Welcome to our informative article on biliary atresia complications, covering important insights into long-term health, prevention, and management strategies. Biliary atresia is a condition that affects infants, leading to blockage and scarring of the bile ducts in the liver. If left untreated, it can have severe consequences, including liver failure and cirrhosis.
Table of Contents
ToggleBy delving into the risks associated with biliary atresia complications, we aim to provide you with valuable information that can help you navigate this condition effectively. We will explore various preventive measures and management strategies that can significantly impact the long-term health outcomes of individuals with biliary atresia.
What is Biliary Atresia?
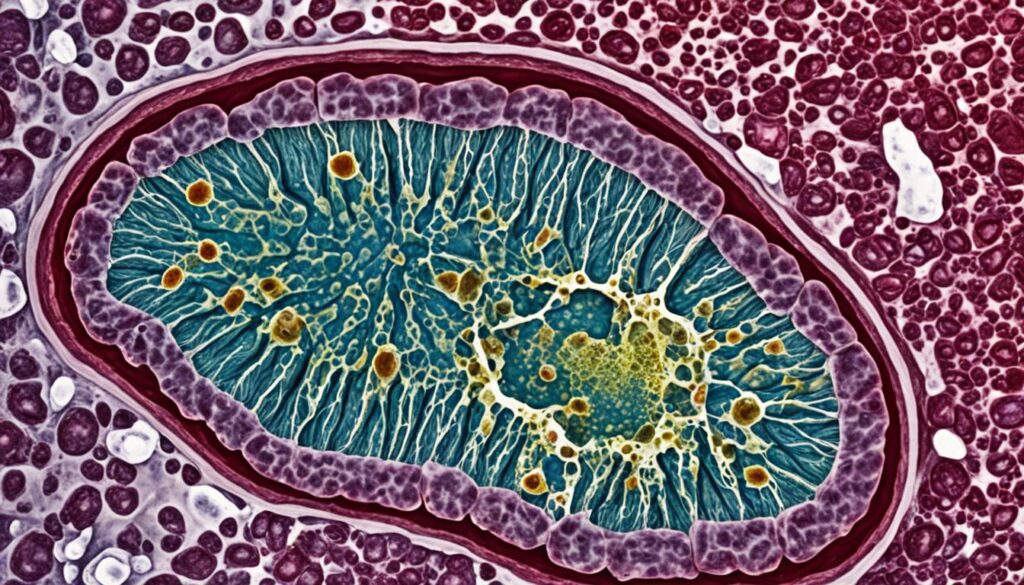
Biliary atresia is a condition in which the bile ducts, both inside and outside the liver, become scarred and blocked. This prevents bile from flowing into the intestine, resulting in a buildup of bile in the liver. Over time, this can lead to scarring, loss of liver tissue and function, and ultimately cirrhosis.
Biliary atresia is a serious condition that primarily affects infants. It is characterized by the abnormal development or absence of bile ducts, which are responsible for carrying bile from the liver to the small intestine. Without proper bile flow, the liver becomes damaged, leading to further complications.
How does biliary atresia occur?
The exact cause of biliary atresia is not fully understood. It may occur due to a combination of genetic and environmental factors. Some studies suggest that certain viruses, infections, or immune system abnormalities may trigger the condition. However, more research is needed to determine the exact mechanisms behind biliary atresia development.
If left untreated, biliary atresia can lead to severe liver damage and cirrhosis, which is a progressive scarring of the liver tissue. This can eventually result in liver failure and the need for a liver transplant.
If you suspect your child has biliary atresia, it is important to consult a healthcare professional for a thorough evaluation and diagnosis. Early detection and timely intervention can significantly improve outcomes and enhance the quality of life for children with biliary atresia.
Types and Prevalence of Biliary Atresia
Biliary atresia, a rare condition, can be classified into two types: perinatal biliary atresia and fetal biliary atresia.
- Perinatal Biliary Atresia: This type occurs after birth and is the most common form of biliary atresia.
- Fetal Biliary Atresia: Fetal biliary atresia develops during pregnancy.
It is estimated that biliary atresia affects approximately 1 in every 12,000 infants, making it a relatively uncommon condition.
Risk Factors for Biliary Atresia
When it comes to biliary atresia, certain risk factors can increase the likelihood of this condition in newborn infants. While the exact cause of biliary atresia is unknown, research suggests that genetic and environmental factors may play a role in its development.
Although biliary atresia can affect infants of any gender or ethnicity, studies have shown a slightly higher prevalence among female infants and those with Asian or African American heritage. This indicates that certain genetic or ethnic factors may contribute to the risk of biliary atresia.
It’s important to note that biliary atresia is a relatively rare condition, affecting approximately 1 in every 12,000 infants. However, the increased risk in specific populations highlights the importance of understanding these risk factors to ensure proper diagnosis and timely intervention.
While genetic factors may predispose some infants to biliary atresia, it’s crucial to remember that it can occur in babies without any family history of the condition. Environmental factors, such as exposure to certain infections or toxins, could also potentially contribute to the development of biliary atresia.
As medical research continues to explore the underlying causes of biliary atresia, identifying these risk factors can aid in early detection and prompt intervention. By understanding the potential predisposing factors, healthcare professionals can provide appropriate care to newborns and help minimize the long-term impact of biliary atresia complications.

| Risk Factors | Description |
|---|---|
| Female Infants | Female infants have a slightly higher prevalence of biliary atresia compared to male infants. |
| Asian or African American Heritage | Infants with Asian or African American heritage have a slightly increased risk of developing biliary atresia. |
| Genetic Factors | While not fully understood, genetic factors may contribute to the development of biliary atresia in some cases. |
| Environmental Factors | Exposure to certain infections or toxins may increase the risk of biliary atresia. |
Understanding the risk factors associated with biliary atresia can help healthcare professionals provide targeted care and support to affected infants and their families. Early intervention and appropriate management strategies are crucial in improving outcomes and ensuring the best possible long-term health for these infants.
Complications of Biliary Atresia
When a child is diagnosed with biliary atresia, it is important to understand the potential complications that may arise. The blocked bile ducts in this condition can lead to various health challenges, impacting the child’s growth and overall well-being.
Failure to Thrive and Malnutrition

One of the primary complications of biliary atresia is failure to thrive. The blocked bile ducts impair digestion and absorption of nutrients, resulting in poor weight gain and stunted growth. Children with biliary atresia may struggle to gain weight and show signs of malnutrition, such as weakness and delayed development.
Cirrhosis and Related Complications
Over time, the buildup of bile in the liver due to biliary atresia can lead to cirrhosis. Cirrhosis is a condition characterized by the scarring and loss of liver tissue, impairing its ability to function properly. The progression of cirrhosis can give rise to various complications, including:
| Complication | Description |
|---|---|
| Portal Hypertension | Increased blood pressure in the portal vein, which carries blood to the liver. This can lead to complications such as varices and ascites. |
| Ascites | Buildup of fluid in the abdomen, causing discomfort and distension. |
| Varices | Dilated and swollen blood vessels in the digestive tract, which can rupture and cause life-threatening bleeding. |
Liver Failure
If left untreated, the continued damage to the liver caused by biliary atresia can result in liver failure. Liver failure occurs when the liver is no longer able to perform its vital functions, leading to severe health consequences and requiring immediate medical intervention, such as a liver transplant.
It is crucial for healthcare professionals to monitor and manage these complications effectively, providing specialized care and support to children with biliary atresia. Early diagnosis, proper nutrition management, and ongoing medical interventions can significantly improve the long-term outcomes for these children.
Treatment Options for Biliary Atresia
When it comes to treating biliary atresia, there are several options available to manage the condition effectively. The primary treatment for biliary atresia is a surgical procedure known as the Kasai procedure. This procedure aims to restore the flow of bile from the liver to the intestine, helping to prevent the progression of cirrhosis and liver failure.
The Kasai procedure involves connecting the small intestine directly to the liver to bypass the blocked bile ducts. By doing so, bile can flow freely, minimizing the damage to the liver and optimizing liver function. It’s important to note that the success rate of the Kasai procedure is higher when performed within the first two months of life.
Although the Kasai procedure is effective in many cases, some children may still require a liver transplant in the future. A liver transplant is considered when the Kasai procedure fails to sufficiently restore bile flow or if the liver becomes severely damaged over time. This surgical intervention involves replacing the diseased liver with a healthy liver from a donor.

It’s essential to manage biliary atresia comprehensively to ensure the best possible outcome for affected individuals. This includes regular monitoring of liver function, nutritional support, and careful management of associated complications. A multidisciplinary healthcare team, consisting of pediatric gastroenterologists, hepatologists, surgeons, and nutritionists, plays a crucial role in the ongoing management and treatment of biliary atresia.
Impact on Nutrition and Growth
Children with biliary atresia face challenges in nutrition and growth due to the reduced flow of bile to the small intestine. This condition can lead to malnutrition and hinder proper growth and development.
The liver damage caused by biliary atresia compromises digestion and nutrient absorption, posing additional risks to a child’s overall health. To support their growth, it is crucial to prioritize nutrition management and ensure adequate intake of essential nutrients.
Proper nutrition plays a vital role in supporting the child’s development, promoting healthy weight gain, and optimizing their overall well-being. A multidisciplinary approach involving healthcare professionals, including pediatric gastroenterologists and dieticians, can help develop a tailored nutrition plan for each child.
Here are some key considerations for managing nutrition in children with biliary atresia:
- Ensure a nutrient-dense diet that provides all essential macro and micronutrients.
- Monitor the child’s growth and weight regularly.
- Consider nutritional supplements, such as vitamins and minerals, under the guidance of a healthcare professional.
- Ensure a balanced and varied diet, including lean proteins, fruits, vegetables, whole grains, and healthy fats.
- Manage portion sizes to meet the child’s specific needs.
- Avoid excessive intake of processed foods, sugary beverages, and foods high in saturated fats.
Growth Monitoring
Regular monitoring of a child’s growth is crucial to identify any growth-related concerns early on. The healthcare team may track growth parameters such as weight, height, head circumference, and body mass index (BMI) over time to ensure that the child is growing at an appropriate rate. Adjustments to the nutrition plan can be made if necessary to address any growth issues.
Importance of Bile Flow
The normal flow of bile is essential for proper digestion and absorption of fats and fat-soluble vitamins (A, D, E, and K).
Bile aids in the digestion of dietary fats by emulsifying them and facilitating their breakdown. It also helps in the absorption of fat-soluble vitamins. In children with biliary atresia, the reduced bile flow hampers these processes, leading to potential deficiencies in essential nutrients.
To support optimal bile flow and aid digestion, a healthcare professional may recommend the following:
- Include fat-soluble vitamins in the child’s diet or provide them as supplements.
- Opt for smaller, frequent meals to aid digestion.
- Consider using bile acid supplements under medical supervision to enhance fat absorption.
Ensuring Adequate Caloric Intake
Children with biliary atresia may require higher calorie intake to meet their nutritional needs and support healthy growth. A healthcare professional can help determine the appropriate caloric intake for a child based on their age, weight, activity level, and overall health.
| Food Group | Examples |
|---|---|
| Proteins | Lean meats, fish, poultry, eggs, dairy products, legumes |
| Fruits | Fresh fruits, unsweetened fruit juices |
| Vegetables | Leafy greens, cruciferous vegetables, colorful vegetables |
| Whole Grains | Brown rice, quinoa, whole wheat bread/pasta, oats |
| Healthy Fats | Avocado, nuts, seeds, olive oil |
| Fluids | Water, milk, fresh juices |
Ensure a well-balanced diet that includes a variety of foods from different food groups to provide essential nutrients for optimal growth and development.
By focusing on nutrition management and supporting healthy growth, children with biliary atresia can overcome some of the challenges posed by the condition and thrive towards a better quality of life.
Understanding the Etiology of Biliary Atresia
The exact cause of biliary atresia is not fully understood. It is believed to be a multifactorial condition involving both genetic and acquired factors. Genetic factors may play a role in some cases, while acquired factors such as inflammation, infections, and exposure to toxins may contribute to the development of biliary atresia.
Possible Causes of Biliary Atresia
- Genetic factors: Some cases of biliary atresia may have a genetic predisposition, although specific genes involved have not been identified.
- Acquired factors: Inflammation in the bile ducts, infections such as viral or bacterial infections, and exposure to certain toxins could potentially trigger the development of biliary atresia.
The combination of genetic and acquired factors likely contributes to the complex etiology of this condition.
Diagnostic Process for Biliary Atresia
The diagnosis of biliary atresia involves a combination of clinical evaluation and diagnostic tests. To accurately assess the condition, healthcare professionals utilize various tests to evaluate liver function, identify blockages, and determine the extent of liver damage.
- Liver function tests: These blood tests measure the levels of enzymes and proteins that indicate how well the liver is functioning. Abnormal results can suggest liver damage or dysfunction.
- Ultrasonography: This non-invasive imaging technique uses sound waves to create images of the liver and bile ducts. It helps identify any structural abnormalities or blockages.
- Cholangiography: This diagnostic procedure involves injecting a contrast dye into the bile ducts, allowing for detailed X-ray images to be taken. It helps visualize the bile ducts and any obstructions.
- Liver biopsy: A liver biopsy involves removing a small tissue sample from the liver for microscopic examination. It helps assess the extent of liver damage and can aid in confirming the diagnosis of biliary atresia.
By carefully analyzing the results of these tests, healthcare professionals can confirm the diagnosis of biliary atresia and develop an appropriate treatment plan. These diagnostic procedures play a crucial role in initiating timely interventions to ensure the best possible outcomes for individuals with biliary atresia.
Prognosis and Long-Term Outlook
With early intervention and treatment, the prognosis for infants with biliary atresia is promising. Many children can survive into adulthood, leading healthy and fulfilling lives. However, the long-term outlook can vary depending on the severity of the condition and the individual’s response to treatment.
For some children, the liver’s function may be sufficiently improved with treatment, allowing them to maintain optimal health without the need for further interventions. These children have a good long-term prognosis and can expect to lead normal lives.
However, in more severe cases where liver damage is extensive, a liver transplant may be necessary to ensure long-term survival and overall health. A liver transplant involves replacing the damaged liver with a healthy liver from a donor. Advances in medical technology and transplantation procedures have significantly improved survival rates and outcomes for children undergoing liver transplants.
It is important to note that the need for a liver transplant is not indicative of treatment failure but rather a necessary step in providing the best possible long-term care for the individual. Regular follow-up appointments with healthcare professionals will be essential to monitor liver function and overall well-being after a transplant.
While the long-term outlook for children with biliary atresia can be positive, ongoing management and support are crucial. This includes regular check-ups, adherence to medication regimens, and lifestyle modifications as advised by the medical team. With proper care and support, children with biliary atresia can live fulfilling lives and achieve their full potential.
Conclusion
Biliary atresia is a complex and potentially severe condition that can have long-term complications for individuals affected by it. However, early diagnosis, timely treatment, and ongoing management strategies are crucial in minimizing the impact of these complications and ensuring the best possible outcomes for those with biliary atresia.
Working closely with healthcare professionals is essential in developing a comprehensive care plan that addresses the specific needs of each individual. Regular monitoring and follow-ups can help identify any potential complications early on and allow for timely intervention.
Prevention also plays a significant role in managing biliary atresia complications. While the exact cause of the condition is still unknown, genetic and acquired factors are believed to contribute to its development. It is important to maintain a healthy pregnancy and avoid exposure to harmful substances during pregnancy to reduce the risk of biliary atresia in infants.
By staying informed, seeking appropriate medical care, and following management strategies recommended by healthcare professionals, individuals with biliary atresia can lead healthy and fulfilling lives. As research and understanding about the condition continue to advance, there is hope for improved outcomes and quality of life for those affected by biliary atresia.
FAQ
What is biliary atresia?
Biliary atresia is a condition in infants where the bile ducts are scarred and blocked, leading to a buildup of bile in the liver. Over time, this can cause cirrhosis, liver failure, and other complications.
What are the types and prevalence of biliary atresia?
Biliary atresia can be classified into two types – perinatal biliary atresia, which occurs after birth, and fetal biliary atresia, which develops during pregnancy. The most common type is perinatal biliary atresia. It affects approximately 1 in every 12,000 infants.
What are the risk factors for biliary atresia?
Biliary atresia primarily affects newborn infants, with slightly higher prevalence in female infants and those with Asian or African American heritage.
What are the complications of biliary atresia?
Complications of biliary atresia include failure to thrive and malnutrition, as the blocked bile ducts hamper digestion and nutrient absorption. Long-term complications can also arise, such as cirrhosis and related complications like portal hypertension, ascites, and varices in the digestive tract. Left untreated, biliary atresia can lead to liver failure.
What are the treatment options for biliary atresia?
The primary treatment for biliary atresia is a surgical procedure called the Kasai procedure, which aims to restore bile flow from the liver to the intestine. Some children may still require a liver transplant in the future even with treatment.
How does biliary atresia impact nutrition and growth?
Children with biliary atresia can experience reduced bile flow to the small intestine, leading to malnutrition and growth problems. The damage to the liver caused by biliary atresia can affect digestion, nutrient absorption, and overall growth. Proper nutrition management becomes crucial in supporting the growth and development of these children.
What is the etiology of biliary atresia?
The exact cause of biliary atresia is not fully understood. It is believed to be a multifactorial condition involving both genetic and acquired factors. Genetic factors may play a role in some cases, while acquired factors such as inflammation, infections, and exposure to toxins may contribute to the development of biliary atresia.
How is biliary atresia diagnosed?
The diagnosis of biliary atresia involves a combination of clinical evaluation and diagnostic tests. Liver function tests, ultrasonography, cholangiography, and liver biopsy are commonly used to assess liver function, identify any blockages, and determine the extent of liver damage. These tests help in confirming the diagnosis and planning appropriate treatment.
What is the prognosis and long-term outlook for biliary atresia?
With early intervention and treatment, most infants with biliary atresia can survive to adulthood. However, the long-term outlook depends on the severity of the condition and the individual’s response to treatment. Some children may require a liver transplant at some point in their lives to maintain optimal liver function and overall health.
What is the conclusion regarding biliary atresia and its complications?
Biliary atresia is a complex condition with potential long-term complications. Early diagnosis, timely treatment, and ongoing management play vital roles in minimizing the impact of biliary atresia complications on an individual’s long-term health. It is important to work closely with healthcare professionals to develop a comprehensive care plan and ensure the best possible outcomes for those with biliary atresia.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.





