Necrotizing enterocolitis is a severe issue in the gut that mostly happens to babies born too early. It’s a leading cause of severe stomach problems in the neonatal intensive care unit. This condition can make parts of the intestine die. This can make a hole where harmful bacteria can leak out. Newborns who come early and are very small are in the most danger. Signs include not eating well, throwing up, feeling very tired, and a sore belly. Doctors must act fast to diagnose and treat it. Doing so early can help prevent bad outcomes.
Table of Contents
ToggleIntroduction to Necrotizing Enterocolitis
Necrotizing enterocolitis (NEC) is a severe condition of the gut that mostly affects babies, especially those born too soon. It causes the intestine’s wall to get inflamed and infected by bacteria. This then leads to the death of the intestinal tissues. NEC is very dangerous, with up to half of the babies who get it not surviving.
Definition and Overview
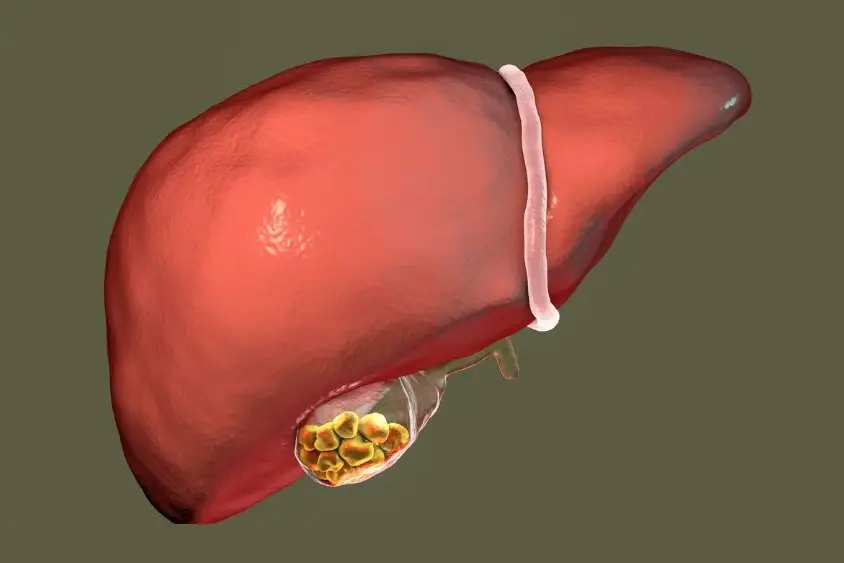
Necrotizing enterocolitis is a tragic disease that attacks the bowels of newborns, mainly premature ones. It happens when the intestine’s wall gets inflamed and is overrun by bad bacteria. The tissue ends up dying, which can cause very serious problems like a hole in the intestine.
Once there’s a hole, the bowels’ contents can leak into the body’s belly, causing even more health issues. This condition is a major concern for babies in neonatal care units.
Prevalence and Risk Factors
Babies born early, especially those with a low weight, have the highest chance of getting NEC. Other things that increase risk include feeding formula, having intestines that haven’t fully developed, and specific genetic factors. NEC usually strikes in a baby’s second or third week of life.
The problem is quite common, with between 0.3 and 2.4 babies out of 1,000 facing it globally. And nearly 70% of these cases are among those born premature before 36 weeks.
what is necrotizing enterocolitis
Necrotizing enterocolitis (NEC) is a severe and life-threatening condition affecting newborns, especially premature ones. It causes the intestinal wall to become inflamed and invaded by bacteria. This leads to tissue death and can create a hole in the intestine.
When the intestine is damaged, it allows bacteria to leak out, leading to severe abdominal infections. Babies born prematurely, especially those with low weight, have a high chance of getting NEC.
NEC is both a medical and surgical emergency, making quick diagnosis and treatment vital. This approach is crucial to lower the risk of complications and the chance of survival. Proper and timely management is key to helping the affected babies.
Even though what is necrotizing enterocolitis is very serious, ongoing research is making a difference. Better medical care is being developed to improve outcomes for babies with this condition. It’s important for doctors and parents to know the causes, symptoms, and treatments for the best results.
Causes and Pathophysiology
The main cause of necrotizing enterocolitis (NEC) is when bacteria invade and cause inflammation in the intestinal wall. The way bacteria get inside is not totally clear. But many think that the gut of premature babies isn’t fully developed, and this makes them more likely to get NEC.
The gut lining of preterm babies is not fully developed. This makes them more open to bacterial invasion, which leads to inflammation and then damage to the tissue. NEC can become really severe. It might even cause a hole in the intestine. This lets bacteria and other things from inside the intestine leak out into the belly. This can lead to a serious infection and even danger to the baby.
Bacterial Invasion and Inflammation
The details on how bacterial invasion and inflammation occur in NEC are not fully known. However, it is thought that the underdevelopment of the gut in premature infants is a big factor.
Intestinal Immaturity in Preterm Infants
The underdeveloped intestinal lining of preterm babies is at higher risk for bacterial invasion. This leads to inflammation and damage to the tissue. NEC can get so bad that it makes a hole in the intestine. This lets out bacteria and other stuff into the belly. This can cause a very serious infection and be life-threatening for the baby.
Symptoms and Signs
The symptoms of necrotizing enterocolitis (NEC) are general and differ by stage.
At the start, babies might not eat well, vomit, have loose stools, their belly gets bigger, and there might be blood in the stool.
Later, they could seem tired, have trouble breathing, or their heart could struggle. Quick action is essential when these signs show up.
Gastrointestinal Symptoms
Babies with NEC may not eat well, may vomit or have loose stools, and sometimes their stomachs get bigger. They might also see blood in their poop.
Systemic Symptoms
NEC’s systemic problems vary, but they often include the baby being sleepy, breathing hard, or their heart not working right. These are signs that the NEC is getting worse and need urgent medical help.
Physical Examination Findings
Doctors might find a baby’s belly is swollen, hurts, or that the sounds in their stomach are low. The baby might start having trouble breathing or not enough oxygen, and their skin could turn blue.

Spotting these NEC symptoms early can help doctors save the baby’s life. It’s crucial for a better outcome for the baby.
Diagnosis and Evaluation
NEC is diagnosed mainly through abdominal imaging. This includes plain film radiography. On X-rays, doctors look for signs like bowel loops that are too wide, pneumatosis intestinalis (air in the bowel wall), and air in the portal vein. These necrotizing enterocolitis abdominal x-rays features help track how severe the condition is. Sometimes, doctors might also use ultrasound or CT scans to confirm the diagnosis.
Abdominal X-rays and Imaging
The necrotizing enterocolitis diagnosis usually depends on noticeable X-ray signs. Pneumatosis intestinalis is when air shows in the bowel wall, marking NEC clearly. If the bowel has a hole, you might also see free air in the abdomen. These signs are vital for figuring out how to treat this life-threatening condition.
Laboratory Tests
Lab tests play a small role in necrotizing enterocolitis evaluation because they often do not show anything specific. A low white cell count is a major clue for sepsis. However, blood tests like cultures usually come back negative. They might also show low sodium and bicarbonate levels. Although not directly diagnostic, these necrotizing enterocolitis laboratory tests help understand the baby’s health.
Management and Treatment
Dealing with necrotizing enterocolitis (NEC) is complicated. The main aims are to stabilize the patient, beat the infection, and save as much intestine as we can. It’s vital to start treatment early to help the patient do better and lower the threat of serious issues.
Initial Supportive Care
At first, supportive care is key for NEC. This means making sure the baby breathes, keeps their blood moving, and giving fluids if they’re in shock. All feeding is stopped and a tube is put through the nose down to the gut. This step prevents more harm and lowers the chance of the gut tearing.
Antibiotics and Nutritional Support
Doctors quickly start strong antibiotics to fight the bacterial infection. The baby won’t eat but gets nutrients through their veins to give the gut a break and help it heal. This support is critical for the baby’s health and to speed up recovery.
Surgical Intervention
If things get worse or don’t get better with medicine, surgery might be the next step. A laparotomy is done, where the doctor cuts to remove dead or damaged gut. They try to save as much as they can. Sometimes, they make a way for waste to leave the body temporarily to help the gut heal. The choice about surgery depends on how sick the baby is and how bad the NEC is.
Complications and Prognosis
Necrotizing enterocolitis (NEC) is a serious health issue with dangerous challenges. It can lead to the intestine breaking, causing severe infections like peritonitis and sepsis. These complications need quick and accurate treatment.
The death rate from NEC is between 10% and 50%. But, it can be close to 100% in severe cases. The outlook for NEC depends a lot on how bad it is when diagnosed and treated. Acting fast and effective treatment can make a big difference.
NEC can lead to problems like peritonitis and sepsis, along with issues in the intestines, liver, and short bowel syndrome. Managing NEC includes stopping normal feeding, removing bowel gas, and giving fluids and nutrients through veins. IV antibiotics are used, and the baby is checked with tests. Sometimes, an operation is needed for a hole in the intestines or a swollen stomach. After surgery, reconnecting the intestine might happen in weeks or months.
After NEC, babies need careful watching for any new issues. Serious problems, like their intestines not working, need a whole team of doctors to look after them. Yet, not much is known about the long-term outcome for babies with NEC. More studies are required to find out what might happen to these babies later in life.
Prevention Strategies
The exact causes of necrotizing enterocolitis (NEC) are still not fully understood. But there are steps that can lower its risk. It’s important to promote breastfeeding and be careful about what babies eat. For example, avoiding certain types of baby formula can help. These steps are key in preventing necrotizing enterocolitis.
Breastfeeding and Careful Feeding
Breastmilk helps protect babies from NEC. This is because it contains many components that boost the immune system. For babies born early, feeding them with human milk lowers the necrotizing enterocolitis risk. If a mother can’t provide milk, safely donated milk is a good option for these babies until they are about 34 weeks old.
Probiotics and Other Potential Interventions
Some studies suggest that probiotics could reduce the risk of NEC. However, more research is needed to confirm this benefit. Scientists are also looking into ways to prevent NEC by targeting nitric oxide production. Using low amounts of carbon monoxide is another approach being studied for its potential.

Necrotizing Enterocolitis in Full-Term Infants
NEC usually happens in babies born early. But it can sometimes occur in full-term babies too, though not as often. For them, NEC usually shows up in the first days of life. It’s linked to things like lack of oxygen, for example from a cyanotic congenital heart defect. How NEC is seen and treated in full-term babies might not be the same as for premature babies. That’s because risk factors and how it happens can be different.
Between 1998 and 2002, a study found 14 full-term babies with NEC. During these years, the number of NEC cases in full-term babies went up from 0.16 to 0.71 per 1,000 live births. The babies’ average weight was 2,829 grams. Almost all were born by Cesarean section. Surprisingly, half of them had no big risk factors for NEC.
These NEC cases started around the 4th day of life and mostly affected the colon. Most babies got better quickly. But one needed surgery because their intestine broke. More Cesarean births were happening too, which might have made NEC more common in full-term babies.
It’s still key to catch NEC early and treat it right away in full-term babies. Doctors need to watch for NEC signs, even without usual risks. This helps them give the best care on time.
Long-Term Outcomes and Follow-Up
Infants who survive necrotizing enterocolitis (NEC) might have health issues for the long haul. This depends on how bad their condition was and the damage to their intestines. They could develop short bowel syndrome, struggle to absorb nutrients, and face growth and learning delays. Research shows that at seven years old, kids who beat NEC may still struggle with bowel problems and function.
It’s vital for these infants to see a doctor regularly. Their progress needs to be watched. Any ongoing health issues should be treated right away. This care is key to help these children do as well as possible in the long run. For many NEC survivors, surgery is necessary. This can lead to tough health challenges, such as not being able to eat enough, slow growth, and more problems digesting food.
NEC’s after-effects can be quite serious. They might need to be fed through a tube for a long time or receive nutrients through a vein. Children might develop short bowel syndrome, face digestive issues, struggle with thinking, and have trouble moving. Plus, they could have breathing issues. A 2020 study explored the long-term impacts on NEC survivors and their parents. It looked into their life quality, both mental and physical health, social situations, and the support they find about NEC.
For the study, there was a survey for parents of NEC kids and one for NEC survivors themselves. The parent survey had 33 questions, and the survivor’s survey had 27. They reached out through emails, the NEC Society’s website, and social media. They invited more than 3000 people this way. The survey results were looked at with statistics for the closed questions and content analysis for the open ones.
Emotional Support for Parents
Having a baby with necrotizing enterocolitis (NEC) can be very hard for parents. The illness is serious, and its outcome is uncertain. Emotional support from healthcare providers is vital. They should connect parents with support groups, counseling, and info about the disease. This helps parents feel less anxious and more in control of their child’s care.
Support for parents who have a baby with NEC is critical. Parents go through a lot of emotions, from the shock of the diagnosis to worry about their baby’s recovery. Doctors and nurses need to understand these feelings. They should make sure parents have the help and information they need.
Helping parents with emotional support is key. This includes connecting them with support groups and counseling. Health workers should also explain clearly about the disease and treatment. These efforts can lessen the stress parents feel. They can also lead to better outcomes for the baby and the family’s well-being.
Research and Future Directions
Ongoing research into necrotizing enterocolitis (NEC) aims to better understand its causes and ways to prevent and treat it. Researchers are looking at how genetics may play a role. For example, they found a link in a 2017 study between preemies who develop NEC and a specific genetic variant, ATG16L1 (T300A).
Another focus is finding ways to lower the risk of NEC through probiotics and other interventions. In 2019, a study showed preemies who got breast milk had less severe NEC. This was because breast milk reduced a certain factor in the gut. Besides, research reveals that probiotics, like L. rhamnosus GG and Bifidobacterium strains, might help cut down the cases of NEC. However, how well they work is still not certain.
Some researchers are also looking into new surgeries and tools to help infants with serious NEC. A 2018 study using mouse models showed that blocking Rho kinase might help the gut and blood vessels from harm, which could be a way to fight NEC.
There’s also a push to find markers that could tell early on if a baby might get NEC. One study, for example, found seven markers in urine that could really well tell apart NEC from a similar condition called sepsis.
As scientists learn more, the goal is to make big strides in NEC care. The dream is for these efforts to give future infants with NEC a better chance.

Necrotizing Enterocolitis Resources
Are you looking for more info on necrotizing enterocolitis (NEC)? The National Institute of Child Health and Human Development (NICHD) has a lot of details. They cover what NEC is, its risk factors, treatments, and what’s new in research. The American Academy of Pediatrics and other medical groups also share info and guidelines about NEC.
Moreover, there are support groups and online communities for families dealing with NEC. They offer a place to share stories, get advice, and find emotional help. Theses [necrotizing enterocolitis resources] can be very helpful as you face the challenges of this disease.
No matter if you’re a parent or a healthcare provider, these [necrotizing enterocolitis resources] are key. They help you understand this condition, find up-to-date information, and connect with others who understand what you’re going through.
Conclusion
Necrotizing enterocolitis (NEC) is a severe issue that mostly impacts early babies. Knowing the causes, symptoms, and management of NEC is key for doctors and parents. This helps in quick discovery and a powerful cure. Even though dealing with NEC is hard, new studies and better medical ways are making a difference for the little ones affected by this harsh disease.
To lower the risk of NEC, doctors suggest breastfeeding. They are also looking into how probiotics might help. Full care is vital, starting with quick help, then proper medicine, and even surgery when needed. This approach can improve the babies’ health for the long term. Also, giving emotional help to families helps them support their child better through support groups and resources.
The fight against necrotizing enterocolitis is getting better each day. An early focus on spotting it, treating effectively, and continuous study are key. This shows that the healthcare team’s efforts can cut down the danger and tough outcomes linked with this stomach issue. This, in turn, makes a real difference in the lives of these fragile babies.
FAQ
What is necrotizing enterocolitis?
Necrotizing enterocolitis (NEC) is a severe gut issue often found in premature babies. It causes the intestines to become inflamed and infected. This can lead to parts of the intestinal wall dying.
What are the symptoms of necrotizing enterocolitis?
Babies with NEC might not eat well, throw up, and feel very weak. They can get a tender tummy too. As NEC gets worse, they might have trouble breathing, look blue, and have poor blood flow.
What causes necrotizing enterocolitis?
NEC is caused by bacteria attacking the gut, leading to inflammation. The digestive system of premature babies isn’t fully developed, making them more prone to this bacterial attack.
How is necrotizing enterocolitis diagnosed?
Doctors diagnose NEC by checking the baby’s abdomen with X-rays. They look for signs like a swollen bowel, bubble-like structures in the gut, and air around the liver.
How is necrotizing enterocolitis treated?
Treating NEC is a team effort. It involves making sure the baby can breathe and their heart is working right. They stop feeding the baby by mouth and use IV nutrients. Antibiotics are given. Sometimes, surgery is needed.
What are the potential complications of necrotizing enterocolitis?
NEC can lead to serious problems like holes in the gut, belly infections, and blood infections. It can be deadly too, with between 10 to 50 out of 100 babies not surviving it.
How can necrotizing enterocolitis be prevented?
To help avoid NEC, it’s vital to encourage breastfeeding and avoid certain formulas. Adding probiotics to the baby’s diet might also lower the risk. Careful feeding and keeping a watch on how the baby responds are crucial.
What are the long-term outcomes for infants who survive necrotizing enterocolitis?
Babies who live through NEC might still face some health challenges. These could affect how they grow and learn. Regular check-ups with a specialist are key to helping them stay healthy.
How can parents and families cope with the emotional impact of necrotizing enterocolitis?
Doctors and nurses should provide support and link families to others going through similar situations. They should also give helpful information to reduce stress and worry.
What new research is being conducted on necrotizing enterocolitis?
Scientists are working hard to understand NEC better and find ways to prevent and treat it more effectively. This includes looking into things like genes, probiotics, and new medical and surgical approaches.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.