There are many bariatric surgical risks that you should keep in mind before anything else. However, knowing more about bariatric surgery is essential to avoid these bariatric surgery side effects as much as possible, with expert medical support and help.
Table of Contents
ToggleWhat is bariatric surgery?
Bariatric surgery is a term indicating a specific surgical process that helps in losing weight through changes made to the digestive systems of our bodies. The term itself may be used for indicating several types of processes including weight loss surgeries and gastric bypass surgeries alike. There are various bariatric surgery types that you should know more about. These surgeries function in various ways including lowering the amount of food that your stomach can take, lowering the ability of the body with regard to nutrient absorption or even a fusion of both these methods.
Bariatric surgery often comes in useful when it comes to quickly combating any life-threatening ailments or conditions that crop up in the case of patients. It is medically recommended and is not for everyone who is otherwise obese or overweight. This point should be kept firmly in mind.
The commonest types of surgery include the following:
- Gastric bypass surgery- This is one of the commonest bariatric surgeries. It works through a method where a minuscule pouch is made in the stomach’s upper portion, dividing it from the remaining portion. Then the first part is divided for the small intestine and the bottom part is linked to the newly-made smaller pouch within the stomach. The top portion of the divided small intestine is then linked to the small intestine’s bottom and this changes the gut hormones and food stream alike. The process restricts the food that the stomach can hold while lowering overall nutrient and calorie absorption alike.
- Sleeve gastrectomy- This is the removal of roughly 80% of the stomach with only a tube-shaped pouch or sleeve left. Hence, the stomach cannot hold food like before. It also helps in lowering the ghrelin hormone which helps with appetite regulation.
- Gastric band- The gastric band is adjustable and the process involves putting an inflatable band around the stomach’s upper portion, creating a smaller pouch over the same. Food storage is comparatively lower while patients achieve a feeling of fullness swiftly. The band reduces in size with adjustments over a period of time.
- Duodenal switch- BPD/DS has a tube-shaped pouch created in the stomach while a major part of the small intestine is also skipped. This lowers the food that the stomach may hold while ensuring fullness more swiftly. It also lowers overall nutrient absorption.
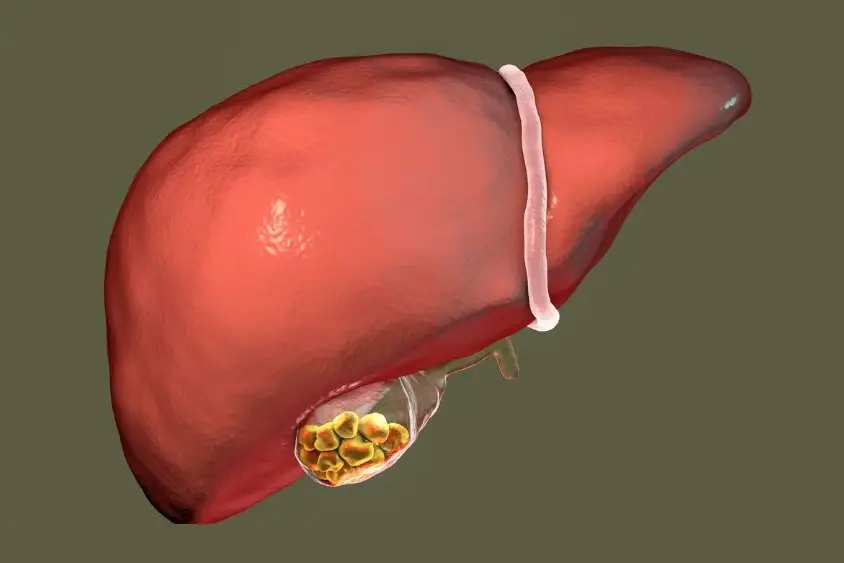
Bariatric surgery is done in case of various issues including stroke, heart disease, sleep apnea, non-alcoholic fatty liver disease, high blood pressure, Type 2 diabetes, and other life-threatening ailments.
What is the commonest complication of bariatric surgery?
Some of the risks include acid reflux, infections, inability to consume specific food items, chronic vomiting and nausea, anaesthesia-linked issues, stomach obstruction, esophageal dilation, weight gain or failure to achieve weight loss and so on. Following a medically guided bariatric surgery diet plan is always recommended in such scenarios. Other long-term risks include blood sugar dips, ulcers, hernia, obstruction of bowel movements, dumping syndrome, malnutrition, and more.
Additional risks include breakage, gallstones, leakage, internal bleeding, calorie or protein malnutrition, perforation of the intestines or stomach, pouch or bowel obstruction, separation of the skin, cardiac or pulmonary issues, spleen or organ injuries, stricture, ulceration of the stomach or intestine and also deficiencies in iron and key vitamins. Other risks include blood clots as well.
You can always lower your bariatric surgery-related side effects and complications by lowering your overall BMI (body mass index) and also increasing your exercise in consultation with your physician. You can also consider stopping your smoking habit (if you have one) in this case. You should consume alcohol with medical advice and preferably create a regular dietary plan in consultation with your physician. There are quite a few complications arising from these surgeries but proper planning (before the surgery), guidance from your doctor and following a healthy regime afterwards, will help you minimise the impact and get back to normal activities with negligible disruptions. The best course of action would be to contact Dr. Nivedita Pandey. Her specialties include gastroenterology and hepatology. With her expertise, you’ll get started on the road to a healthy lifestyle.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.