Endoscopy and colonoscopy are diagnostic procedures that allow doctors to see the inside of your digestive system using a thin, flexible tube with a camera and light.
Table of Contents
ToggleIn endoscopy , the scope enters through your mouth to examine the esophagus, stomach, and upper small intestine, which helps detect ulcers, acid damage, infections, and bleeding. Colonoscopy uses a longer scope inserted through the rectum to inspect the entire colon and rectum, making it essential for finding polyps, bowel inflammation, and colon cancer.
Although both tests use similar technology, they serve different medical purposes because they examine separate digestive regions.
Difference Between Endoscopy and Colonoscopy
Endoscopy looks at the upper part of your digestive system through the mouth, while colonoscopy examines the lower digestive tract through the rectum. Doctors choose between these tests based on where your symptoms start, what organs they need to see, and which diseases they suspect. The scope path, preparation, risks, and diagnostic value change because the organs involved are not the same.
Area of The Digestive Tract Examined
Endoscopy examines the upper digestive tract. This includes the esophagus (food pipe), stomach, and duodenum, which is the first part of the small intestine. Doctors use endoscopy when symptoms start above the belly button.
A colonoscopy examines the lower digestive tract. This includes the entire colon and the rectum. Doctors rely on colonoscopy when symptoms involve bowel habits, stool changes, or lower abdominal pain.
Upper and lower digestive diseases often cause different warning signs, which is why one test cannot replace the other.
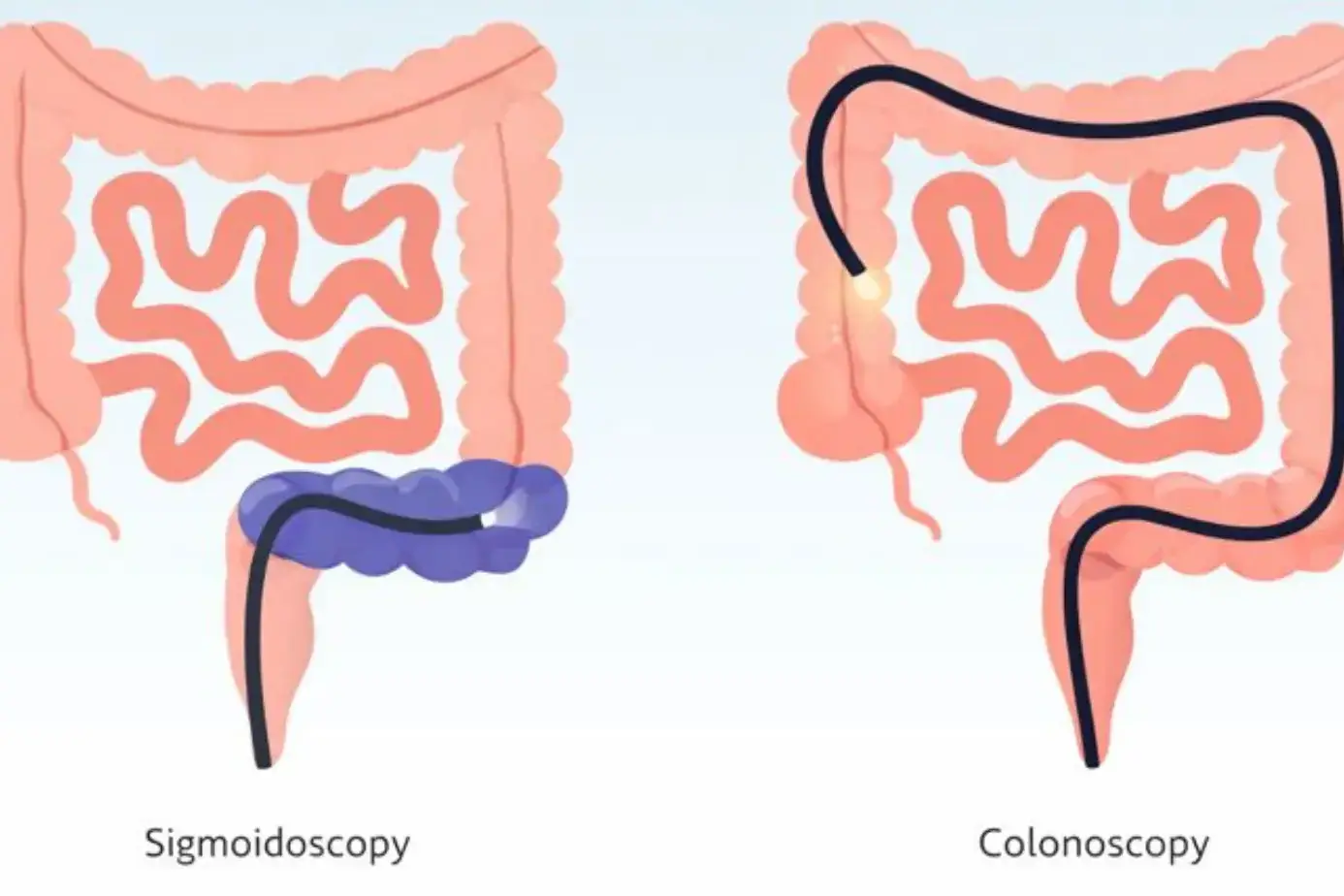
Type of Scope and Insertion Route
During endoscopy , the doctor inserts a thin, flexible tube through your mouth. The scope moves down your throat into the stomach. A small camera at the tip sends live images to a monitor.
During a colonoscopy , the scope enters through the rectum and moves through the colon. The tube is longer because the colon is longer and curved.
Both scopes are flexible and designed to reduce injury. The insertion route determines the preparation, discomfort level, and recovery experience.
Conditions Each Test Helps Diagnose
Endoscopy helps doctors find acid damage, ulcers, infections like Helicobacter pylori (a stomach bacterium), swallowing disorders, and upper digestive bleeding. It also allows tissue sampling when cancer or inflammation is suspected.
Colonoscopy helps detect colon polyps, colorectal cancer, inflammatory bowel disease, chronic bleeding, and unexplained diarrhea. It also allows doctors to remove polyps during the same procedure, which helps prevent cancer.
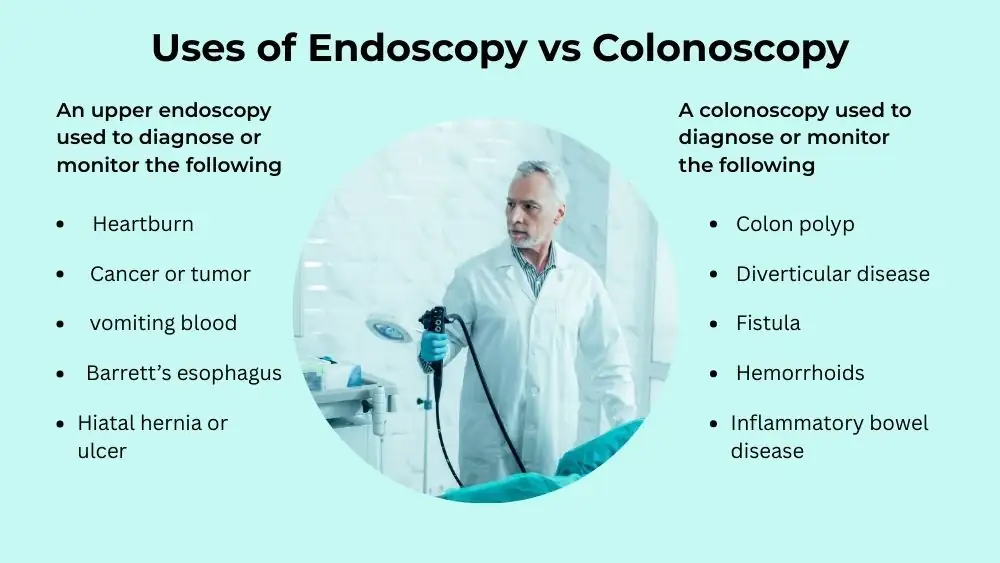
Endoscopy vs Colonoscopy Uses
Endoscopy helps identify problems in the upper digestive tract, such as acid damage, ulcers, and swallowing disorders. Colonoscopy focuses on the lower digestive tract and plays a major role in finding polyps, bowel disease, and colon cancer.
When Endoscopy Is Recommended
Doctors recommend an endoscopy when your symptoms suggest upper digestive problems. These include long-lasting heartburn, chest pain unrelated to the heart, trouble swallowing, vomiting blood, or ongoing nausea.
The uses of endoscopy also include checking stomach ulcers that do not heal, evaluating anemia with an unknown cause, and monitoring known conditions like Barrett’s esophagus. Endoscopy improves early detection of esophageal cancer in high-risk patients.
When Colonoscopy Is Recommended
Doctors recommend a colonoscopy when symptoms involve the lower digestive tract. These include blood in stool, unexplained weight loss, long-term constipation, chronic diarrhea, or sudden bowel habit changes.
The uses of colonoscopy also include routine cancer screening, usually starting at mid-adulthood, even when no symptoms exist. Colonoscopy lowers colon cancer death rates by allowing early detection and polyp removal.
Conditions Where Both Tests May Be Needed
Some conditions affect both ends of the digestive system. Severe anemia, unexplained bleeding, or long-standing inflammatory diseases may require both endoscopy and colonoscopy .
Doctors decide based on lab tests, imaging results, and symptom patterns. Doing both tests together improves diagnosis when the bleeding source remains unclear.
Endoscopy vs Colonoscopy Pain
Endoscopy usually causes brief throat pressure and mild discomfort, while colonoscopy can cause cramping or fullness due to the gas used during the test. Pain levels vary by person, but neither procedure is considered highly painful when performed correctly.
Pain Levels During Endoscopy
Most people describe endoscopy pain as mild pressure rather than sharp pain. Doctors spray a numbing medicine in your throat to reduce your gag reflex. You may feel fullness or brief discomfort when the scope passes. Most patients rate endoscopy pain as low when sedation is used. The short duration also limits discomfort.
Pain Levels During Colonoscopy
Colonoscopy pain usually comes from air or carbon dioxide used to expand the colon for better viewing. This can cause cramping or pressure during and shortly after the test.
Studies comparing patient comfort show that colonoscopy pain varies more than endoscopy pain , mainly due to bowel sensitivity and anatomy. Sedation reduces pain for most patients.
Role of Sedation in Reducing Discomfort
Sedation plays a major role in comfort for both tests. Doctors usually give light to moderate sedation through an IV. This helps you relax and reduces awareness.
Research from anesthesia studies shows sedation lowers reported endoscopy pain and colonoscopy pain without increasing complication risk in healthy patients. Some people remain awake but calm, while others remember very little afterward.
Endoscopy vs Colonoscopy Risks
Endoscopy carries a slightly lower overall risk because it examines a shorter section of the digestive tract, while colonoscopy has a higher but still rare risk due to colon length and polyp removal. Most complications are mild and temporary, and serious problems occur infrequently.
Common Risks of Endoscopy
The risks of endoscopy remain low when trained specialists perform the test. The most common issues include throat soreness, bloating, mild nausea, and temporary hoarseness. These symptoms usually fade within one day.
Bleeding can occur if doctors remove tissue samples, but this bleeding is often minor and stops on its own. Studies from clinical gastroenterology journals show that serious complications from endoscopy occur in fewer than one out of one thousand procedures.
Common Risks of Colonoscopy
The risks of colonoscopy include gas pain, abdominal cramping, and bloating after the procedure. These symptoms happen because air or carbon dioxide expands the colon during the test.
Bleeding can occur after polyp removal, especially when polyps are large. Research confirms that post-procedure bleeding usually appears within seven days and often resolves without surgery.
Rare but Serious Complications
Rare complications include perforation, which means a tear in the digestive wall. This happens more often during colonoscopy than endoscopy , mainly due to the length and shape of the colon.
Sedation reactions can also occur, especially in people with lung or heart disease. Medical guidelines stress careful monitoring to reduce these risks.
When Do You Need Endoscopy vs Colonoscopy
Symptoms Pointing Toward Upper GI Issues
You may need an endoscopy if you experience burning chest pain that does not improve with treatment, frequent vomiting, trouble swallowing, or black vomit. These symptoms often signal upper digestive damage.
Doctors also order an endoscopy when blood tests show iron deficiency without a clear cause, as upper bleeding can be hidden.
Symptoms Pointing Toward Lower GI Issues
You may need a colonoscopy if you notice blood in stool, long-term diarrhea, unexplained constipation, or sudden changes in bowel habits. upper abdominal pain that persists also raises concern. Many colon cancers cause few early symptoms, which is why screening colonoscopy matters even when you feel well.
Doctor Decision Factors
Doctors consider your age, family history, symptom duration, and previous test results. Cancer risk weighs heavily in the decision.
Colonoscopy is recommended earlier for people with a strong family history, while endoscopy depends more on symptom severity.
Procedure Time and Recovery Comparison
How Long Endoscopy Take
Endoscopy usually takes fifteen to thirty minutes. Preparation and recovery add extra time, but the procedure itself remains short. Because the scope travels a short distance, physical stress stays limited.
How Long Colonoscopy Take
Colonoscopy typically takes thirty to sixty minutes. The bowel preparation before the test requires more effort than the procedure itself. The test may take longer when doctors remove polyps or inspect suspicious areas closely.
Recovery Time and Same-Day Discharge
Both tests usually allow same-day discharge. You may feel drowsy for several hours due to sedation. Most people return to normal eating within twenty-four hours. Doctors advise avoiding driving or signing legal documents the same day.
Endoscopy vs Colonoscopy Accuracy and Detection
Conditions Best Detected by Endoscopy
Endoscopy detects ulcers, esophageal narrowing, reflux damage, stomach tumors, and upper bleeding sources with high accuracy. It also allows direct biopsies, which improve diagnosis. Endoscopy plays a key role in detecting early esophageal cancer in high-risk patients.
Conditions Best Detected by Colonoscopy
Colonoscopy remains the gold standard for detecting colon polyps and colorectal cancer. It also diagnoses inflammatory bowel diseases like ulcerative colitis. Colonoscopy prevents cancer by removing precancerous polyps during the same exam.
Role in Cancer Detection and Prevention
Colonoscopy prevents cancer more than it detects it, because polyp removal stops cancer before it forms. Endoscopy focuses more on early detection than prevention. Both tests improve survival when used correctly.
Cost and Availability Differences
Typical Cost Range for Endoscopy
Endoscopy generally costs less because it requires less time and preparation. Costs vary by location, facility type, and sedation use. Hospital-based procedures often cost more than othose in utpatient centers.
Typical Cost Range for Colonoscopy
Colonoscopy usually costs more due to longer procedure time and bowel preparation. Polyp removal and biopsy increase the cost.
Despite the higher cost, screening colonoscopy saves money long-term by preventing cancer treatment expenses.
Insurance Coverage Considerations
Most insurance plans cover endoscopy when symptoms justify it. Screening colonoscopy often receives full coverage after a certain age under preventive care rules. Coverage may differ for diagnostic procedures.
FAQs
Is Endoscopy Safer Than Colonoscopy?
Both endoscopy and colonoscopy have low complication rates when done by trained doctors. Safety depends more on your health conditions than on the procedure itself.
Which Test Is More Painful?
Most people report slightly higher colonoscopy pain due to gas pressure. Sedation keeps discomfort low for both tests in the majority of patients.
Can Both Tests Be Done on the Same Day?
Doctors can perform endoscopy and colonoscopy on the same day when medically needed. This approach reduces anesthesia exposure and recovery time.
Which Test Is Better for Acid Reflux?
Endoscopy works best for acid reflux because it directly shows esophageal damage and inflammation caused by stomach acid.
Which Test Detects Colon Cancer Better?
Colonoscopy detects colon cancer better because it views the entire colon and allows removal of pre-cancerous polyps.
Do Both Require Sedation?
Sedation is common for both tests, but not mandatory. Doctors decide based on anxiety level, health status, and procedure complexity.
How Often Should Each Test Be Repeated?
Repeat timing depends on findings. Normal colonoscopy results may last years, while endoscopy repeats depend on symptom return.
Is Colonoscopy Necessary If Endoscopy Is Normal?
Yes. A normal endoscopy does not rule out colon disease. The two tests examine different digestive areas.
Can I Eat Normally After Both Procedures?
Most people resume normal eating within hours. Doctors may suggest light meals first to reduce nausea.
Who Should Avoid These Procedures?
People with unstable heart, lung, or bleeding conditions may need special planning. Doctors evaluate risks before scheduling either test.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin