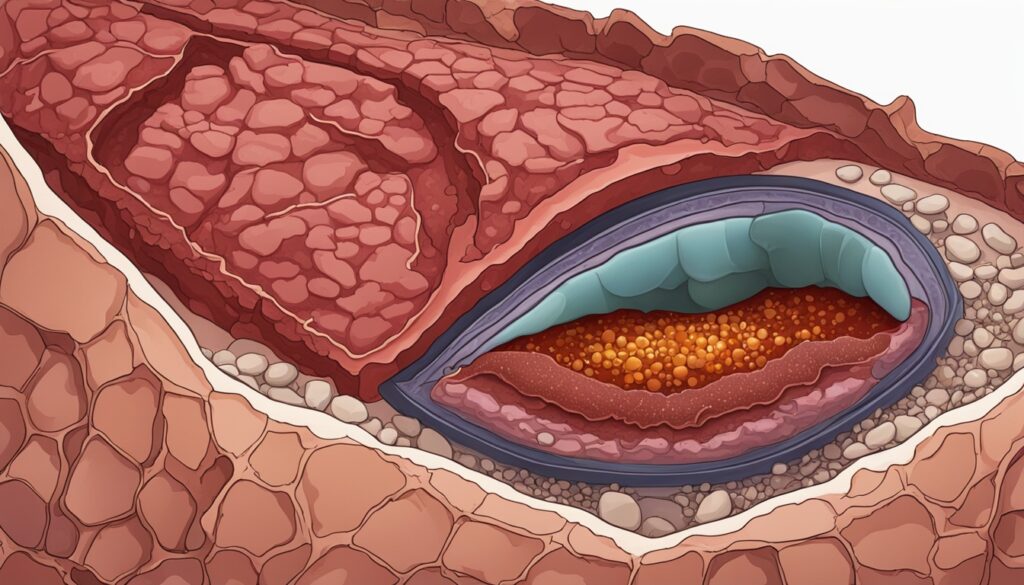
Have you ever wondered why your liver might be storing fat, even when you’re not drinking alcohol? If you’re dealing with hemochromatosis, a condition where your body absorbs too much iron, that extra iron may be silently damaging your liver. One big concern is: can hemochromatosis cause a fatty liver?
Table of Contents
ToggleThe answer is yes, and the connection is deeper than most people realize. In this guide, you’ll learn how hemochromatosis affects your liver, why fat builds up, and most importantly how you can treat and reverse it.
What is Hemochromatosis?
Hemochromatosis is a genetic disorder where your body absorbs too much iron from your diet.
- It’s often called an iron metabolism disorder.
- Too much iron can act like a poison in the body.
- Over 1 in 200 people of European descent may have hereditary hemochromatosis.
This extra iron overloads the liver, leading to oxidative stress in liver cells, which makes the liver more vulnerable to damage.
Over time, this excess iron builds up in various organs, especially the liver, leading to inflammation, scarring, and even fatty liver disease
Definition and Overview
Primary hemochromatosis comes from changes in a gene called HFE. This gene helps control the iron the body takes in. There are known genetic changes, like C282Y and H63D, linked to primary hemochromatosis. Secondary hemochromatosis is caused by other health issues that raise iron levels.
Organs affected:
- Liver
- Pancreas
- Heart
- Joint pains
- Skin
- Pituitary gland
This overload can slowly damage cells, trigger oxidative stress, and set the stage for nonalcoholic fatty liver disease (NAFLD).
Types of Hemochromatosis
The main cause of hemochromatosis is genetic. It links back to changes in the HFE gene. If someone gets specific mutations from both parents, they are more likely to get hemochromatosis. Other risks include family history, some backgrounds, and too much iron in the diet.
| Type | Description |
|---|---|
| Hereditary Hemochromatosis (Primary) | Caused by gene mutations (usually HFE gene). Found in families. |
| Secondary Hemochromatosis | Caused by conditions like anemia, frequent blood transfusions, or chronic liver disease. |
Causes and Risk Factors
Causes of hemochromatosis by genetic factors. Key genetic changes in the HFE gene play a big role. If a person gets specific mutations from both parents, their risk increases. Other things like family history, certain backgrounds, and too much iron in the diet raise the risk too.
Read: Can Hemochromatosis Cause High Blood Pressure? Exploring the Link
Symptoms You Shouldn’t Ignore
Wondering if your liver is already affected? Watch for these early warning signs of NAFLD due to hemochromatosis:
- Fatigue and weakness
- Abdominal pain (especially upper right side)
- Unexplained weight loss
- Yellowing of eyes or skin (jaundice)
- Itchy skin
- Low appetite
Hemochromatosis and Liver Disease
Hemochromatosis is when too much iron builds up in the liver. This can cause many liver issues like inflammation and cirrhosis. The extra iron damages liver cells and causes other problems.
Iron buildup in the liver can cause many issues. It damages liver cells and leads to diseases like inflammation and cirrhosis. This can also cause problems such as fatty liver disease and liver cancer.
Iron Overload and Liver Damage
Too much iron in the liver harms it in many ways. This includes causing inflammation, fibrosis, and cirrhosis. It disrupts how the liver works, leading to other issues like fatty liver disease and cancer.
Prevalence of Liver Complications
Liver complications from hemochromatosis and how to manage them. Up to half of them might get liver damage without treatment. Many might get cirrhosis or liver cancer if not treated on time.
The seriousness of liver issues varies. It depends on the amount of iron in the liver and other health conditions. Early diagnosis and treatment are crucial.
Can Hemochromatosis Cause a Fatty Liver?
The iron overload in hemochromatosis doesn’t just sit harmlessly. It triggers inflammation, damages liver cells, and impairs metabolism, which causes fat deposits to form in your liver, even if you don’t drink alcohol.
- Inflammation + iron = liver stress
- Damaged liver = impaired fat metabolism
- Impaired metabolism = fatty liver
A 2023 BMC Gastroenterology study showed that up to 24.2% of people with hereditary hemochromatosis (HFE C282Y/C282Y mutation) also had fatty liver.
Key Risk Factors:
| Risk Factor | Description |
|---|---|
| High serum ferritin (SF) | > 1100 µg/L in NAFLD patients vs. ~567 µg/L in non-NAFLD |
| Elevated liver enzymes (ALT/AST) | Suggests ongoing liver inflammation |
| Type 2 diabetes | Strong link with NAFLD in iron-overloaded individuals |
Genetic Factors and Screening
Hemochromatosis is mainly caused by problems in the HFE gene. This gene controls how our body deals with iron. The C282Y and H63D mutations in this gene are linked to hemochromatosis. People who get these mutations from both parents are at the highest risk.
HFE Gene Mutations
Studies show the C282Y and H63D mutations happen a lot in the U.S. population. People with two H63D mutations often have too much iron. Having both C282Y and H63D mutations can also mean you are more likely to get hemochromatosis.
Importance of Early Screening
It’s vital to find hemochromatosis early to stop serious issues like liver damage or heart disease. Testing is key for those with a family history or of Northern European descent. It helps catch the disease early, making treatment more effective. Genetic tests are also great for spotting HFE mutations.
| Test Type | What It Detects |
|---|---|
| Blood tests | High ferritin, high transferrin saturation |
| Liver enzymes (ALT/AST) | Liver cell injury |
| Imaging (ultrasound, CT, FibroScan) | Fat accumulation, fibrosis |
| Liver biopsy | Confirms steatosis or fibrosis |
| Genetic testing | Checks for HFE mutations like C282Y, H63D |
Treatment and Management
The Treatment options for hemochromatosis is to lower the body’s too much iron. This is usually done through phlebotomy, which is like bloodletting. It means taking out a bit of blood regularly. This lowers the iron in the body. Changing your diet is also key. It’s important to eat less food high in iron. Sometimes, the doctor might also give you medicines. These drugs help get rid of the extra iron.
Non-Surgical Treatments
These are the first-line options and often the most effective.
Phlebotomy (Blood Removal)
Phlebotomy is a big part of treating hemochromatosis. It helps take down your iron levels in a safe way. You might go in for these blood-removal sessions once or twice a week. You keep going until your iron levels go back to normal.
Medications for Iron Overload
Sometimes, your doctor may also give you medicines to remove the extra iron. These are called iron chelators. They help with taking out iron from your body. Common ones include deferasirox and deferiprone. These drugs are useful if you can’t do phlebotomy often or if you have a lot of iron overload.
| Treatment | What It Does |
|---|---|
| Phlebotomy | Removes blood to reduce iron load (like donating blood) |
| Chelation therapy | Uses medications like deferoxamine to bind and eliminate iron |
| Statins | Help lower cholesterol, may benefit liver fat |
| Insulin sensitizers | Used in diabetic patients to improve liver fat metabolism |
| Weight loss | Losing 5–10% of body weight can dramatically reduce liver fat |
Lifestyle Changes That Help:
- Eat a low-iron, anti-inflammatory diet
- Avoid red meat, alcohol, and high-fructose corn syrup
- Exercise at least 30 minutes/day
- Quit smoking (it worsens liver disease)
Home Remedies & Natural Strategies
These can be used alongside medical treatment to boost liver healing.
Dietary Modifications
Changing what you eat is crucial too. You’re told to eat less iron-rich food. For example, less red meat, fortified cereals, and some seafoods. Rather, focus on foods low in heme iron. This kind of iron is easily soaked up by the body.
By changing your diet and getting regular phlebotomy, it’s easier to lower your iron levels. This also lowers the risks of problems linked to too much iron.
Surgical Interventions (Only for Advanced Liver Damage)
When liver damage reaches cirrhosis or liver failure, more intensive measures are required.
| Surgical Treatment | Description |
|---|---|
| Liver Transplant | Needed in cases of end-stage liver failure due to iron-induced scarring |
| Liver biopsy (diagnostic) | Helps assess degree of damage |
| Bariatric surgery | Can help with weight loss in obese individuals, which improves NAFLD—but done cautiously in iron overload cases |
Detailed Treatment Plan Based on Your Condition
| Stage | Treatment Approach |
|---|---|
| Early NAFLD + Hemochromatosis | Phlebotomy + Lifestyle change |
| Moderate Fatty Liver | Add statins, insulin sensitizers, close monitoring |
| Severe Fibrosis or Cirrhosis | Consider liver biopsy, transplant evaluation |
| Diabetes Present | Glycemic control + iron reduction crucial |
| Obese + NAFLD + Iron Overload | Weight loss (diet/exercise), avoid steatogenic meds |
Read: How to Treat Hemochromatosis: Medical and Lifestyle Approaches
Complications and Risks
If not treated, too much iron in the body can cause serious issues for people with hemochromatosis. The main problem is liver cirrhosis, which might lead to liver failure and raise the chance of liver cancer. Diabetes is also a concern because too much iron can harm the pancreas, making it hard to produce insulin.
Extra iron in the heart can cause heart failure. This is when the heart can’t pump blood well. Over time, it makes the heart muscle weaker.
Liver Cirrhosis
Liver cirrhosis is a big risk for those with hemochromatosis. It can lead to liver cancer. Signs of cirrhosis include feeling tired, losing weight, itching, liver pain, and yellow skin.
Diabetes
Too much iron might also bring on diabetes. It harms the pancreas, affecting blood sugar. Warning signs include more peeing, feeling thirsty, and being extra tired.
Heart Problems
Extra iron in the heart can damage muscles. This could lead to heart failure. Symptoms of heart failure are feeling out of breath, tired, and swelling in the legs, ankles, or feet.
Lifestyle Factors and Prevention
Genes are vital in hemochromatosis development. But choices in life also matter. They affect how the disease moves and responds to treatment. Tips on drinking, eating, and moving can really make a difference. They help those with hemochromatosis stay in control and reduce problems.
Alcohol Consumption
Drinking can hurt the liver more in people with this disease. It can make liver scarring and other big issues even worse. So, cutting back or quitting drinking is usually advised. This helps protect the liver from further harm.
Diet and Exercise
Eating and moving right is key in handling hemochromatosis. It lowers the body’s total iron level. This is done by eating less iron-rich foods. And by getting enough vitamin C, which lowers how much iron your body absorbs. Exercise also improves how the body uses insulin and its overall health. This lowers the chance of getting diabetes and other issues.
Living healthy, with care in alcohol and a good diet, makes a big difference. It helps fight hemochromatosis and its health problems. This way, those with the disease can do a lot to stay well and avoid trouble.
Research and Future Directions
Ongoing research wants to know more about hemochromatosis. It looks at what causes it and how to diagnose and treat it better. Liver disease and diabetes are common problems for people with hemochromatosis.
Researchers check how both genes and the environment play a part in these problems. They also try to find new ways to help, like through new medicines. This work could make life better for those with hemochromatosis in the future.
Ongoing Studies
Scientists are digging into how too much iron, gene problems, and other factors can lead to illnesses like liver disease. They hope their work will find new ways to treat hemochromatosis.
Potential Treatments
Research is also looking at different ways to treat hemochromatosis. This includes new medicines and ways to fix gene issues. If successful, these approaches may greatly help patients with hemochromatosis.

Take Action Before It’s Too Late
Yes, hemochromatosis can cause a fatty liver, and the damage is progressive but preventable.
If you’re living with iron overload, don’t wait for symptoms to appear. Get your liver checked. Reduce your iron load. Tweak your diet. Begin early fatty liver treatment.
Dr. Nivedita Pandey, MBBS, Diplomate American Board (Internal Med & Gastroenterology), is a US-trained Senior Gastroenterologist and Hepatologist in Delhi. She is a specialist in:
- Fatty liver, NASH, cirrhosis
- Hemochromatosis, liver transplants
- Hormonal gut disorders in women
- Obesity-related gut issues
As one of South Delhi’s few female gastroenterologists, she offers a safe space for women to talk about digestive and liver health.
Click here to schedule your appointment and get your liver back on track!
FAQs
What is hemochromatosis?
Hemochromatosis is a genetic disorder that causes too much iron in the body. This iron can collect in organs like the liver. This might lead to a fatty liver.
What are the different types of hemochromatosis?
Hemochromatosis has primary and secondary types. Primary is due to a gene mutation, often in the HFE gene. Secondary comes from other conditions that make the body store too much iron.
What are the main causes and risk factors for hemochromatosis?
Genetic mutations, especially in the HFE gene, are the main cause. If someone gets the C282Y mutation from both parents, they have a higher risk. Other risks are having a family history of the disease, certain ethnic backgrounds, and a diet rich in iron.
How does hemochromatosis affect the liver?
In hemochromatosis, the liver can get too much iron. This can hurt the liver in many ways. Over time, it can cause serious liver problems like cirrhosis and liver cancer.
Can hemochromatosis cause a fatty liver?
The link between hemochromatosis and a fatty liver is being studied. Too much iron in the liver may be linked to this. But we’re still learning about how this happens.
How is hemochromatosis diagnosed?
Doctors use blood tests, gene tests, and sometimes a liver biopsy to diagnose it. Blood tests look at iron levels. Gene tests check for specific mutations
How is hemochromatosis treated?
Treating hemochromatosis means lowering the body’s iron levels. This most often involves removing blood through phlebotomy. Changing your diet and taking medications may also help. These can be part of the treatment plan.
What are the potential complications of untreated hemochromatosis?
Not treating hemochromatosis can lead to serious problems. These include liver cirrhosis, diabetes, and heart issues. It’s very important to treat it early to avoid these problems.
Can hemochromatosis cause a fatty liver even if I eat healthy?
Yes, because even with a healthy diet, your body may still absorb too much iron. Hemochromatosis isn’t about what you eat—it’s about how your body handles iron. That excess iron can settle in your liver and contribute to fat buildup.
How do I know if my fatty liver is due to iron overload?
You can’t tell just by symptoms. You’ll need specific blood tests and imaging scans. These include ferritin levels, transferrin saturation, and sometimes a liver MRI to check both iron buildup and fat in the liver.
What blood tests check for iron levels and liver health?
Your doctor may order tests like serum ferritin, transferrin saturation, and liver enzymes (ALT and AST). These help check for excess iron in your blood and signs of liver damage.
Is it dangerous to have both hemochromatosis and NAFLD?
Yes, it can be much more dangerous than having just one condition. The combination accelerates liver damage, increasing your risk for cirrhosis, liver cancer, and even liver failure if not properly managed.
Will losing weight help both hemochromatosis and fatty liver?
Yes. Weight loss helps reduce liver fat and inflammation. Just losing 5–10% of your body weight can make a significant difference in improving liver enzyme levels and reducing fat accumulation.
Can iron chelation therapy treat fatty liver too?
Not directly. Iron chelation therapy helps remove excess iron from the body, which reduces liver stress. This, in turn, can support recovery and slow down further fat-related damage to liver cells.
Are there any superfoods for people with hemochromatosis and fatty liver?
Yes, but they should be low in iron and rich in antioxidants. Foods like green tea, berries, turmeric, and broccoli help fight inflammation and support liver healing. Always consult a specialist before starting any specific diet.
How long does it take to see improvement in liver health?
If you follow treatment closely, diet, exercise, and medical therapy, you may see improvement in 6–12 months. But the timeline varies depending on the severity of your condition and how early you start treatment.
Can genetics play a role in both conditions?
Absolutely. Both hemochromatosis and fatty liver can run in families. If you have a family history of iron overload or liver disease, it’s a good idea to get tested, especially if you also have metabolic issues like obesity or diabetes.
Are liver transplants common for people with these dual conditions?
Not common but they are sometimes necessary. If both conditions are ignored for too long, the risk of advanced liver inflammation, cirrhosis, and failure increases. Early detection and treatment reduce this risk dramatically.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.





