Have you ever felt a sharp pain in your upper belly that didn’t go away? It might be more than just gas or something you ate. It could be your pancreas sending a warning. Now, what is pancreatitis and why should you care? Pancreatitis is not just a medical term. It’s a painful condition that can quickly become dangerous if not treated right.
Table of Contents
ToggleIn this blog, we will explain what is pancreatitis, why it matters, how to spot the signs early, and what you can do to manage or even prevent it.
What is Pancreatitis?
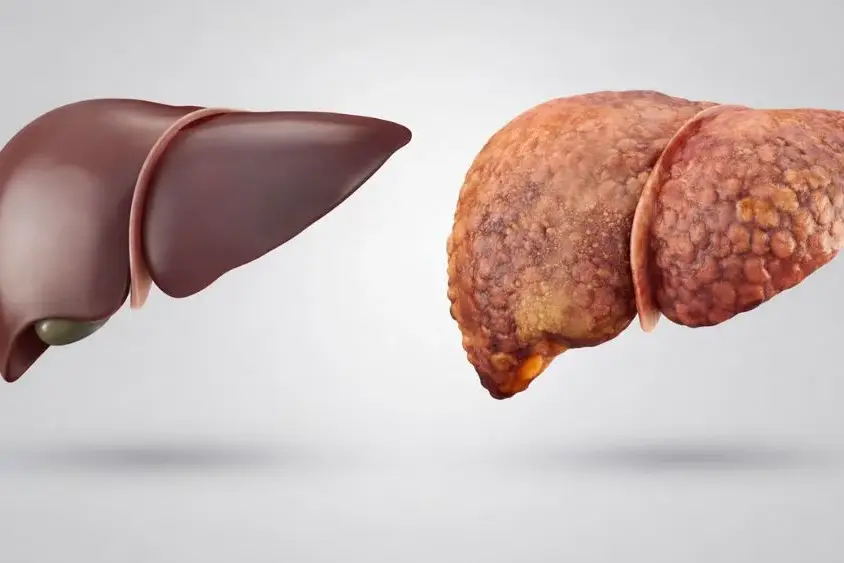
The pancreas is a small organ behind your stomach. It helps digest food and control sugar in your blood. But when it gets swollen and inflamed, we call that pancreatitis.
A healthy pancreas releases special juices called pancreatic enzymes. These enzymes break down food in the small intestine. When the pancreas is inflamed, these enzymes start working while still inside the pancreas. This causes damage to the organ itself.
So, what is pancreatitis doing to your body? It can turn a helpful organ into one that harms you. And yes, it can become life-threatening.
Stat Check: According to the NIH, over 275,000 people in the U.S. are diagnosed with pancreatitis every year.
What Are the Types of Pancreatitis and How Do They Differ?
Pancreatitis can happen suddenly or build up over time. Let’s look at both.
Acute Pancreatitis
This is a sudden inflammation of the pancreas. Symptoms show up fast and can be very painful.
- It often starts with upper belly pain.
- Pain can move to your back.
- You may also feel nauseous or throw up.
Causes include:
- Gallstones
- Heavy alcohol use
Fact: 80% of acute pancreatitis cases are linked to gallstones or alcohol – Cleveland Clinic.
Depending on how bad it is, it can be:
- Mild (goes away with rest)
- Moderate (may need hospital care)
- Severe (can harm other organs)
Chronic Pancreatitis
This is long-term swelling that keeps coming back or never fully goes away.
- It slowly damages the pancreas.
- You may lose weight or feel full early.
- It can lead to digestive issues and even diabetes.
Common causes include:
- Long-term alcohol use
- Genetic problems
So, what is pancreatitis when it doesn’t go away? Chronic pancreatitis is your answer.
What Causes Pancreatitis?
Now that we know what is pancreatitis, let’s understand why it happens.
The reasons can vary, but some triggers are common.
| Cause | Percentage Share |
|---|---|
| Gallstones | 40% |
| Heavy Alcohol Use | 30% |
| High Triglycerides | 15% |
| Medications & Trauma | 10% |
| Autoimmune/Other | 5% |
The most common pancreatitis causes are:
- Gallstones and pancreatitis: Gallstones can block the pancreatic duct and trap digestive juices.
- Alcohol-related pancreatitis: Drinking too much alcohol can damage the pancreas.
- High blood fats (triglycerides)
- Some medicines and injuries
- Autoimmune conditions
Each of these leads to pancreas swelling and enzyme buildup inside the organ.
Read: Alcohol Detox at Home: Safe and Effective Ways to Cleanse Your Body

What Are the Symptoms of Pancreatitis That You Should Never Ignore?
Recognizing the signs early helps. Knowing pancreatitis symptoms can even save your life.
Symptoms may start suddenly or slowly grow over time.
Key signs include:
- Pain in the upper belly (main pancreatitis pain location is the center or upper left area)
- Pain moving to your back
- Nausea or vomiting
- High fever
- Rapid heartbeat
- Bloating or tenderness in the belly
In acute pancreatitis, these come on fast. In chronic pancreatitis, the pain is constant and gets worse over time.
How Do Doctors Diagnose Pancreatitis?
Diagnosing pancreatitis uses tools like physical check-ups, past medical history, blood tests, and images. These methods help doctors find out the root cause of pancreatitis. They also aid in creating the right treatment plan.
Blood Tests
Doctors can check for high levels of certain enzymes in your blood. Amylase and lipase levels often spike in pancreatitis patients. These blood tests for pancreatitis are crucial for confirming the illness. They also help in tracking how it’s progressing.
Imaging Studies
To see your pancreas better, doctors might use different tests. This includes X-rays, ultrasound, CT scans, and MRI. These imaging tests for pancreatitis are key. They can show if there are any issues, like blockages or fluid build-ups. Such details are vital for proper diagnosis and care.
Endoscopic Procedures
If needed, doctors can look deeper into your ducts with special tools. ERCP and EUS are two ways they can do this. They can take samples to study or even treat problems like gallstones. These endoscopic procedures for pancreatitis offer a direct look and possibly solutions to the problem.
What is the Standard Treatment for Pancreatitis?
Dealing with acute pancreatitis means rest for your pancreas and proper care. This is often done in a hospital. There, patients get fluids through a vein, meds for pain, and sometimes antibiotics. If it’s not too serious, you might start eating or drinking light things soon. But, in more extreme cases, eating or drinking might not be allowed for a while. This helps the pancreas get better.
Hospitalization and Supportive Care
In the hospital, the main focus is on getting you hydrated and avoiding problems. You will get fluids through a vein to avoid dehydration. Oxygen might be given through your nose, and in bad cases, a machine to help you breathe might be needed.
Pain Management
Acute pancreatitis is known for causing strong belly pain. The goal is to control this pain. Doctors will give meds to help with the pain. They will adjust the dose as needed. You might also get antibiotics if there’s an infection along with the pancreatitis.
Procedures for Severe Cases
For some with acute pancreatitis, there could be more complex issues like dead tissue, infections, or fluid build-up. In these cases, special procedures might be needed. This could include using a thin, flexible tube with a camera (ERCP) to take out gallstones or drain fluid. In very severe situations, surgery might be needed to take out parts of the pancreas that are too damaged. These options are only for the most critical cases.

What Role Does Diet Play in Recovery and Prevention of Pancreatitis?
Diet is key. Knowing the right diet for pancreatitis can speed up healing and avoid flare-ups.
You need a diet that keeps your pancreas calm.
| Foods to Eat | Foods to Avoid |
| Boiled veggies | Fried foods |
| Lean meats (chicken) | Red meats |
| Low-fat dairy | Full-fat dairy |
| Whole grains | Sugar-loaded snacks |
| Plenty of water | Alcohol |
Tips for long-term health:
- Eat small meals
- Avoid alcohol completely
- Add protein from plants
Good food helps reduce pancreas swelling and supports your body’s repair process.
What Are the Possible Complications of Untreated Pancreatitis?
Ignoring what is pancreatitis can lead to serious health risks.
Common complications include:
- Pancreatic pseudocysts (fluid-filled sacs)
- Pancreatic necrosis (dead tissue)
- Diabetes
- Weight loss and malnutrition
- Higher risk of pancreatitis vs pancreatic cancer
Severe untreated pancreatitis can raise death risk. If pain worsens, go to the ER immediately.
How is pancreatitis different from pancreatic cancer?
| Feature | Pancreatitis | Pancreatic Cancer |
| Type | Inflammation | Tumor (malignant) |
| Pain Type | Sharp, may come and go | Dull, constant |
| Cause | Enzymes attacking pancreas | Cancer cells grow abnormally |
| Treatment | Lifestyle, meds, surgery | Chemo, surgery, radiation |
So, pancreatitis vs pancreatic cancer differ in many ways, but both are serious.
How Can Pancreatitis Be Prevented or Managed Long-Term?
You now know what is pancreatitis and how painful it can be. Let’s focus on avoiding future flare-ups.
Steps you can take:
- Stop alcohol use
- Control blood fats
- Maintain healthy weight
- Eat low-fat meals
- If family history exists, ask about genetic screening
You can also lower your risk of recurrent pancreatitis by following doctor’s orders and making lifestyle changes.
Acute vs. Chronic Pancreatitis: Key Differences
Pancreatitis comes in two forms: acute and chronic. Acute pancreatitis is a sudden, short-lived inflammation. It might get better by itself or need hospital care. Chronic pancreatitis is long-lasting and can hurt the pancreas permanently.
Acute Pancreatitis
Acute pancreatitis causes sharp, sudden belly pain. This pain can move to the back or chest. It’s usually because of gallstones or too much alcohol. With the right care, it often gets better in a few days or weeks.
Chronic Pancreatitis
Chronic pancreatitis brings ongoing pain that can get worse after eating. This lasting swelling causes problems like poor nutrition, pancreas scarring, and diabetes control problems. Doctors use CT scans and MRIs to find chronic pancreatitis.
Knowing how acute and chronic pancreatitis differ is key for medical teams. With this knowledge, they tailor treatments correctly. This helps patients get better care and improves their health in the long run.
Gallstone Pancreatitis: A Common Cause
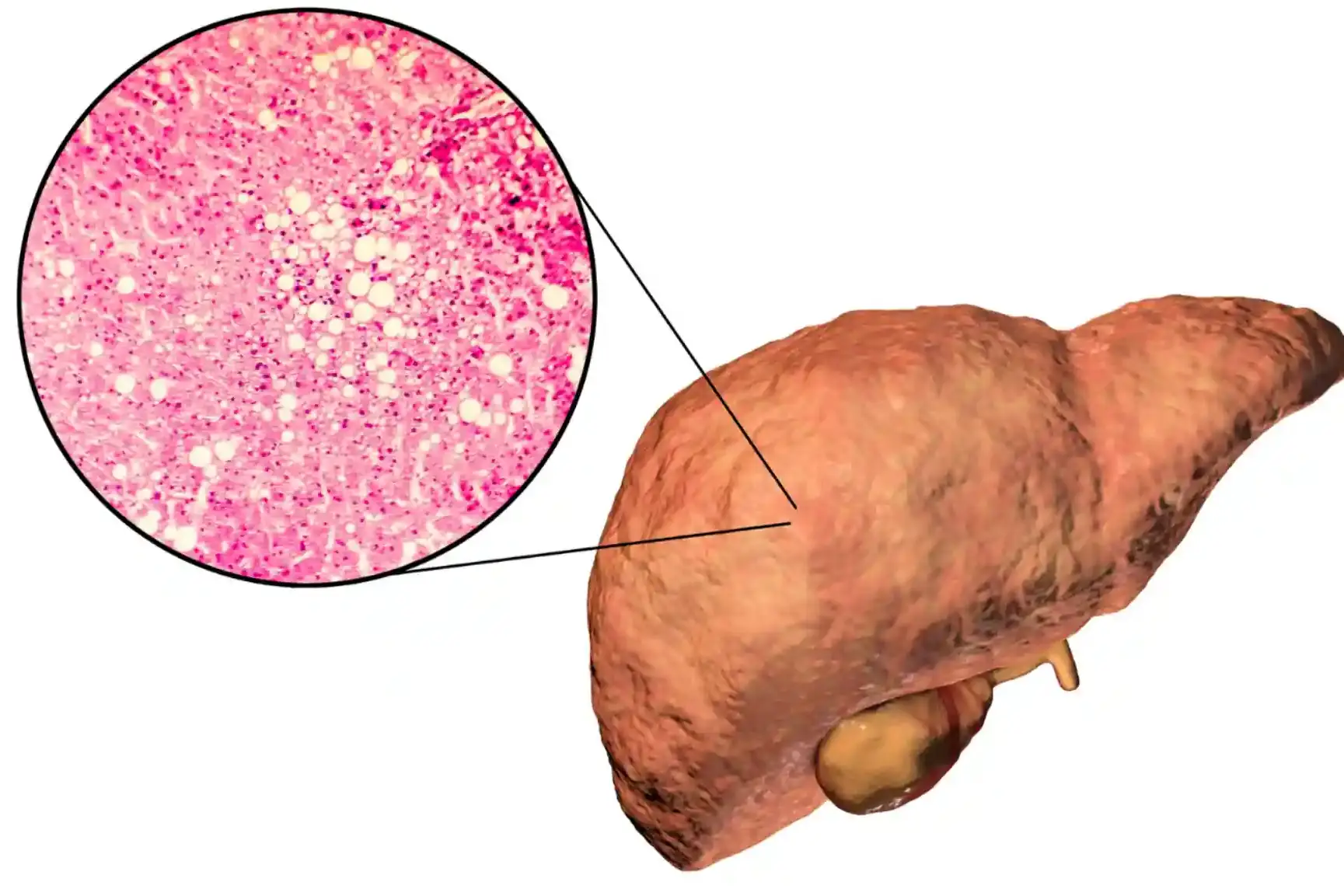
The presence of gallstones is a major reason for pancreatitis. These are hard particles in the gallbladder. They can block the bile duct. This stops pancreatic enzymes from draining properly. The enzymes then flow back into the pancreas. This causes the pancreas to become inflamed. And this is how gallstone pancreatitis starts.
Read: Case Study on GallStones Leading to Acute Pancreatitis
Gallstone Formation and Blockage
Many things can cause gallstones. This includes high cholesterol and liver disease. When a gallstone gets stuck in the bile duct, it can block the pancreatic duct. This blockage causes pancreatic enzymes to build up. They then irritate the pancreas, leading to gallstone pancreatitis.
Preventing Gallstone Pancreatitis
To avoid gallstone pancreatitis, it’s key to deal with gallstones. This can mean changing your diet, taking medicine, or having surgery to remove the gallbladder. It’s also important to stay healthy. This includes eating well and keeping a good weight. It can help lower your chance of getting gallstones and pancreatitis.
Alcohol-Induced Pancreatitis
Half of pancreatitis cases come from heavy drinking. The exact way alcohol leads to this is unclear. But, scientists think its toxic leftovers from breaking down alcohol can directly hurt the pancreas.
Drinking heavily can mess up how the pancreas works. This can lead to the organ attacking itself, causing inflammation.
Mechanisms of Alcohol-Related Damage
Alcohol abuse is behind a big chunk of pancreatitis cases. Between 17% and 25% of all sudden pancreas problems come from drinking too much. And, chronic pancreatitis is caused by alcohol in 40% to 70% of cases.
People who drink a lot and smoke have a higher risk. They could get acute pancreatitis, a sudden and severe form of the disease.
Reducing Alcohol Consumption
To avoid this, heavy drinkers should cut down or stop. Getting help to quit alcohol is a key part of treating pancreatitis. It helps avoid the disease coming back.
Also, quick diagnosis and the right treatment are vital. This includes things like fluid therapy and managing pain. It’s all part of looking after someone with alcohol-related pancreatitis.

When to Take Action: Protect Your Pancreas Today
Now you know what is pancreatitis, its signs, causes, and how to take care of yourself. Don’t wait for symptoms to worsen. Early help makes a big difference.
If you’re having belly pain, nausea, or other signs, reach out for help. Book a consultation with Dr. Nivedita Pandey today.
Dr. Nivedita Pandey, MBBS, Diplomate, American Board (Internal Medicine & Gastroenterology), is a U.S.-trained, board-certified Senior Gastroenterologist and Hepatologist. She is an expert in providing personalised pancreatitis treatment.
Take your gut health seriously. And if you or a loved one ever wonders what is pancreatitis, now you know where to turn.
FAQ
What is pancreatitis?
Pancreatitis is when the pancreas becomes inflamed. The pancreas is a gland behind the stomach. It helps with digestion and regulates blood sugar. This condition can be acute, meaning it comes on suddenly. Or it can be chronic, lasting a long time and possibly causing damage.
What are the main causes of pancreatitis?
The top causes of pancreatitis are gallstones and too much alcohol. They make the pancreas’ digestive enzymes hurt the tissue. This process causes inflammation. Other causes include some drugs, high blood fats or calcium, infections, injuries, and genetics.
What are the symptoms of pancreatitis?
The key symptom is intense stomach pain. This pain can spread to the back or chest. In acute cases, the pain is sudden and sharp. With chronic pancreatitis, the pain might be regular but not as intense. People might also feel sick, vomit, have a fever, and feel sore in their stomach. As chronic pancreatitis gets worse, digestion problems might start. This includes feeling bloated, losing weight, and having greasy stools.
What are the risk factors for developing pancreatitis?
Some factors raise the risk of getting pancreatitis. These include heavy drinking, smoking, being obese, having diabetes, and if it runs in the family. Especially, heavy drinkers and smokers are at a much higher risk.
How is pancreatitis diagnosed?
Doctors use physical exams, your medical history, blood tests, and imaging to diagnose pancreatitis. Blood tests check the levels of certain enzymes. These are often high if you have pancreatitis. Imaging like X-rays and scans help doctors see the pancreas and any issues clearly.
How is acute pancreatitis treated?
Treating acute pancreatitis involves two main steps: resting the pancreas and supportive care. This means staying in the hospital for IV fluids, pain meds, and antibiotics if needed. If the case is not severe, you might start a clear liquid or low-fat diet after the pain is gone. Severe cases might need procedures to take out gallstones or drain fluids.
How is chronic pancreatitis managed?
For chronic pancreatitis, lifestyle changes, medications, and sometimes surgery are needed. Quitting alcohol and smoking is key to improving. Doctors might give enzyme supplements to aid digestion and prevent malnutrition. There are also many ways to manage pain, from medicines to alternative therapies.
What are the potential complications of pancreatitis?
Complications of pancreatitis can be serious. They include pseudocysts, bad digestion, malnutrition, diabetes, and a higher chance of pancreatic cancer.
How can pancreatitis be prevented?
To avoid pancreatitis, limit alcohol, keep a healthy weight, and stop smoking. Taking these steps can reduce your risk a lot.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.