A fistula is an abnormal connection between tissues. It can happen after surgery or due to infections. It’s also linked to ongoing health issues like inflammatory bowel disease and HS.
Table of Contents
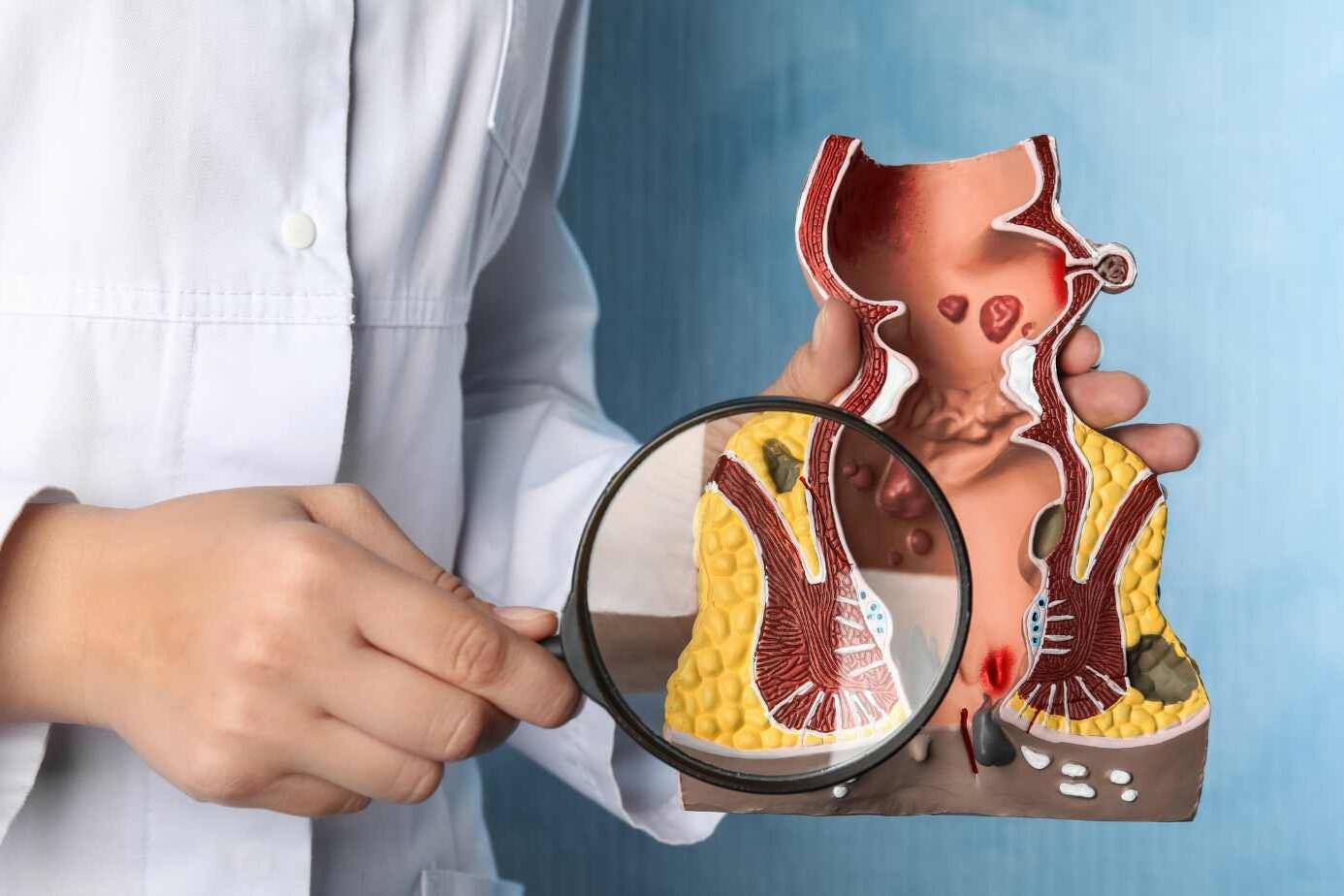
ToggleThese connections can form in many body areas. The Different Types of Fistulas are anal fistulas, enterocutaneous fistulas, enterovesical fistulas, colovaginal fistulas, and colovesical fistulas. Some, like enterocutaneous fistulas, go from the intestines to the skin. Others, like enterovesical fistulas, link the intestines to the bladder. And a few, like colovaginal fistulas, connect the colon to the vagina. Conditions such as Crohn’s disease might cause these.
Knowing about fistulas and how to treat them is very important. This helps doctors handle the situation better.
Introduction to Fistulas
A fistula is an abnormal connection. It can happen between the skin and an organ, or two organs. They come from surgeries, infections, or diseases like Crohn’s or hidradenitis suppurativa.
What is a Fistula?
A fistula is an abnormal channel. It links two surfaces, such as the skin to an organ. Causes can be surgeries gone wrong, infections, or certain diseases.
Causes of Fistula Formation
The most common causes of fistula formation include:
- Surgical complications, such as those that may occur after abdominal, pelvic, or colorectal procedures
- Infections, particularly in the gastrointestinal or urinary tract
- Chronic inflammatory conditions, like Crohn’s disease and hidradenitis suppurativa, which can lead to the development of fistulas
It’s important to know what causes fistulas. This helps doctors treat and stop them.
Anal Fistulas
Anal fistulas are very common and come from anorectal abscesses. They cause trouble with the anal sphincter muscles. It’s key to know the types for good care.
Intersphincteric Fistulas
Intersphincteric fistulas are the top kind, making up 45% of cases. They start between the anal muscles. These are quite easy to fix, with 95% success for simple cases.
Transsphincteric Fistulas
Transsphincteric fistulas are next, seen in about 30% of people. They go from one muscle to the other and can be harder to treat. Surgery like seton placement or LIFT may be needed.
Suprasphincteric Fistulas
About 20% of cases are suprasphincteric. They are above the internal muscle and tricky to fix. People could have issues with stool control after treatment.
Extrasphincteric Fistulas
The rarest type, extrasphincteric, makes up 5% of cases. They start outside the muscles and are the most challenging. They need a team of specialists for treatment.
Enterocutaneous Fistulas
Enterocutaneous fistulas are weird links between the gut and the skin. They may happen after belly or pelvic surgery. Or, they can show up in diseases like Crohn’s. These links vary in output, leading to a simple and complex kind.
The position and cause of these fistulas really change how we treat and see them. Sadly, they can be very dangerous, with some people not making it. Since most come from surgery, having skilled surgeons and careful after-surgery care matters a lot.
It’s interesting that not all fistulas are from surgery. Some come from diseases, radiation, cancer, injuries, or bad blood flow. There’s also a very risky kind that can cause serious bleeding in the gut.
Treating these fistulas needs many tools, like medicines or surgeries. It’s not easy but a team effort from doctors, nurses, and the patient can make a big difference.
types of fistula
There are several types of fistulas, such as anal and enterocutaneous fistulas. Other kinds include enterovesical, colovaginal, and colovesical. These less common types can seriously affect a person’s health and life quality.
Enterovesical Fistulas
Enterovesical fistulas create a link between the bladder and the intestines. They can appear due to Crohn’s disease or after radiation treatment. Signs might be frequent urinary infections and passing gas or stool through the urine.
Colovaginal Fistulas
Colovaginal fistulas connect the vagina to the colon or rectum. They might happen after pelvic surgeries or due to conditions like Crohn’s disease. Signs can be an unusual odor from the vagina or passing gas and stool through it.
Colovesical Fistulas
Colovesical fistulas link the bladder to the colon or rectum. Causes include past surgeries or diseases like diverticulitis. Signs might involve urinary problems, like constant infections or passing gas or stool in the urine.

Crohn’s Disease and Fistulas
Crohn’s disease, an inflammatory bowel condition, often leads to fistulas. Fistulas in Crohn’s disease can be quite complex. They’re difficult to treat effectively. The two main types of fistulas seen in Crohn’s patients are perianal and enteroenteric.
Perianal Fistulas in Crohn’s Disease
Perianal fistulas are most frequently found in Crohn’s disease. These are abnormal tunnels between the anal canal and the skin around the anus. They cause pain, discharge, and sometimes incontinence. Doctors use MRI and endoscopic ultrasound to see how severe these fistulas are.
Treatment for perianal fistulas includes medicines and surgery. Biologics help reduce drainage and speed up healing. Antibiotics like metronidazole and ciprofloxacin are crucial in managing these fistulas. Surgery options include fistulotomy and other procedures to treat severe cases.
Enteroenteric Fistulas in Crohn’s Disease
Enteroenteric fistulas are between two parts of the small intestine in Crohn’s disease. They can cause not absorbing food well, diarrhea, and losing weight. Tests like CT or MRI help find these fistulas.
Managing enteroenteric fistulas includes both medicines and surgery. Medications like biologics and immunomodulators lessen inflammation and help close the fistula. But sometimes, surgery to remove parts of the intestine may be needed for harder cases.
For any kind of fistula, it’s vital for Crohn’s disease patients to closely work with their doctors. Together, they should create a treatment plan that’s just right for them. The goal is to heal the fistula and improve the patient’s quality of life.
Diagnosis of Fistulas
Diagnosing fistulas right is key to a good treatment plan. Doctors use both check-ups and special pictures to figure them out.
Clinical Examination
The first thing in diagnosing a fistula is a detailed check-up. The doctor will look at the sore spot, touch around it, and see any leaking. They might slide a small tool, called a probe, in the sore to learn more about it.
Imaging Techniques
Your doctor might also ask for pictures to see the fistula better. These could be:
- MRI imaging – This is a painless scan that makes detailed pictures of the fistula.
- Endoscopic ultrasound – It uses sound waves and is good for checking the muscles and tissues around the fistula.
- Fistulography – This special X-ray uses a dye to show the path of the fistula.
These tools help doctors find out exactly what the problem is. This is needed to plan the right treatment.

Surgical Management of Fistulas
Sometimes, complex or recurring fistulas need surgery to heal. Common surgeries are fistulotomy, seton techniques, advancement flap procedures, and the LIFT method.
Fistulotomy
In fistulotomy, the fistula tract is cut open to heal from the inside. It’s very effective, working in about 95% of simple cases.
Seton Techniques
Seton techniques use a thread inside the fistula to spread muscle fibers. This is helpful for complex cases to lower the chance of future problems and incontinence.
Advancement Flap Procedures
With advancement flap procedures, a flap of healthy tissue is moved to cover the fistula’s opening. This method works about 70% of the time but can have a risk of hurting the sphincter muscle.
Ligation of Intersphincteric Fistula Tract (LIFT)
The LIFT procedure tightens and cuts the fistula tract, with a success rate of 75%. It also lowers the risk of muscle damage.
Non-surgical Treatments
Not everyone can or wants to have surgery for fistulas. Luckily, there are non-surgical choices. These options work well for people who can’t have surgery or prefer something less invasive. Some ways to treat fistulas without surgery are:
Fibrin Glue
Fibrin glue is injected into the fistula tract. It mixes fibrin and thrombin to seal the fistula, promoting healing. This method has worked on simple and complex fistulas, with success between 30% and 80%.
Fistula Plugs
Another choice is using fistula plugs. They’re made from collagen or other materials. Doctors place them in the fistula tract to help it heal. Studies show success rates from 30% to 70%.
Stem Cell Therapy
Stem cell therapy is a new way to approach fistulas. It uses the patient’s own stem cells, injecting them into the fistula. The goal is to grow new tissue and speed up healing. This method is still under research but is promising in some cases.
Non-surgical treatments can work for smaller or simpler fistulas. But, they might not be as reliable as surgery. They also might mean the fistula could come back. Your best option depends on your fistula, your health, and talking to a colorectal specialist. They will guide you to the right treatment for you.
Complications and Recurrence
Fistula care is tricky and may cause problems again. One big issue is losing control of the bowels (incontinence). This can really affect how a person lives. Where the fistula is and how bad it is, plus why it happened, can all lead to incontinence.
Incontinence
Incontinence often happens with fistulas near the anal area. Up to 25% of those with anorectal fistulas can face it. If the fistula breaks the anal muscles, incontinence is more likely. Quick and right treatment is key to lower this risk and have good results.
Risk Factors for Recurrence
Fistulas can come back, with rates from 30% to 80%. A study on anal fistula surgeries showed a 32% chance of coming back. Things like Crohn’s disease, surgeries that didn’t work, and how complex the fistula is can up the chance of it coming back.
Handling fistula problems and cutting the comeback chance needs a full treatment plan. This might mean doing different kinds of surgery, like fistulotomy or using a seton, or trying things without surgery, such as fibrin glue. There’s also talk about using stem cells for tough cases.
Knowing the main fistula issues, like incontinence and them coming back, helps doctors make treatments just for the patient. This makes dealing with fistulas easier on people.
Preventive Measures
Managing fistulas can be tough, but there are preventive measures that help. Good hygiene, quick infection treatment, and good nutrition are key. Also, be careful during surgery and manage diseases like Crohn’s well to cut down fistula risk.
For those at high fistula risk, like people with Crohn’s or past fistulas, watch closely and act fast. Early treatment of new symptoms can stop the fistula from getting worse. That lowers the chance of bad outcomes.
New surgeries and treatments, like stem cell therapy, are showing hope in stopping fistulas. These methods aim to heal tissues better, lower the return risk, and help patients more.
A full-on plan for preventive measures for fistulas makes a big difference. It helps cut the hardship of fistulas and betters life for those dealing with it. Regular check-ups, team work, and keeping a close eye are vital for stopping fistulas.
Conclusion
Fistulas are tricky medical problems that can come from different things, like surgery troubles and infections. It’s key to know the types of fistulas, why they happen, and how to check and treat them well. Keeping up with the new in fistula care helps doctors give the right care fast, making life better for patients.
Detecting fistulas early and treating them right for each person is super important. Doctors use check-ups and special pictures to find and name fistulas correctly. Then, they make a plan just for that patient. It might be surgery, medicine, or both.
Medicine is always getting better. New treatments like stem cell therapy and special surgeries are now out there. Knowing about these new things helps doctors give their patients the best care. This makes life easier and the problem less hard to deal with.
FAQ
What is a fistula?
A fistula is a special issue where a wrong link forms. It connects places that should not be connected. This can be from the skin to inside the body or between body parts.
What causes fistula formation?
Fistulas happen because of surgery, infections, or long-term swellings like Crohn’s disease. They can also start from infections, or other diseases.
What are the different types of anal fistulas?
Anal fistulas come in a few types. These include intersphincteric, transsphincteric, suprasphincteric, and extrasphincteric fistulas.
What is an enterocutaneous fistula?
An enterocutaneous fistula is a link between the gut and the skin. It happens after stomach or pelvis surgery. Crohn’s disease can also cause this issue.
What other types of fistulas are there?
Some other fistulas are enterovesical, colovaginal, and colovesical fistulas.
How are fistulas association with crohn s disease?
Crohn’s disease often causes fistulas. This disease makes you more likely to develop these connections.
How are fistulas diagnosed?
Doctors use a few ways to diagnose fistulas. They do exams and may use ultrasound or MRI. Sometimes, they do a test called fistulography.
What are the surgical management options for fistulas?
Surgery is a common way to treat fistulas. Doctors may do a fistulotomy, use setons, or advance flaps. They also do a procedure called LIFT.
What non-surgical treatments are available for fistulas?
Without surgery, treatments include fibrin glue, plugs, and even stem cells.
What are the potential complications and risks of recurrence with fistulas?
Fistulas might cause leaking problems or come back after treatment, especially the hard cases.
How can the development of fistulas be prevented?
To prevent fistulas, treat infections early. Use careful surgeries. Also, manage diseases like Crohn’s well.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin