Your pancreas plays a significant role in digestion. They also regulate blood sugars.
Acute pancreatitis is a sudden inflammation of the pancreas, a vital gland responsible for digestion and blood sugar regulation. While many cases resolve with prompt treatment, severe instances can lead to life-threatening complications.
Table of Contents
ToggleWhether you’re seeking to understand symptoms, causes, treatment, or long-term recovery, this guide offers a complete breakdown based on current clinical insights.
In this blog, we will break down acute pancreatitis in the simplest terms. From early signs to diet tips, causes, and even the nursing diagnosis for acute pancreatitis, everything you need to know is covered.
What is Acute Pancreatitis?
Acute pancreatitis is a sudden swelling or inflammation of the pancreas. The pancreas is a gland behind your stomach that helps digest food and control blood sugar through pancreatic enzymes and insulin.
Why is the pancreas so important?
It plays a key role in the digestive system disorder group. When it gets inflamed, those powerful enzymes begin to attack the pancreas itself instead of helping your body.
Acute vs. Chronic Pancreatitis
| Type | Description | Duration | Reversible? |
|---|---|---|---|
| Acute Pancreatitis | Sudden inflammation | Days to weeks | Usually yes |
| Chronic Pancreatitis | Long-term damage | Months to years | Often no |
What are the Signs of Acute Pancreatitis?
The symptoms of acute pancreatitis can be scary but catching them early makes a big difference. The most common pancreatitis symptoms include:
- Upper abdominal pain that feels sharp or burning
- Pain that worsens after meals
- Vomiting or feeling nauseated
- Belly tenderness
- Fever or rapid heart rate
These signs can often feel like food poisoning or severe gas. But when the pain grows or spreads to your back, it’s time to take it seriously.
When to See a Doctor?
If you have severe abdominal pain that doesn’t go away or worsens, don’t wait. It might be a sign of acute pancreatitis needing hospital care; opt for personalized pancreatitis treatment from a leading gastroenterologist.
What Causes Acute Pancreatitis in Most People?
The most common causes of pancreatitis are
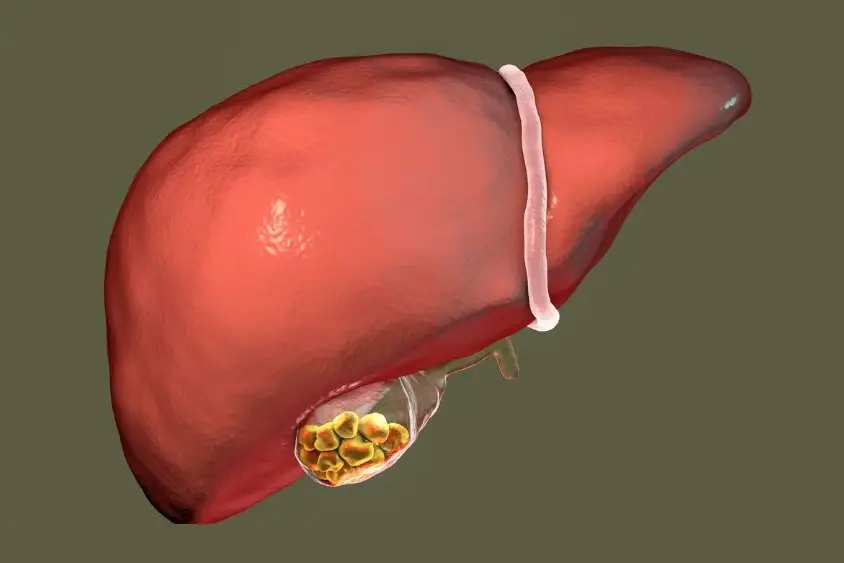
- Gallstones and pancreatitis (about 40–70% of cases)
- Alcohol consumption (about 25–35%)
Other less common causes include:
- Hypertriglyceridemia: Triglyceride levels over 1000 mg/dL are associated with acute attacks.
- Medications: Drugs like azathioprine, valproic acid, and certain antibiotics may trigger inflammation.
- Infections: Viral illnesses like mumps and hepatitis are known culprits.
- Genetic or autoimmune disorders: Hereditary pancreatitis or autoimmune pancreatitis may also be at play
Table: Causes of Acute Pancreatitis
| Cause | % of Cases |
|---|---|
| Gallstones | 40–70% |
| Alcohol | 25–35% |
| High triglycerides | 5–10% |
| Other causes | 5–15% |
Symptoms of Acute Pancreatitis:
Abdominal Pain:
Severe pain localized in the upper abdomen is a defining and often excruciating symptom of acute pancreatitis. This pain may extend to the back and tends to intensify after eating. The distinctive nature and persistence of this abdominal pain serve as a hallmark characteristic, prompting individuals to seek medical attention.
Nausea and Vomiting:
Nausea is a common accompaniment to acute pancreatitis, often leading to bouts of vomiting. This can result in dehydration, exacerbating the overall impact on the individual’s well-being. The combination of nausea and vomiting further underscores the severity of the inflammatory process within the pancreas.
Fever and Rapid Pulse:
Inflammation in the pancreas can trigger systemic responses, including an elevated heart rate and fever. These physiological changes indicate the body’s inflammatory reaction and can provide valuable diagnostic insights for healthcare professionals assessing a potential case of acute pancreatitis.
Jaundice:
Yellowing of the skin and eyes, a condition known as jaundice, may occur in cases where the bile duct is obstructed. This obstruction affects the normal flow of bile, resulting in the accumulation of bilirubin and the characteristic yellow discoloration. Jaundice serves as an additional sign that acute pancreatitis may be impacting the surrounding structures and necessitates careful evaluation.
Read: Home Remedies for Jaundice: Natural Support for Liver Health
How Doctors Diagnose Acute Pancreatitis?
Medical History and Physical Examination: The healthcare provider will assess the patient’s medical history and conduct a physical examination to identify symptoms and potential risk factors.
- Physical Exam: Doctors will gently press your belly to find tender spots.
- Blood Tests: Elevated levels of pancreatic enzymes, such as amylase and lipase, can indicate pancreatitis. Liver function tests will help understand if the cause of pancreatitis is gallstones and help direct management.
- Imaging Tests: Imaging studies like CT scans or MRIs help visualize the pancreas and detect inflammation or other abnormalities.
“We usually look for three key signs before confirming a case of acute pancreatitis: severe belly pain, elevated enzymes, and imaging changes.” – Dr. Nivedita Pandey
Diagnosing early helps doctors decide the best pancreatitis treatment quickly.
Treatment:
- Hospitalization: Acute pancreatitis often requires hospitalization to manage symptoms and monitor complications.
- Pain Management: Pain relief is crucial, and medications may be prescribed to alleviate discomfort.
- Fluid Replacement: Intravenous (IV) fluids help prevent dehydration and maintain electrolyte balance. This is the single most crucial treatment option in acute pancreatitis. It prevents complications and prevents organ damage from severe inflammation.
- Treatment of Underlying Causes: Addressing the root cause, such as gallstone removal or alcohol cessation, is essential to prevent recurrence.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure uses a special dye to outline the pancreatic and bile ducts to remove any stone in the bile duct that might be causing pancreatitis.
What is the Recovery and Long-Term Outlook of Acute Pancreatitis?
Mild Cases:
- Most recover fully in 5–10 days.
- Follow-up care may involve lifestyle changes and periodic monitoring.
Severe Cases:
- Complications like pancreatic necrosis, pseudocysts, or organ failure may prolong hospitalization.
- Some patients develop chronic pancreatitis, leading to exocrine pancreatic insufficiency (EPI), diabetes, or chronic pain
How Does Acute Pancreatitis Affect Your Life?
The short-term effects:
- Low energy
- Poor digestion
- Pain while moving or eating
Long-term risks include:
- Permanent pancreas damage
- Trouble digesting fat
- Increased risk of diabetes
- Higher chances of chronic pancreatitis vs acute
Doctors will monitor your pancreas function through regular checkups and tests.
Is Acute Pancreatitis Life-Threatening?
Yes, in some cases it can be.
About 15–20% of people develop severe acute pancreatitis with serious complications like:
- Organ failure (lungs, kidneys)
- Infections or sepsis
- Pancreatic necrosis (tissue death)
Mortality Rate by Severity
| Type of Pancreatitis | Death Rate |
|---|---|
| Mild | <1% |
| Moderate | 2–5% |
| Severe | 10–30% |
What Lifestyle and Diet Changes Help With Recovery?
Eating right after acute pancreatitis is key. A good pancreatitis diet helps healing and reduces flare-ups.
Table: Best and Worst Foods
| Foods to Eat | Foods to Avoid |
|---|---|
| Steamed vegetables | Fried or greasy foods |
| Lean chicken or fish | Red meat |
| Brown rice or whole grains | Full-fat dairy |
| Water, coconut water | Alcohol, sugary sodas |
Who is at Higher Risk for Acute Pancreatitis?
Certain people have more pancreatitis risk factors than others:
- Age 35–60
- Males (higher alcohol use)
- Obesity and poor diet
- Family history of pancreatic enzymes issues
- People with digestive system disorders
If you fall in any of these categories, speak to a doctor even if symptoms are mild.
Common Complications of Acute Pancreatitis
Some people recover fully. Others develop long-term issues like:
- Pancreatic pseudocysts (fluid-filled sacs)
- Necrotizing pancreatitis (tissue death)
- Breathing problems (ARDS)
- Diabetes due to low insulin production
- Recurrence of acute pancreatitis
Knowing these helps in long-term management and avoiding repeated hospital stays.
Conclusion:
Acute pancreatitis stands as a critical medical condition necessitating immediate and decisive medical intervention. The timely recognition of symptoms, swift initiation of medical attention, and the diligent exploration and resolution of underlying causes are pivotal in effectively managing and preventing complications linked to this ailment. If there is reason to believe that you or someone you know might be undergoing an episode of acute pancreatitis, it is imperative to consult with a healthcare professional promptly. This consultation will entail a comprehensive evaluation of symptoms, medical history, and potential risk factors, enabling the formulation of an accurate diagnosis and the implementation of an appropriate and timely treatment plan.
In conclusion, the proactive management of acute pancreatitis involves a collaborative effort between the individual and healthcare professionals. Prompt recognition of symptoms, timely medical consultation, and a comprehensive approach to address the underlying causes contribute significantly to the effective treatment and prevention of complications associated with acute pancreatitis. Suppose there is any suspicion or concern about the onset of this condition. In that case, it is strongly recommended to consult with a healthcare professional promptly to ensure a thorough evaluation and appropriate care.
Don’t Ignore the Signs
Acute pancreatitis may seem like just a stomach problem, but it can quickly turn dangerous. Recognizing the signs, understanding the causes, and seeking timely care can save lives. If you or someone you love has symptoms or a nursing diagnosis for acute pancreatitis, don’t wait.
Book a consultation today to take control of your health, prevent future attacks, and understand your nursing diagnosis for acute pancreatitis better.
FAQs
Can acute pancreatitis go away on its own?
In mild cases, acute pancreatitis can get better on its own with rest, plenty of fluids, and a short hospital stay. However, it’s not safe to guess at home. Some cases turn severe quickly and can harm organs. Always consult Dr. Nivedita Pandey to find the safest care plan and avoid complications.
What is the fastest way to recover from acute pancreatitis?
The fastest recovery happens when you get early treatment. That means resting your pancreas by not eating, staying on IV fluids, and controlling pain in a hospital. Avoid alcohol and fatty foods completely. Dr. Pandey will also guide you with a personalized treatment and follow-up plan.
What foods worsen acute pancreatitis symptoms?
Greasy, fried, spicy, and sugary foods can inflame your pancreas more. Foods high in fat or processed oils are the worst culprits. Alcohol is also very dangerous. If you’ve had an attack, Dr. Nivedita Pandey can help you create a pancreatitis diet that’s safe and healing.
How long does an episode of acute pancreatitis last?
Most people with mild acute pancreatitis recover in 3–7 days, especially if treated early. More severe cases may take weeks, and some need ICU care. With proper care from a specialist like Dr. Pandey, recovery is faster and safer with fewer risks of relapse.
What should you not do if you have acute pancreatitis?
Don’t drink alcohol, eat fatty foods, skip medicines, or ignore your symptoms. These can make the inflammation worse. Overexerting your body or delaying treatment can cause life-threatening problems. Always follow Dr. Pandey’s advice strictly to avoid another attack.
Is hospitalization always necessary for acute pancreatitis?
Yes, hospitalization is often needed, especially during the first attack. The body needs rest, IV fluids, and constant monitoring. Even if you feel okay, internal swelling can be serious. Dr. Pandey recommends not waiting at home if symptoms worsen—get care right away.
What is the long-term outlook for acute pancreatitis patients?
Many people recover fully if they treat the condition early and make healthy changes. But without care, repeated attacks can cause permanent damage and turn chronic. With regular follow-ups, a proper diet, and lifestyle guidance from Dr. Pandey, you can avoid long-term issues.
Can acute pancreatitis lead to diabetes?
Yes. If the pancreas stays inflamed for too long, it can damage the insulin-producing cells, raising your chance of getting diabetes. Some people need lifelong insulin. Dr. Nivedita Pandey will keep track of your sugar levels and help prevent such risks.
Does smoking increase the risk of pancreatitis?
Absolutely. Smoking harms the pancreas and makes attacks more likely. It also reduces healing and increases the risk of cancer. If you have acute pancreatitis, quitting smoking is a must. Dr. Pandey can also guide you with support programs to stop smoking.
What are the warning signs of a severe complication?
Watch for high fever, trouble breathing, extreme tiredness, or confusion. Also, if your belly swells up or blood pressure drops, it may be an emergency. These signs mean the pancreas or other organs may be failing. Call for help immediately and consult Dr. Pandey without delay.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.