Liver infection occurs when viruses, bacteria, parasites, or rarely fungi invade liver tissue and trigger inflammation that disrupts detoxification, digestion, and energy storage. This condition affects how bile flows, how toxins leave the blood, and how nutrients get processed, which explains why symptoms involve fatigue, jaundice, digestive trouble, and mental fog.
Table of Contents
ToggleSome liver infections clear with timely care, while others persist silently and scar liver tissue over months or years. The danger lies in delayed detection, because early stages often feel mild even as damage continues internally.
Common Symptom of Liver Infection
A liver infection disrupts toxin removal and bile flow, which explains why symptoms affect energy, digestion, skin color, and body temperature. Symptoms often appear gradually and may worsen as liver inflammation increases or spreads.
Fatigue And Weakness
Constant tiredness is one of the earliest signs. You may feel drained even after rest. Muscles feel heavy. This happens because the infected liver cannot store or release energy properly. Waste products also reach the brain, lowering alertness.
Fever And Chills
Fever means your immune system is fighting germs. In a liver infection , fever may rise and fall during the day. Chills happen when the body tries to raise temperature quickly. Persistent fever often signals active infection rather than simple inflammation.
Jaundice (Yellowing Of Skin And Eyes)
Jaundice occurs when bilirubin [a yellow waste pigment from old blood cells] builds up. The liver normally clears it. Infection blocks this process. You may notice yellow eyes first, then skin. Urine turns dark. Stool becomes pale.
Abdominal Pain And Liver Tenderness
Pain usually appears on the upper right side of the belly. It may feel dull or sharp. Deep breathing can worsen it. Swelling occurs when inflamed liver tissue stretches its outer covering, which contains pain nerves.
Nausea, Vomiting, And Loss Of Appetite
Digestive symptoms occur because bile flow slows. Fat digestion becomes difficult. You may feel full after small meals. Long-term appetite loss leads to weight loss and weakness.
These signs form the common symptom of liver infection doctors watch closely. Symptoms may differ by cause and stage.
5 Reasons You May Be At Risk For Liver Disease
Risk factors increase exposure to germs or weaken liver defenses, making a liver infection more likely to develop and harder to clear. Multiple risk factors together significantly raise the chance of severe liver damage.
Viral Infections Such As Hepatitis
Hepatitis viruses directly attack liver cells. Some spread through contaminated food or water. Others spread through blood or body fluids. Chronic viral infection keeps liver inflammation active for years.
Excessive Alcohol Consumption
Alcohol damages liver cells and weakens immune defense. It also increases gut bacteria leakage into blood, sending more germs to the liver. Even moderate drinking worsens infection outcomes.
Obesity And Fatty Liver Disease
Excess fat inside liver cells disrupts oxygen flow. This weakens local immunity. Germs grow more easily in fatty tissue, increasing infection risk and slowing recovery.
Exposure To Contaminated Food Or Water
Poor sanitation allows parasites and bacteria to enter the digestive system. These organisms can migrate to the liver through blood vessels. This risk rises during travel or floods.
Weakened Immune System
Cancer treatment, long-term steroid use, HIV, and uncontrolled diabetes reduce immune strength. In these cases, mild infections can spread rapidly and cause severe liver damage.
These factors explain the 5 reasons you may be at risk for liver disease that clinicians evaluate during assessment.
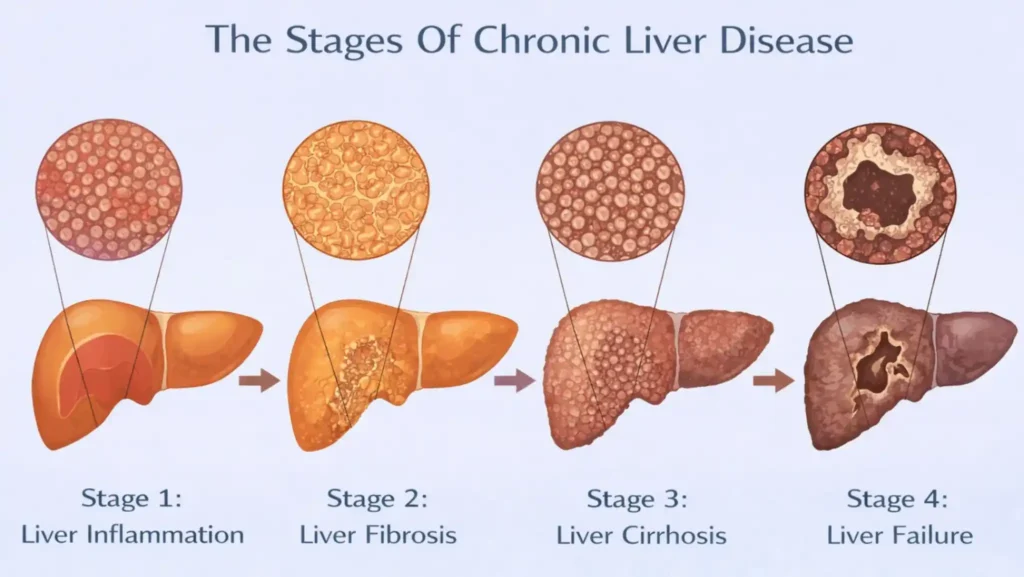
What Are The Stages Of Chronic Liver Disease
A liver infection does not cause sudden failure in most people. Chronic liver damage develops step-by-step when inflammation persists over time. A long-standing liver infection keeps the immune system active, replacing healthy tissue with scar tissue and slowly reducing liver function.
Stage 1: Liver Inflammation
This is the earliest stage. Liver cells swell and immune cells gather. Blood tests show raised enzymes. At this stage, removing the cause often allows full healing.
Stage 2: Liver Fibrosis
Fibrosis means scar tissue begins replacing healthy cells. Blood flow through the liver slows. Symptoms may still be mild, but internal damage increases steadily.
Stage 3: Liver Cirrhosis
Cirrhosis means widespread scarring. Normal structure collapses. Blood bypasses liver tissue, allowing toxins to reach the brain. Swelling, jaundice, and bleeding risk increase.
Stage 4: Liver Failure
The liver loses the ability to perform essential tasks. Toxins affect thinking, called hepatic encephalopathy [brain dysfunction due to liver failure]. Bleeding and infections become life-threatening.
How Liver Infections Progress Over Time
Repeated or untreated liver infection keeps inflammation active. Healing attempts create scars instead of healthy cells. Over years, this leads to irreversible loss of function. Early treatment slows or stops this progression.
These steps define the stages of chronic liver disease used in clinical care.
Diagnosis Of Liver Infection
A liver infection cannot be confirmed by symptoms alone. Many signs overlap with stomach illness or viral fever. Doctors rely on combined testing to find the exact cause and severity. Accurate testing also helps rule out non-infectious liver problems like fatty liver or drug-related injury. Early testing reduces long-term damage and shortens recovery time.
Blood Tests And Liver Function Tests
Blood tests measure liver enzymes such as ALT and AST [proteins released when liver cells get injured]. High levels signal active liver damage. Other tests check bilirubin, clotting ability, and protein levels. These values show how well the liver still performs its core jobs during a liver infection .
Viral Markers And Infection Screening
Specific blood markers detect viruses like hepatitis A, B, or C. Doctors also screen for bacteria or parasites when fever stays high. These tests help identify whether the diagnosis of liver infection points to viral, bacterial, or parasitic causes.
Imaging Tests (Ultrasound, CT, MRI)
Ultrasound shows liver size, blood flow, and abscesses [pus-filled pockets]. CT and MRI give more detail if swelling, tumors, or blocked bile ducts are suspected. Imaging also tracks how far a liver infection has spread within the organ.
Liver Biopsy When Required
A biopsy removes a tiny liver tissue sample. Doctors use it when blood and imaging results remain unclear. It helps assess scarring level and active inflammation. This step is not routine and is done only when needed.
Importance Of Early Diagnosis
Early detection allows targeted treatment before scarring begins. Delayed diagnosis of liver infection increases the risk of chronic disease, cirrhosis, and liver failure.
liver function test
Treatment Of Liver Infection
The treatment of liver infection depends on the cause, severity, and existing liver health. Treatment goals include removing the germ, reducing inflammation, and protecting remaining healthy cells. Most plans combine medication with lifestyle changes and close monitoring.
Antiviral And Antimicrobial Therapies
Doctors prescribe antivirals for viral causes and antibiotics for bacterial infections. Parasitic infections require specific anti-parasitic drugs. Medication choice depends on test results, not symptoms alone. Dosage varies by age, weight, and liver function.
Supportive Care And Symptom Management
Fluids help flush toxins. Fever reducers lower strain on the body. Anti-nausea drugs support nutrition. Supportive care allows the liver to focus energy on healing during a liver infection.
Dietary Modifications During Treatment
Low-fat meals reduce bile stress. Protein intake is adjusted to prevent toxin buildup. Alcohol is completely avoided. Diet changes protect liver cells and speed recovery.
Hospitalization In Severe Cases
Severe pain, confusion, or bleeding require hospital care. IV medications, oxygen, and close monitoring prevent complications. Hospitalization becomes critical when infection affects brain function.
Monitoring Response To Treatment
Blood tests repeat regularly. Imaging checks healing progress. Treatment plans adjust if enzymes stay high. Continuous monitoring ensures the treatment of liver infection remains effective.
Types Of Liver Infections
Different germs affect the liver in different ways, influencing speed of damage and treatment choice. Identifying the exact type of liver infection prevents ineffective treatment and delays in recovery.
Viral Liver Infections
Viruses cause most cases worldwide. Some clear within weeks. Others stay for years and silently damage tissue. Chronic viral infection increases scarring risk even without symptoms.
Bacterial Liver Infections
Bacteria often cause liver abscesses. These infections spread quickly and need urgent antibiotics. Drainage may be required if pus collects.
Parasitic Liver Infections
Parasites enter through contaminated food or water. They may stay dormant before causing symptoms. Travel history helps identify this type of liver infection .
Fungal Liver Infections (Rare)
Fungal infections affect people with very weak immunity. They spread fast and need specialized antifungal drugs. Early detection is critical.
Complications Of Untreated Liver Infection
When untreated, a liver infection continues damaging liver cells, increasing scarring and disrupting blood flow. Complications often appear suddenly after long periods of mild or ignored symptoms.
Progression To Chronic Liver Disease
Repeated inflammation leads to permanent scarring. Liver function slowly declines. Daily activities become harder due to fatigue and weakness.
Liver Abscess Formation
Untreated infection can trap bacteria inside liver tissue. Abscess rupture spreads infection to the blood, causing sepsis [body-wide infection].
Risk Of Liver Failure
Advanced damage stops toxin removal. Brain swelling, bleeding, and coma may follow. Liver failure carries high death risk.
Increased Risk Of Liver Cancer
Long-standing infection increases cancer risk due to repeated cell injury and abnormal repair.
Prevention Of Liver Infection
Prevention focuses on reducing exposure to infectious agents and protecting liver health. Simple actions lower the overall risk of developing a liver infection and reduce disease severity.
Vaccination Against Hepatitis
Vaccines protect against hepatitis A and B. These vaccines reduce severe infection and long-term complications.
Safe Food And Water Practices
Clean water prevents parasites. Proper cooking kills bacteria. Handwashing limits viral spread.
Avoiding Alcohol During Liver Illness
Alcohol worsens inflammation and slows healing. Complete avoidance protects remaining liver cells.
Maintaining Healthy Weight And Hygiene
Healthy weight reduces fatty liver risk. Hygiene blocks germs before they reach the liver.
When To See A Doctor
Certain warning signs indicate worsening liver damage or spreading infection. Prompt medical care during a liver infection greatly improves outcomes and prevents irreversible complications.
Persistent Fever Or Jaundice
Ongoing fever or yellow skin signals active liver injury that needs testing.
Severe Abdominal Pain
Sharp or worsening pain may indicate abscess or swelling.
Worsening Fatigue Or Confusion
Mental changes suggest toxin buildup affecting the brain.
Abnormal Liver Test Results
Unexpected blood test changes require prompt medical review.
FAQs
What Is The Most Common Cause Of Liver Infection?
The most common cause of liver infection is viral hepatitis. These viruses enter through contaminated food, blood exposure, or close contact and directly attack liver cells over time.
Are Liver Infections Contagious?
Some liver infection types spread between people, especially viral forms. Others, like bacterial or parasitic infections, usually come from food, water, or internal spread.
Can Liver Infection Be Cured Completely?
Many liver infection cases fully heal when treated early. Chronic infections may not cure completely but can be controlled to prevent further liver damage.
How Long Does Liver Infection Treatment Take?
Treatment length varies. Mild cases resolve in weeks. Chronic liver infection may need months or long-term monitoring depending on cause and liver health.
Is Liver Infection Life-Threatening?
Yes, severe liver infection can become life-threatening if it causes liver failure, bleeding, or brain involvement without timely medical care.
Can Liver Infections Become Chronic?
Some liver infection types, especially viral ones, can persist for years and slowly cause scarring if untreated or poorly controlled.
What Foods Should Be Avoided During Liver Infection?
Alcohol, fried foods, excess sugar, and processed foods stress the liver. A simple diet supports recovery during a liver infection .
Are Antibiotics Always Needed For Liver Infection?
No. Antibiotics treat bacterial causes only. Viral liver infection requires antivirals, while parasitic infections need specific medications.
Can Liver Infection Lead To Cirrhosis?
Yes. Long-term liver infection keeps inflammation active, leading to scarring and eventually cirrhosis if untreated.
How Can Liver Infections Be Prevented?
Vaccination, clean food and water, avoiding alcohol misuse, and early treatment reduce liver infection risk significantly.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.