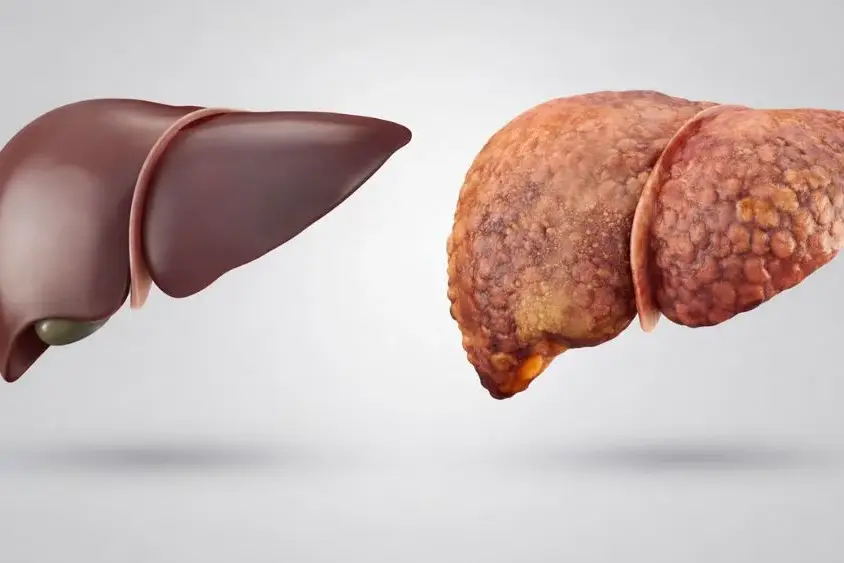
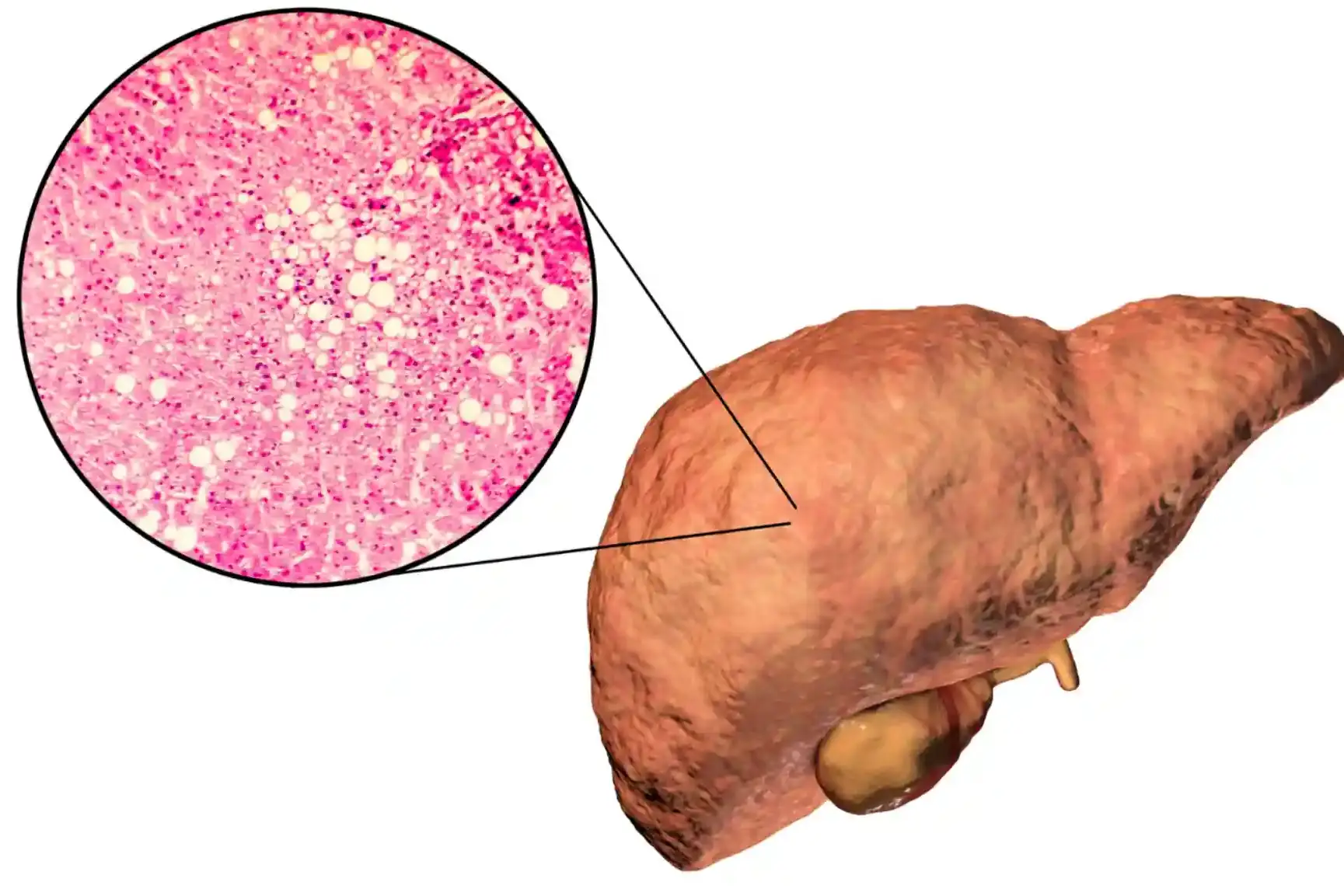
Fatty liver disease, or hepatic steatosis, is when too much fat builds up in the liver. This can hurt the liver’s function and cause problems if not treated. There are two main types: Non Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD).
Table of Contents
ToggleNAFLD is more common and linked to obesity and insulin resistance. It can change from simple fatty liver to non-alcoholic steatohepatitis (NASH). NASH can damage liver cells and lead to cirrhosis and liver failure.
Dr. Nivedita Pandey is an expert in treating liver steatosis. This article will look at treatments for fatty liver disease. We’ll cover lifestyle changes, medical treatments, and new therapies. Knowing about these can help you improve your liver health and stop the disease from getting worse.
Understanding Fatty Liver Disease
Fatty liver disease, also known as hepatic steatosis, is when fat builds up in the liver. It comes in two types: Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). Knowing about these types is key to managing and treating the disease.
Definition and Types of Fatty Liver Disease
NAFLD is more common, affecting about 1 in 3 adults in the U.S. It’s linked to obesity, insulin resistance, and metabolic syndrome. NAFLD can be simple fatty liver or non-alcoholic steatohepatitis (NASH), which causes inflammation and damage.
NASH can lead to cirrhosis and liver failure. AFLD, caused by too much alcohol, affects about 5% of Americans. It can also cause liver problems similar to NAFLD.
Risk Factors and Causes
Many things can increase your risk of fatty liver disease. These include obesity, type 2 diabetes, and metabolic syndrome. High cholesterol, certain medications, and a poor diet also play a role.
A sedentary lifestyle, hypothyroidism, sleep apnea, and polycystic ovarian syndrome (PCOS) are other risk factors. About 20% of people with NAFLD develop NASH, leading to severe liver damage.

Fatty liver disease isn’t just for adults. About 10% of children in the U.S. have NAFLD. It’s more common in older kids, Hispanic, and Asian American children. Boys are also more likely to have it.
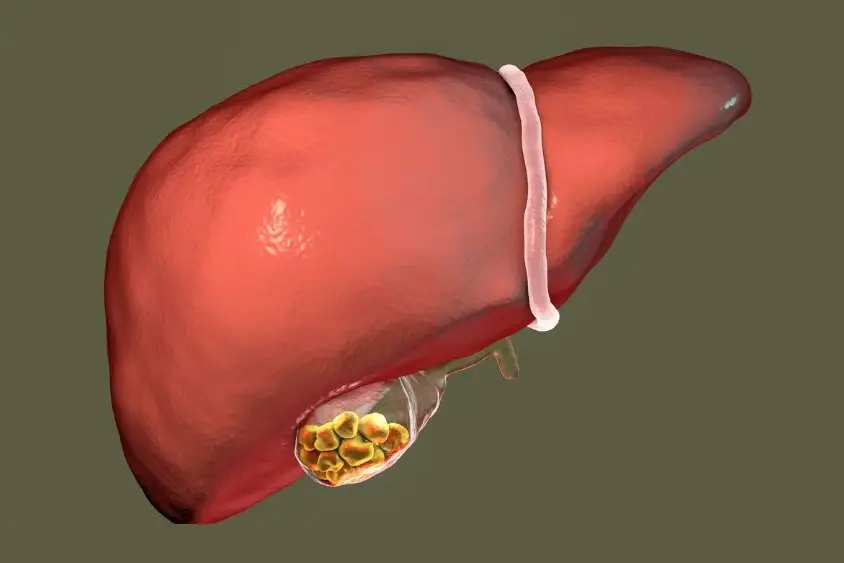
Diagnosis of Fatty Liver Disease
Diagnosing fatty liver disease takes a few steps. We’ll look at each step in the process.
Blood Tests for Liver Function
Blood tests are the first step. They check liver enzymes like ALT and AST. These tests show if the liver is healthy.
Imaging Techniques for Fatty Liver Detection
Imaging is key in diagnosing fatty liver. An ultrasound is often the first test. CT scans and MRI give more details.
Liver Biopsy: Confirming the Diagnosis
A liver biopsy might be needed. It takes a small liver sample for analysis. This helps find the disease’s severity and type.
Healthcare uses blood tests, imaging, and sometimes a biopsy. This way, they can find fatty liver disease and plan treatment.
Lifestyle Modifications for Steatosis of Liver Treatment
Making lifestyle changes is often the first step in treating fatty liver disease. Simple diet and exercise changes can greatly improve your liver health. This can also lower the risk of serious problems.
Weight Loss and Dietary Changes
Getting to a healthy weight is key for those with fatty liver disease. Losing just 5-10% of your body weight can greatly reduce liver fat and inflammation. This might even reverse liver damage.
The Mediterranean diet is a good choice. It includes fish, fruits, whole grains, nuts, olive oil, veggies, avocados, and legumes. Adding foods rich in omega-3 fatty acids, monounsaturated fats, and antioxidants also helps liver health.
Exercise and Physical Activity
Regular exercise is vital for managing fatty liver disease. Aim for aerobic exercise for 30-60 minutes daily, along with strength training. This combo can help lower liver fat and inflammation.
Brisk walking, jogging, swimming, and cycling are great options. They are all good for your liver.
Managing Comorbidities
Conditions like diabetes, high blood pressure, and high cholesterol can worsen fatty liver disease. It’s important to manage these conditions through lifestyle changes, medication, and regular doctor visits. This helps keep your liver healthy.

By changing your lifestyle, you can actively treat your fatty liver disease. This can also lower the risk of more serious problems. Talk to a skilled hepatologist to create a treatment plan that fits your needs and goals.
Medical Interventions for Fatty Liver Disease
Changing your lifestyle is key to treating fatty liver disease. But, sometimes doctors might give you medicine to help. Resmetirom, or Rezdiffra, is a special drug for non-alcoholic fatty liver disease (NAFLD). It helps lower liver fat in people with non-alcoholic steatohepatitis (NASH) and severe scarring.
Doctors are also looking into new treatments for fatty liver disease. These new therapies aim to fight inflammation and improve how your body uses insulin. The goal is to find better ways to treat this condition.
Approved Medications and Emerging Therapies
- Resmetirom (Rezdiffra): The only FDA-approved medication for NAFLD, which can help reduce liver fat in individuals with NASH and severe scarring.
- Emerging Therapies: Scientists are exploring new treatments that target different aspects of fatty liver disease, such as reducing inflammation and improving insulin sensitivity.
Right now, there are no other drugs approved for long-term NAFLD care. But, researchers keep working to find better treatments. They want to help manage this complex condition along with lifestyle changes.

Steatosis of Liver Treatment: Role of Vitamin E and Antioxidants
Researchers are looking at vitamin E and antioxidants for fatty liver disease treatment. Many studies show vitamin E supplements help those with non-alcoholic fatty liver disease (NAFLD). This is especially true for those without type 2 diabetes.
Vitamin E can reduce liver inflammation and oxidative stress. These are key factors in NAFLD. Studies suggest it can also help prevent non-alcoholic steatohepatitis (NASH), a more serious disease.
Other antioxidants are also being studied for fatty liver treatment. Antioxidant enzymes show different patterns in NAFLD stages. This means a targeted antioxidant therapy might be helpful.
Even with promising results, more research is needed. Healthcare providers and patients should talk about the benefits and risks of these supplements. This is for NAFLD treatment plans.
Vitamin E and antioxidants may help manage NAFLD by tackling oxidative stress and inflammation. As research grows, patients and doctors can make better choices. This includes using these natural therapies in liver disease treatment.
Managing Complications of Advanced Fatty Liver Disease
Fatty liver disease can get worse and lead to serious problems. If it turns into liver cirrhosis, patients face big challenges. These include portal hypertension, liver failure, and a higher risk of liver cancer.
Liver Cirrhosis and Its Challenges
Liver cirrhosis is a serious problem from advanced fatty liver disease. It happens when the liver gets badly scarred and can’t work right. People with cirrhosis might feel sick in many ways.
- Portal hypertension can cause swelling in the esophageal veins and a risk of bleeding.
- Liver failure means the damaged liver can’t do its important jobs.
- There’s a higher chance of getting liver cancer, called hepatocellular carcinoma.
Liver Transplantation: A Last Resort
In very bad cases, a liver transplant might be the only choice left. But, the main goal is to stop the disease from getting worse. This is done by changing lifestyle and sometimes using medicine.
By fixing the causes of fatty liver disease, like obesity and diabetes, we can avoid cirrhosis. This means fewer people will need a liver transplant.
An Integrative Approach to NAFLD Management
Managing nonalcoholic fatty liver disease (NAFLD) needs teamwork. Hepatologists, family doctors, and dietitians work together. They create a plan that fits each patient’s needs.
Collaboration Between Healthcare Providers
Healthcare teams tackle NAFLD’s many challenges. Hepatologists focus on liver health. Family doctors manage the patient’s overall health.
Dietitians and fitness experts help with healthy eating and exercise. These are key for NAFLD care.
Patient Education and Support
Teaching patients about NAFLD is vital. They must know about their condition and how to manage it. The healthcare team helps set goals and encourages patients.
This team effort improves NAFLD outcomes. It empowers patients and ensures they get the care they need. This approach helps manage this growing health issue.
Prevention Strategies for Fatty Liver Disease
Fatty liver disease affects millions in the U.S. It’s important to prevent it to avoid serious liver problems. Public health efforts and lifestyle advice are key in fighting this issue.
Public Health Initiatives
Working with schools and local groups can help spread the word. It’s about teaching people to eat right and stay active. This helps keep communities healthy.
- Educate the public on the risks of fatty liver disease and the importance of preventive measures.
- Develop programs that provide access to nutritious foods and opportunities for regular exercise.
- Partner with healthcare providers to integrate fatty liver disease prevention into routine check-ups and screenings.
Lifestyle Counseling
Doctors and nurses are vital in preventing fatty liver disease. They teach patients about healthy eating and exercise. This helps people lower their risk of getting this condition.
- Encourage patients to adopt a Mediterranean-style diet, which has been shown to improve liver health and reduce the risk of related complications.
- Recommend regular physical activity, such as brisk walking, swimming, or cycling, to promote weight management and overall well-being.
- Provide guidance on managing comorbidities, such as diabetes and hypertension, as they are strongly associated with fatty liver disease.
By using all these prevention methods, we can make a big difference. We can help reduce fatty liver disease and improve public health.
Conclusion
Fatty liver disease is a big health problem. It includes NAFLD and AFLD. Doctors need to work together to treat and prevent it.
They can do this by understanding the disease and its risks. They also need to know how to diagnose it. This way, they can make plans that fit each patient’s needs.
Changing your lifestyle is key to treating fatty liver disease. This means losing weight, eating better, and being more active. Studies show these changes work well.
Doctors can also use medicine and supplements like vitamin E to help. But, they must also deal with serious problems like cirrhosis. Sometimes, a liver transplant is needed.
To fight fatty liver disease, we need everyone’s help. This includes doctors, public health groups, and educating patients. The research shows we need a strong plan to tackle this disease and help patients get better.
FAQ
What is fatty liver disease?
Fatty liver disease is when too much fat builds up in the liver. There are two main types: Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). NAFLD is more common and linked to obesity and diabetes.
What are the risk factors for fatty liver disease?
Risk factors include obesity, diabetes, and metabolic syndrome. High cholesterol, certain meds, and a bad diet also increase risk. A sedentary lifestyle, hypothyroidism, sleep apnea, and PCOS are other factors.
How is fatty liver disease diagnosed?
Doctors use blood tests, imaging, and sometimes a liver biopsy to diagnose. Blood tests check liver enzymes. Imaging like ultrasound can spot fatty liver. A biopsy confirms the diagnosis and assesses damage.
What are the treatment options for fatty liver disease?
Treatment focuses on lifestyle changes. Losing weight, cutting alcohol, and managing diabetes are key. Medications like Resmetirom may also be used.
Can vitamin E and other antioxidants help with fatty liver disease?
Vitamin E may help those with NAFLD, especially without diabetes. It reduces liver inflammation and oxidative stress.
What happens if fatty liver disease progresses to cirrhosis?
Cirrhosis is a severe stage. It can lead to liver failure and cancer risk. In severe cases, a liver transplant may be needed.
How can healthcare providers help manage fatty liver disease?
Managing fatty liver disease requires teamwork. Hepatologists, family doctors, and dietitians work together. Patient education is key for success.
What can be done to prevent the development of fatty liver disease?
Preventing fatty liver disease is important. Public health initiatives promote healthy living. Healthcare providers should counsel on diet and exercise.
Source Links
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.