take bile for tests.
ERCP is helpful but comes with risks. These include pancreatitis, which is inflammation of the pancreas, as well as bleeding, infection, and perforation. It’s critical that only trained specialists do ERCP. They must consider the dangers and benefits for each patient.
Treatment Approaches
Managing sclerosing cholangitis focuses on easing its symptoms and complications. The main goals of treatment are to make symptoms better, slow down the disease, and handle complications when they show up.
Managing Itching and Infections
Dealing with the itch (pruritus) from sclerosing cholangitis can be tough. Your doctor might suggest medicines you can get without a prescription or prescribe stronger drugs like bile acid sequestrants. Sometimes, you might need opioid antagonists or ursodeoxycholic acid (UDCA) to treat the cause of the itch.
Infections in the bile ducts, or cholangitis, are also possible. Your doctor could give you antibiotics to prevent infection risk from procedures like ERCP. This is both during the process and after.
Nutritional Support
Sclerosing cholangitis can make it hard for your body to absorb important nutrients. This often includes vitamins A, D, E, and K. You may need dietary supplements to fix your vitamin levels and improve your overall nutrition. Your doctor might also recommend medications and supplements for conditions like osteoporosis, which sclerosing cholangitis can cause.
Treating Bile Duct Blockages
A major issue with sclerosing cholangitis is the bile ducts getting blocked. This can cause bile to build up and hurt the liver more. ERCP is a common way to open up these ducts. Doctors may also use another procedure called percutaneous transhepatic cholangiography to clear blockages.
Liver Transplantation
If sclerosing cholangitis turns into cirrhosis or liver failure, a liver transplant might be the only option. This is usually for those with severe symptoms, complications, or bile duct cancer who haven’t done well with other treatments. Liver transplantation is the only known cure for sclerosing cholangitis. It means taking out the sick liver and putting in a new one.
Lifestyle and Home Remedies
While sclerosing cholangitis has no cure, managing it with lifestyle changes can help. Healthy living and the right diet choices are key to feeling better. They also support your liver’s health.
Avoiding alcohol is crucial if you have this condition. Drinking can harm your liver even more. It’s best to quit drinking or drink very little to ease the pressure on your liver.
Keeping a healthy weight matters too. Extra weight can cause more health problems. So, focus on eating well and staying active to maintain a healthy weight. Your healthcare provider can give you advice tailor-made for you.
Don’t forget to stay current on your vaccinations, especially for hepatitis A and B. Vaccines can shield your liver from more harm. They help stop the condition from worsening.
Doing regular exercise and handling stress well can lessen tiredness and other symptoms of sclerosing cholangitis. Yoga, meditation, or light exercises can make you feel better. They also help your liver stay healthy.
It’s vital to team up with your healthcare provider. They can help you make a plan that’s just right for your health and life. By dealing actively with your health through changes and home remedies, you can make a big difference in how you feel every day.
Prognosis and Monitoring
The outlook for those with sclerosing cholangitis can be quite different from person to person. This is because the disease worsens over time and can cause severe problems. The sclerosing cholangitis prognosis changes based on the state of the bile ducts, any complications, and how well you respond to treatments.
Keeping an eye on the condition is key to managing sclerosing cholangitis. Your doctor will suggest that you get blood tests regularly. This is to check your liver’s health and look for any worsening signs. They might also use imaging tests like MRCP or ERCP to monitor sclerosing cholangitis and see how your bile ducts change over time.
It’s also very important for you to watch for any drop in how you feel. Be on the lookout for more tiredness, stomach pain, or if your skin and eyes turn yellow. And if you notice anything unusual, let your healthcare provider know right away. This can help them fine-tune your treatment and keep a closer watch on your health.
Though how sclerosing cholangitis might turn out in the long run is not always clear, spotting it early and managing it well can make a big difference. If the disease is caught early, its progress can be slowed down. This can help make life better for you. Your health team will create a plan that suits your unique situation and meets your concerns.
Complications of Sclerosing Cholangitis
As sclerosing cholangitis progresses, it brings big problems. These issues can really hurt someone’s health and life. The main problems linked to this condition are cholangiocarcinoma and liver failure.
Cholangiocarcinoma (Bile Duct Cancer)
If someone has sclerosing cholangitis, they face a higher risk of cholangiocarcinoma. That’s a cancer that starts in the bile ducts. It’s a very serious condition and needs fast diagnosis and treatment.
Liver Failure
Sclerosing cholangitis causes ongoing damage and scarring in the liver. This can eventually lead to the liver failing. When this happens, the liver can’t do its important jobs anymore. Someone with liver failure might need a new liver from a transplant to survive.
Patients must watch closely for signs of these problems. It’s important to work with their healthcare team. This can help catch complications early and manage the condition better, reducing further liver harm.
Ongoing Research and Clinical Trials
Sclerosing cholangitis has a big impact, but the fight against it continues. There is ongoing research and clinical trials. These aim to help us understand and treat this rare liver disease better. Investigators are looking into many parts of the illness, such as:
- The natural history and survival analysis of primary sclerosing cholangitis, as explored in a 1989 study by Wiesner et al.
- Prognostic variables in primary sclerosing cholangitis, as indicated in a 1991 study by Farrant et al.
- The importance of cholangiography for prognosis assessment, as reported in a 2002 study by Ponsioen et al.
- The overlap syndrome of autoimmune hepatitis and primary sclerosing cholangitis, described by Gohlke et al. in 1996.
- The high prevalence of small duct primary sclerosing cholangitis among patients with overlapping autoimmune hepatitis, as found in a 2009 study by Olsson et al.
- The natural history of small-duct primary sclerosing cholangitis, as studied by Björnsson et al. in 2008.
Studies include some about ursodeoxycholic acid treatment. A trial by Beuers et al. (1992) and others by Lindor et al. and Imam et al. shared new insights. Still, high doses might not be best for everyone, as Imam et al. found in 2011.
Another option under the spotlight is 24-norursodeoxycholic acid. Fickert et al. highlighted its potential benefits in research on mice.
Liver transplant can be crucial. Works by Bjoro et al. and Brandsaeter et al. show it can help a lot.
The fight goes on through research and clinical trials. These are key in cracking this complex disease and finding better ways to help those living with it.
Coping and Support Strategies
Living with sclerosing cholangitis is tough on the body and mind. Yet, there are many ways to help yourself and your loved ones deal with this rare illness. Being proactive and using the right support can make a big difference. It can help you handle symptoms, deal with not knowing what’s ahead, and lift your spirits.
Building a strong support network is crucial for dealing with sclerosing cholangitis. Joining support groups, either face-to-face or online, links you with others. This connection can bring knowledge, emotional backup, and useful tips. Others facing the same challenges can make you feel less alone.
It’s also key to stay in touch with your medical team. This includes your gastroenterologist, hepatologist, and primary care doctor. Keep your medicine list, insurance info, and emergency contacts current. Ask questions and stand up for your needs. Staying informed about treatment updates is also smart. It helps you be part of your care plan.
Looking after yourself is vital too. Try to stay fit, eat well, and drink plenty of water. This can ease symptoms like tiredness, aches, and itches. Considering other therapies, like acupuncture or meditation, might also bring extra relief.
Being ready for more complex steps, such as a possible liver transplant, is part of the journey. Knowing about the stages of liver disease and keeping in good health is critical. This can prepare you if a transplant ever becomes an option.
Remember, coping with this illness is a process. It’s OK to be good to yourself and ask for help when you need it. Taking a thorough approach to handling your condition is important. It lets you play an active part in bettering your health and happiness.
Preparing for Your Doctor’s Appointment
Living with primary sclerosing cholangitis means staying prepared for doctor visits. Make a list of any new or worsening symptoms you’ve noticed. Include things like stomach pain, tiredness, and skin or eye color changes. Also, talk about your medical past and any drugs or lifestyle changes.
Understanding how they check and follow your condition is key. These tests might include liver function tests, MRI scans, and ERCP. Learn about these methods. It will help you have a good talk with your doctor about what to do next.
Having someone you trust with you at your appointment can be very helpful. They can remember what the doctor says, take notes, and ask questions you might forget. If you’re ready and organized, working with your doctor will be more effective. This makes getting the right care for your primary sclerosing cholangitis easier.
FAQ
What is sclerosing cholangitis?
Sclerosing cholangitis is a liver disease. It’s marked by the swelling, scarring, and narrowing of bile ducts. These ducts carry bile in and out of the liver. As a result, bile can’t flow properly, harming the liver.
What are the symptoms of sclerosing cholangitis?
At first, this disease might not show any signs. But later, it can cause belly pain, tiredness, and a yellow skin and eyes. It might lead to bile duct cancer or liver failure.
How is sclerosing cholangitis diagnosed?
Doctors diagnose it using lab tests, images, and sometimes a liver sample. They may also use a special procedure called ERCP to look closer at the bile ducts. This helps them see what’s happening inside.
What are the treatment options for sclerosing cholangitis?
Unfortunately, there’s no cure for this disease. But doctors can treat its symptoms and effects. They help with itching, fight infections, and sometimes suggest a new liver.
What is the prognosis for individuals with sclerosing cholangitis?
The outlook for those with this disease varies. It can lead to severe problems like cancer. Finding and dealing with it early can help a lot.
What are the risk factors for sclerosing cholangitis?
This disease mostly affects people between 30 and 40, more so men than women. It often shows up with gut diseases like ulcerative colitis. Knowing about this link is important.
What lifestyle and home remedies can help manage sclerosing cholangitis?
Even without a cure, there are things you can do at home. Eating well, drinking enough water, and avoiding what makes you feel worse are key. They can help you feel better.
What are the latest developments in sclerosing cholangitis research and clinical trials?
Scientists keep working to find new ways to deal with this condition. They look into different treatments and how to stop or handle the worst parts of the disease.
How can patients and their families cope with the challenges of living with sclerosing cholangitis?
This illness is tough on both the body and the mind. But there are many ways to cope. Finding support, managing stress, and teaming up with your doctors are all very helpful. They can make your care more effective and your life better.
Source Links
- https://my.clevelandclinic.org/health/diseases/23569-primary-sclerosing-cholangitis
- https://www.mayoclinic.org/diseases-conditions/primary-sclerosing-cholangitis/diagnosis-treatment/drc-20355802
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/cholangitis
- https://www.mayoclinic.org/diseases-conditions/primary-sclerosing-cholangitis/symptoms-causes/syc-20355797
- https://www.niddk.nih.gov/health-information/liver-disease/primary-sclerosing-cholangitis
- https://www.ncbi.nlm.nih.gov/books/NBK537181/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4553160/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/primary-sclerosing-cholangitis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4530326/
- https://www.niddk.nih.gov/health-information/liver-disease/primary-sclerosing-cholangitis/treatment
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/primary-sclerosing-cholangitis/primary-sclerosing-cholangitis-treatment
- https://pscpartners.org/about/treatment-options/nutrition.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4322589/
- https://pscsupport.org.uk/the-challenges-of-living-with-psc/
- https://pscpartners.org/about/the-disease/learn-about-psc.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7337345/
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.





