GERD and stress move together for many people. Stress changes how your gut works. That change can raise acid flow into the esophagus. This is why your chest burns more during tough weeks. When you calm your body and treat reflux, symptoms drop. That is the direct link.
Table of Contents
ToggleCan Stress Really Cause Acid Reflux?
Yes. Stress does not create acid from thin air. It shifts brain and gut signals that guide digestion. That shift can set off reflux. The stress acid reflux connection shows up in daily life. You rush meals, drink more coffee, and sleep less. Those choices add fuel.
Stress also acts inside the gut. Nerves and hormones change tone and motion. That is where GERD and stress begin to flare.
The Physiological Link Between Stress And Digestion
Your brain and gut talk through the vagus nerve. Stress turns the dial on that line. Blood moves to muscles. Gut motion slows. Food stays longer in the stomach. Pressure builds. The valve that guards the esophagus can open at the wrong time. Acid then moves up. That is how stress causes GERD to show during hard days.
How Stress Affects The Lower Esophageal Sphincter
The lower esophageal sphincter, or LES, is a ring of muscle at the top of the stomach. Its job is simple. Keep acid down. Stress can make the LES relax at the wrong time.
Small burps become more common. Those burps can carry acid mist. The lining gets sore. You feel heartburn. This is a common path where GERD and stress meet.
The “Fight Or Flight” Response And Increased Acid Production
Fight or flight readies your body to act fast. Heart rate climbs. Breathing speeds up. The stomach may make more acid. At the same time, emptying slows. More acid sits for longer. Pressure rises against the LES. Reflux follows. Many people notice worse burns on long, tense days. That is the pattern with GERD and stress.
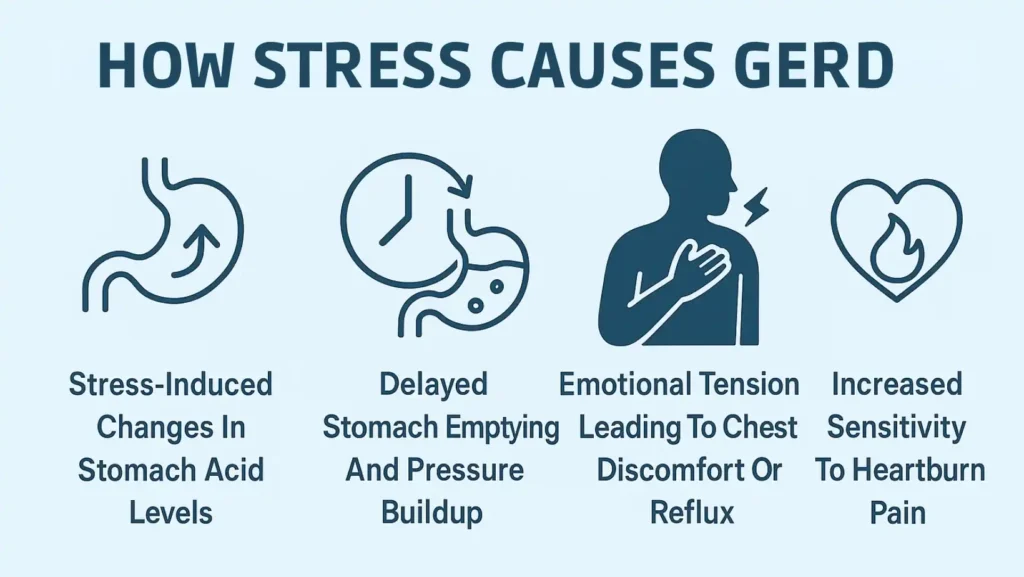
How Stress Causes GERD Symptoms
Think of a chain. Stress hormones rise. Stomach emptying slows. Gas forms. Pressure presses on the LES. Acid splashes up. The esophagus gets inflamed. You feel pain. You may also taste sour fluid. Your brain reads the signals as a threat. Pain feels bigger. That is the loop behind GERD and stress during busy seasons.
Stress-Induced Changes In Stomach Acid Levels
Some people make more acid under stress. Others do not. Either way, acid hurts when it is in the wrong place. Stress can thin the mucus shield in the gut. Less shield means more sting. Even normal acid can feel harsh. This helps explain GERD and stress spikes without a big diet change.
Delayed Stomach Emptying And Pressure Buildup
When food lingers, the stomach swells. Gas adds volume. Pressure rises like air in a balloon. The LES can pop open for a second. Acid slips up. You burp often. You feel full after small meals. You feel tight under the ribs. These are classic stress days with GERD and stress.
Emotional Tension Leading To Chest Discomfort Or Reflux
Tension makes you clench and hunch. You breathe high in your chest. That posture squeezes your belly. Pressure pushes on the LES. Acid moves up. You feel a burn that rides with mood swings. Fixing posture can ease that burn. Relaxed breathing helps too.
Increased Sensitivity To Heartburn Pain
Stress primes the brain to scan for danger. Nerve signals from the esophagus feel louder. The same splash may feel like sharp fire. You wake at night from minor reflux. It feels worse than usual. This is why GERD and stress can seem severe even when acid levels are not extreme.
The Connection Between GERD And Anxiety
Anxiety is not just worry thoughts. It is a bodily state. Pulse spikes. Muscles tense. Breathing speeds up. Your gut slows. You notice every twinge. That raises distress. Reflux feels stronger. Worry rises again. The acid reflux anxiety stress link is a two-way street. Treating both sides works best.
Why Anxiety Makes Reflux Symptoms Worse
Anxious breathing is fast and shallow. You swallow more air. More air means more belching. Each belch can open the LES for a moment. Acid mist follows. You also scan for pain. Small burns feel big. This is a clear reason GERD and stress often flare with worry.
How GERD Can Trigger Panic-Like Sensations
Strong heartburn can mimic chest pain. You may feel tightness and sweat. You may fear a heart issue. Fear spikes. Breathing speeds up more. More air goes into the stomach. Pressure grows. Reflux worsens. A tight loop forms. Breaking the loop takes calm breathing, upright posture, and steady steps.
The Stress–GERD Feedback Loop Explained
Stress raises reflux. Reflux pain raises stress. Sleep drops. Short sleep raises acid and hunger hormones. You snack late. You lie down soon after eating. Gravity stops helping. Night symptoms grow. To break the loop, you tackle mind and gut at once. That brings GERD and stress under control.
Signs You’re Experiencing Stress-Related Acid Reflux
Look for patterns across a week. Note stress level, meals, sleep, and symptoms. When stress climbs and heartburn follows, you have a clue. And yes, stress can trigger GERD symptoms for many people.
Burning Or Tightness In The Chest After Emotional Episodes
After a heated talk, your chest burns or feels tight. The burn may rise to the throat. A sour taste can follow. Calm breathing and a slow walk often help. This points to GERD and stress as a pair.
Heartburn That Worsens During Work Or At Night
Desk hours often mean slouching. Slouching raises belly pressure. Late emails can push dinner late. Then you lie down. Acid slides up. If nights spike after tense days, you likely have GERD and stress feeding each other.
Constant Throat Clearing Or Coughing Under Stress
Acid can irritate the voice box. You feel a lump. You clear your throat a lot. A dry cough shows up. When stress fades, these often ease. Track that change. It supports the stress can trigger GERD symptoms for you.
Nausea Or Bloating When Anxious
The stomach stalls when you worry. Food sits and gas builds. You feel queasy. You burp more. Pants feel tight at the waist. These signs fit with GERD and stress during rough days.
How To Manage Stress-Triggered GERD Symptoms
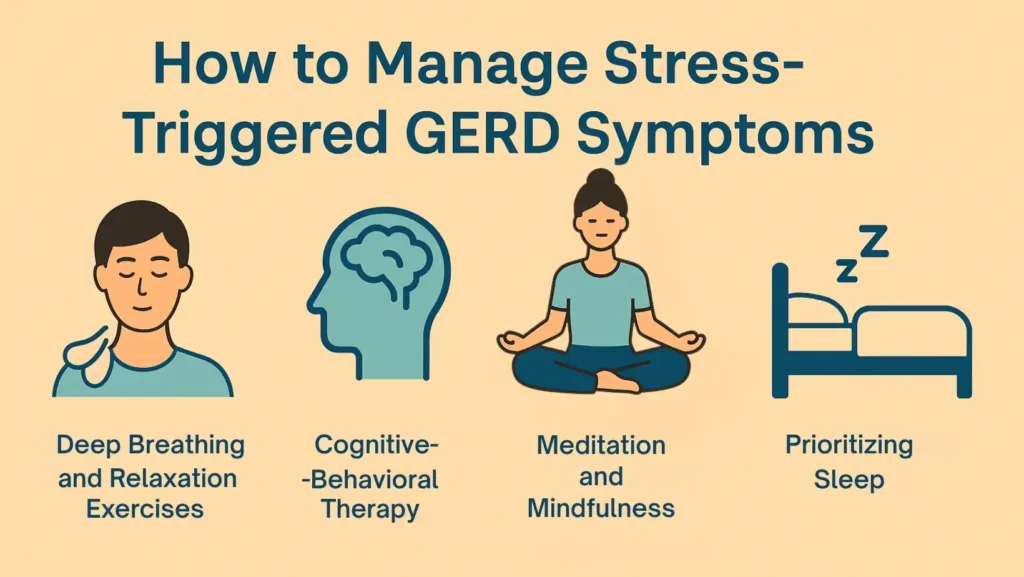
You need skills that calm your nerves and move food along. Use them daily. Short, repeatable habits beat rare long sessions. The goal is steady acid reflux stress relief you can feel.
Deep Breathing And Relaxation Exercises
Use box breathing before meals. Breathe in for four, hold for four, out for four, hold for four. Do this for two to five minutes. Your heart rate slows. Your chest opens. Stomach pressure falls. Try paced breathing at six breaths per minute for five minutes. Do it after the largest meal. These steps calm GERD and stress fast.
Practical cues:
- Sit tall with feet flat.
- Rest one hand on the belly.
- Let the belly rise with each inhale.
- Keep the jaw loose and the shoulders down.
Cognitive-Behavioral Therapy For Anxiety-Related Reflux
Cognitive-behavioral therapy, or CBT, teaches thought and habit skills. You learn to test fear stories. You train attention away from body alarms. You practice calm actions when symptoms start. Many people see fewer flares and better sleep. CBT works well when the acid reflux anxiety stress link is clear.
Tips to start:
- Ask your doctor for a CBT referral.
- Try a six to eight-session plan.
- Practice skills between visits for ten minutes a day.
Meditation And Mindfulness To Reduce Gut Tension
Set a short daily sit. Two to ten minutes is enough. Focus on breath or ambient sounds. When the mind wanders, label it, then return. This reduces pain gain. You react less to minor burns. Your body settles faster. That makes GERD and stress easier to handle.
Quick setup:
- Same time each day.
- Quiet room or headphones.
- Eyes closed or soft gaze.
- Timer to avoid clock watching.
Prioritizing Sleep For Digestive Recovery
Sleep repairs tissue and balances hormones. Short sleep raises acid risk and hunger. Build a steady routine.
- Keep the last meal three hours before bed.
- Use a wedge pillow if nights are rough.
- Limit screens in the last hour.
- Keep the room dark, cool, and quiet.
Better sleep supports LES tone and gut motion. Night symptoms ease when you protect sleep during weeks of GERD and stress.
Medical Treatment For GERD Caused By Stress
When symptoms keep returning, medical treatment can help calm acid while you work on stress skills. A combined approach works better than using only medication or only relaxation. The goal is to protect the esophagus and regain normal digestive flow. Many patients see the best results when both gut and mind factors are treated together. This is because GERD and stress often feed each other.
Proton Pump Inhibitors And Acid Blockers
Proton pump inhibitors (PPIs) lower acid in the stomach. They allow the esophagus lining to heal. These medicines include omeprazole, pantoprazole, and esomeprazole. They are often taken once a day before breakfast. Histamine blockers, such as famotidine, lower acid too, but in a milder way.
These medicines can reduce burning, help sleep, and prevent throat irritation. They do not stop the stress acid reflux connection, but they do protect the tissue while you work on stress control habits.
When Medication And Therapy Are Used Together
Some patients need medical treatment along with stress therapy. This can include CBT sessions, breathing practice, and mindful eating. Using both helps because one handles acid, while the other handles how stress causes GERD symptoms to keep flaring.
Patients who use both usually have:
- Less pain while eating
- Calmer sleep
- Fewer flare-ups on tense days
This combined plan is very helpful when GERD and stress have been going on for months or years.
Importance Of Consistent Follow-Up With Your Doctor
Check in with your doctor if you use PPIs for more than two months. Your doctor may adjust the dose or help you step down slowly. Tracking symptoms in a journal also helps doctors see patterns. This shows whether stress, meals, sleep, or posture play a bigger role.
If symptoms return each time stress increases, that shows the acid reflux anxiety stress link is present. Your care plan should then include stress management steps along with digestive care.
Stress Management Techniques That Help Reflux
You do not need long routines to see results. You need repeated small calming actions that keep the nervous system steady. These actions help reduce stomach pressure, relax the diaphragm, and improve breath control. This is where real acid reflux stress relief begins.
Yoga Poses For Digestion And Calm
Gentle yoga can help release belly tension without bending too deeply. Good poses include child’s pose, seated side stretch, and standing mountain posture. Hold each pose with slow breathing. Avoid yoga right after eating because bending too soon can raise reflux.
Gentle stretching also eases the tight chest posture that often shows up during GERD and stress flare-ups.
Progressive Muscle Relaxation
Progressive muscle relaxation (PMR) lowers full-body stress. Tense a muscle group for five seconds, then relax for ten seconds. Move from the feet upward. This teaches your body to notice tightness early, so flare-ups do not rise as fast.
People who practice PMR regularly often report fewer episodes where stress can trigger GERD symptoms.
Journaling And Emotional Release Techniques
Writing thoughts down helps lower emotional load. Even five to ten minutes a day can reduce gut tension. The goal is to express stress rather than hold it in your body. You can journal triggers, meals, symptoms, and the situation around them. Over time, patterns become clear.
Many people discover moments where GERD and stress rise together. Once seen, these moments can be changed.
Gentle Physical Activity And Posture Control
Light activity speeds stomach emptying and reduces gas. A slow walk after meals helps reduce pressure in the stomach. Good posture also matters. Sitting upright allows space for the stomach and diaphragm to move naturally.
Poor posture raises pressure and makes the stress acid reflux connection feel stronger. One simple cue is to keep your chest open and shoulders down.
Diet And Lifestyle Tips To Reduce Reflux From Stress
Daily habits directly shape reflux. You do not need extreme diet rules. You need consistent, calm choices that protect the LES and support digestion.
Avoid Caffeine, Chocolate, And Spicy Foods During Stress Peaks
These foods can relax the LES or irritate the lining. During hard weeks, limit or avoid them. Replace caffeine with warm herbal tea. Choose mild seasoning instead of spicy meals. This helps prevent GERD and stress from flaring.
Eat Smaller, Slower Meals
Large meals expand the stomach. This pushes hard on the LES. Using smaller plates, chewing longer, and eating slowly lowers this pressure. Slow meals also calm the nervous system. This reduces the acid reflux anxiety stress link.
Stay Hydrated And Limit Alcohol
Water helps digestion and reduces burning. Sip steadily instead of chugging. Alcohol loosens the LES and is best limited during high-stress periods. Reducing alcohol helps many people see fewer evening flare-ups of GERD and stress.
Keep A Regular Meal And Sleep Routine
Your gut works best on rhythm. Eating at random times can confuse digestion signals. Try to eat at similar times daily. Keep the final meal at least three hours before sleep. A regular bedtime helps the gut reset overnight.
These steps directly weaken how stress causes GERD to flare when life gets busy.
When To See A Doctor For Stress-Related GERD
Some signs show you need medical attention. Do not ignore them.
Frequent Heartburn Despite Lifestyle Changes
If you control meals, sleeping posture, and stress, but still have symptoms most days, see a doctor. Persistent GERD and stress patterns may need medical treatment.
Difficulty Swallowing Or Chest Discomfort
Food feeling stuck or chest pressure that feels deep should always be checked. These symptoms need medical review soon.
Anxiety Or Panic Linked With Reflux Episodes
If reflux episodes now bring fear or panic waves, discuss this with your doctor. This confirms the acid reflux anxiety stress link and guides the correct treatment combination.
Frequently Asked Questions
Can Stress Alone Cause GERD?
Stress can weaken the LES and slow digestion, which allows acid to move upward more easily. For some people, stress alone is enough to trigger reflux symptoms during tense days, along with GERD and stress patterns.
How Can I Stop Acid Reflux Triggered By Anxiety?
Use slow breathing, sit upright, and walk for a few minutes. Avoid lying down after eating. Calming the nervous system reduces flare severity and supports acid reflux stress relief in real time.
Does Stress Medication Help With GERD?
Medication that reduces anxiety may help lower body tension, reduce swallowing air, and stabilize breathing patterns. This can help reduce how stress can trigger GERD symptoms in some people.
Can Relaxation Techniques Replace Medication?
Relaxation techniques help reduce pressure, improve posture, and calm sensitivity, but medication may still be needed at first. Both approaches often work well together for GERD and stress control.
Why Does My Reflux Worsen During Stressful Times?
Stress changes gut motion and muscle tension. You may eat faster, breathe shallow, and sleep less. All these increase the stress acid reflux connection and make symptoms stronger.
About The Author

This article is medically reviewed by Dr. Nivedita Pandey, Senior Gastroenterologist and Hepatologist, ensuring accurate and reliable health information.
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist specializing in pre and post-liver transplant care, as well as managing chronic gastrointestinal disorders. Known for her compassionate and patient-centered approach, Dr. Pandey is dedicated to delivering the highest quality of care to each patient.
→ Book a consultation to discover which remedies suit your needs best.
About Author | Instagram | Linkedin