Gallbladder problems are often underestimated, yet they can silently progress into severe health conditions. Many people mistake the signs for simple indigestion or acid reflux, but the truth is that gallbladder symptoms can signal issues that need prompt medical care.
Table of Contents
ToggleUnderstanding how these problems present, what causes them, and how they are managed is critical for anyone aiming to protect their digestive health. This article gives a complete view of the gallbladder disease symptoms that matter most and helps you learn when to take them seriously.
What Does Gallbladder Pain Feel Like? (Gallbladder Pain Symptoms Explained)
The most common clue to gallbladder issues is pain. Unlike common stomach pain, gallbladder pain symptoms have a very distinct pattern. The pain usually appears in the upper right side of the abdomen, just beneath the ribcage. It may also extend to the right shoulder blade or the center of the back.
People often describe this pain as sharp and stabbing. Some compare it to being squeezed tightly from inside, while others feel a dull ache that lingers for hours. One hallmark is that symptoms of gallbladder pain often start suddenly, sometimes at night, and can last between 30 minutes and several hours.
A common example is someone eating a greasy pizza or fried chicken, and within an hour they experience intense abdominal pain that radiates to the shoulder. This is not simple heartburn but a sign of biliary colic, where a gallstone temporarily blocks the bile duct.
The difference from gastric pain is that gallbladder pain is less affected by antacids and is more likely to appear after fatty meals. When coupled with nausea or vomiting, this type of pain strongly suggests an underlying gallbladder condition.
Common Gallbladder Disease Symptoms And Bad Gallbladder Symptoms
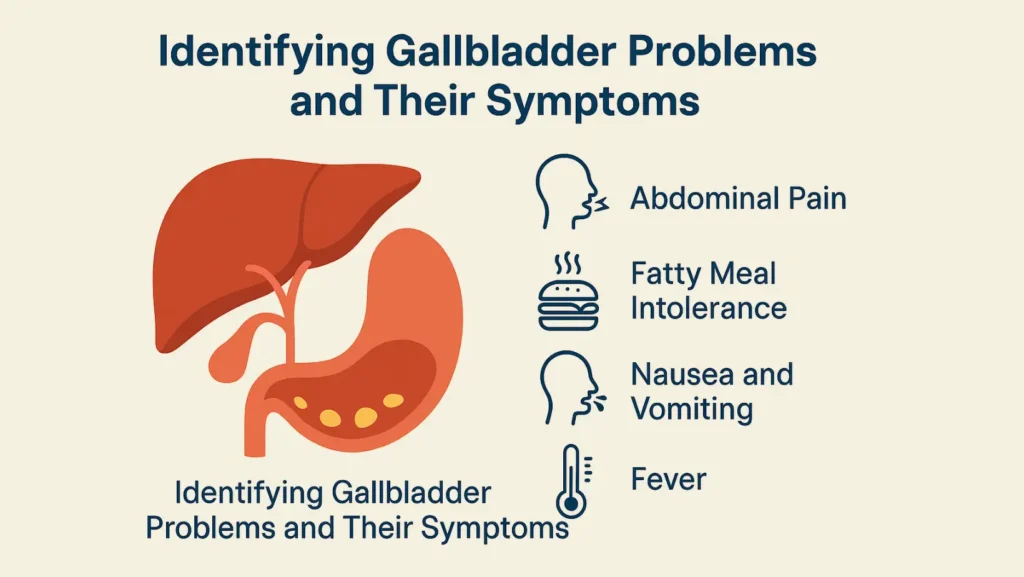
Gallbladder conditions often show patterns beyond pain. Recognizing these signs early helps prevent complications. Common gallbladder disease symptoms include:
- Sharp abdominal pain that worsens after fatty meals
- Pain spreading to the back or right shoulder
- Indigestion with bloating or burping
- Repeated nausea and vomiting
- Fever with gallbladder infection
- Jaundice and gallbladder issues causes yellowing of the skin or eyes.
- Stool abnormalities like pale stools and discolored or dark urine
These are considered bad gallbladder symptoms when they appear together or worsen quickly. For example, a person who develops abdominal pain, fever, and chills may have acute gallbladder inflammation (cholecystitis). Another scenario is when gallstones cause blockage, leading to gallstone blockage symptoms and infections in the bile ducts.
The appearance of jaundice indicates that bile flow is obstructed. This is a serious warning sign that requires urgent medical evaluation. Ignoring such symptoms may result in severe outcomes like a perforated gallbladder, gallbladder cancer, or chronic infections.
What Causes Gallbladder Problems?
The majority of gallbladder problems or gallbladder disease come from gallstones. These stones are hardened deposits of cholesterol or bilirubin that form in the bile. If they remain small and do not block bile ducts, they may go unnoticed for years. Trouble starts when they obstruct the ducts, causing biliary pain and infection.
Other causes include:
- Gallbladder polyps which can sometimes progress to cancer
- Tumors that obstruct the bile ducts
- Infections leading to swelling and inflammation
- Injury from trauma or surgery
- Diseases like sickle cell anemia or liver disease that increase bilirubin levels
Risk factors are often summarized by the “5 Fs”: female, forty, fat, fertile, and fair. Women over 40 who are overweight and have multiple pregnancies face a higher risk, though gallstones can affect anyone. Family history, rapid weight loss, and certain medications also contribute.
A key point is that complications of untreated gallbladder disease can spread to nearby organs. For example, gallstones can cause pancreatitis if they block the pancreatic duct. Chronic cases may even lead to scarring and long-term digestive problems.
How Are Gallbladder Problems Diagnosed?
Diagnosis begins with a clinical evaluation. Doctors ask about the pattern of pain, when it occurs, and if it relates to meals. Physical exam findings include tenderness when pressing the upper right abdomen, sometimes with a sharp pain on inhalation called Murphy’s sign.
The primary diagnostic instrument is the Ultrasound (gallbladder ultrasound). It detects stones, sludge, and thickened gallbladder walls. If ultrasound is inconclusive, doctors may use a CT scan or MRI (gallbladder MRI) for more detail.
When a function needs to be tested, a HIDA scan (cholescintigraphy) is done. It monitors the bile flow to determine if the gallbladder is emptying correctly. This test is especially useful for diagnosing biliary dyskinesia, where no stones are present but the gallbladder is not working correctly.
If blockage of the bile ducts is suspected, an ERCP (Endoscopic retrograde cholangiopancreatography) is both diagnostic and therapeutic. It allows doctors to visualize the ducts and remove stones at the same time.
Blood tests help detect infection, inflammation, and liver or pancreas involvement. Increased white blood cell counts indicate the presence of an infection. High liver enzymes and bilirubin levels suggest obstruction or damage.
Together, these tools provide a clear picture of the condition. For example, a patient with dark urine, pale stool, and elevated bilirubin on a blood test is likely facing an obstructed bile duct.
How Are Gallbladder Problems Treated?
Treatment depends on severity. If symptoms are mild, dietary adjustments may help. Avoiding fried and fatty meals can reduce episodes of pain after fatty meals.
When gallstones are present with repeated symptoms, surgery is the most common solution. Surgery / gallbladder removal (cholecystectomy) can be done laparoscopically with quick recovery. Without the gallbladder, bile flows directly into the small intestine, which most people tolerate well.
In cases of infection, physicians recommend antibiotics and fluids to stabilize the patient prior to surgery. Pain relievers (ibuprofen, Aleve, Motrin) are often used for pain control. In cases where a stone blocks the duct, an ERCP may be done before surgery to remove it.
Rarely, medications can dissolve cholesterol stones, but this takes months and stones often return. When patients are not surgical candidates, drainage procedures may be performed to prevent infection.
Complications like gangrene, abscesses, or a perforated gallbladder require emergency treatment. Advanced cases like gallbladder cancer are treated with surgery, chemotherapy, or radiation depending on spread.
When Should You See A Doctor For Gallbladder Symptoms?
You should not wait if gallbladder symptoms include persistent upper right abdominal pain, fever, or jaundice. Emergency care is needed if pain lasts longer than a few hours, is accompanied by vomiting, or spreads to the chest.
Other warning signs include nausea and vomiting, diarrhea or chronic diarrhea, pale stools, and dark urine. These indicate obstruction of bile flow. Seeking care early prevents severe infections and reduces the risk of pancreatitis or sepsis.
If you experience recurrent but less severe attacks, it is still important to see a doctor. Chronic inflammation can damage the gallbladder over time. Elective surgery in such cases often prevents bigger emergencies later.
The Bottom Line
Gallbladder disease is not just about pain after meals. It involves a wide range of symptoms that can impact digestion, liver health, and even cause life-threatening infections. Identifying bad gallbladder symptoms early, getting timely scans like ultrasound or HIDA, and following through with treatment are key steps.
The gallbladder may be a small organ, but ignoring its signals can have large consequences. Taking abdominal pain seriously is not about being cautious; it is about protecting long-term health and avoiding emergencies that could have been prevented.
FAQs
What are the first signs of a bad gallbladder?
The earliest signs are upper right abdominal pain, bloating after meals, nausea, and occasional vomiting. Pain that worsens after fatty food is a classic early warning.
What are the 5 F’s of gallbladder disease?
The five risk factors are female, forty, fat, fertile, and fair. These traits increase the chance of gallstone formation but do not guarantee gallbladder disease.
How do you confirm gallbladder issues?
Doctors confirm gallbladder issues with physical exam, blood tests, and imaging. The most reliable test is ultrasound, though HIDA scan and ERCP may also be used when needed.
Can a urine test detect gallbladder problems?
A urine test cannot detect gallstones or inflammation. However, dark urine can signal bile obstruction. Imaging studies like ultrasound or MRI are required for accurate diagnosis.
Can a bad gallbladder cause weight gain?
A bad gallbladder does not directly cause weight gain. However, dietary changes, reduced activity due to pain, and digestive issues may contribute to weight fluctuations in some individuals.
What are three treatments for gallstones?
The main treatments include surgical removal of the gallbladder, ERCP to remove duct stones, and bile-dissolving medications in selected cases. Surgery remains the most effective long-term option.
How can you tell the difference between gastric pain and gallbladder pain?
Gastric pain improves with antacids and is often linked to acid reflux. Gallbladder pain is sharper, radiates to the shoulder or back, and worsens after fatty meals.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin




