Understanding the gut liver axis
The gut-liver axis is the biological pathway that links the digestive system with the liver. It’s a constant two-way exchange of nutrients, signals, and waste products that keeps your body in balance.
Table of Contents
ToggleFood enters your gut, where it’s broken down into nutrients and gut-derived metabolites. These nutrients and compounds travel through the portal vein and liver function pathway directly to the liver. The liver processes them, storing energy, making proteins, and removing harmful substances.
There is more than one direction to the gut-liver relationship. The liver also secretes bile into the gut to aid in fat digestion and regulate bacterial levels. This constant liver-gut communication is what keeps gut and liver health stable.
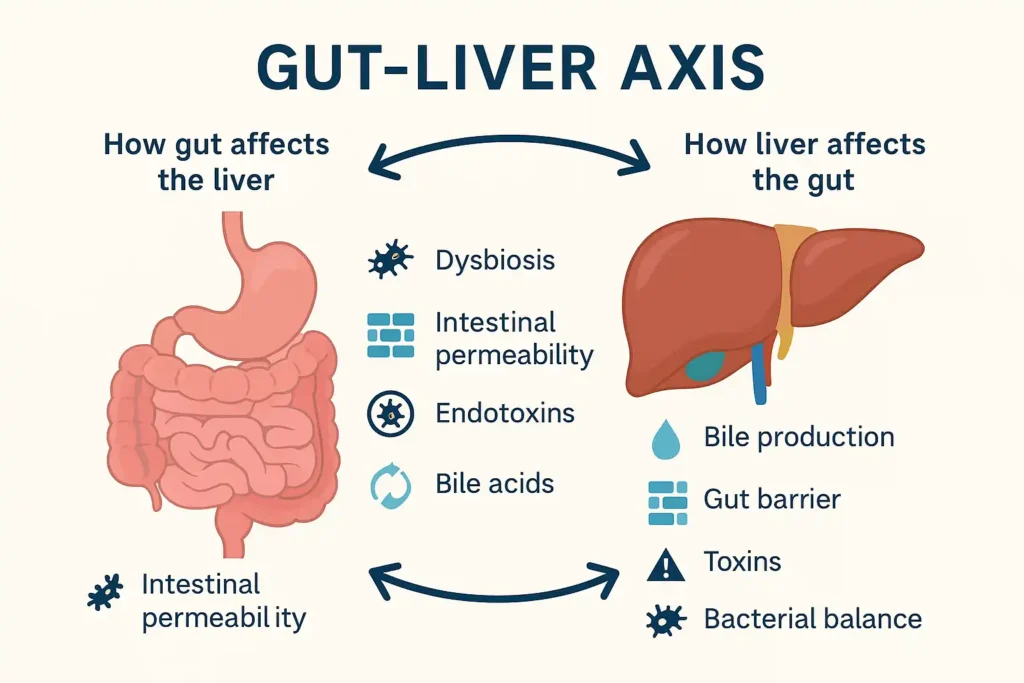
A healthy microbiome in the gut produces short-chain fatty acids (SCFAs) that reduce inflammation, improve the gut barrier function, and protect the liver. But when the gut is damaged, through poor diet, infection, or intestinal permeability, harmful substances like endotoxins and liver inflammation triggers can leak into the bloodstream. This puts stress on the liver and may cause long-term damage.
When the gut-liver relationship works smoothly, digestion, immunity, and metabolism stay balanced. But if it fails, the risk of chronic diseases rises sharply.
How the Gut Affects the Liver?
Your gut is home to trillions of bacteria. This community is called the microbiome. It helps digest food, makes vitamins, and keeps your immune system alert. But when gut bacteria become unbalanced — a problem known as dysbiosis and liver health — it can affect the liver.
One way this happens is through intestinal permeability. Normally, the gut wall acts like a filter, letting only safe substances pass. Toxins and dangerous microorganisms may seep into the bloodstream if the filter deteriorates. These toxins, called endotoxins and liver inflammation triggers, travel to the liver and cause damage.
Gut bacteria also influence bile acids and gut microbiota. Bile acids help digest fats and signal the liver to make or release certain chemicals. Changes in these acids can disrupt fat processing, leading to non-alcoholic fatty liver disease (NAFLD).
Another factor is short-chain fatty acids (SCFAs), produced when gut bacteria digest fiber. These fatty acids help control inflammation and support liver function. A lack of SCFAs can lead to more inflammation and poor liver gut health.
How the Liver Affects the Gut
The liver is not just a passive receiver. It also influences gut health through liver-gut communication. Bile produced by the liver travels to the gut to aid digestion and control bacterial growth. If bile production is low or imbalanced, harmful bacteria can grow too much.
The liver processes toxins and waste products. If liver function drops, these wastes can build up and affect the gut environment. This can weaken the gut barrier function and raise the risk of infections or inflammation.
The liver microbiome interaction is another key factor. The liver shapes the type of bacteria that thrive in the gut. A sick liver can cause bacterial imbalances, making the gut more prone to disease.
Conditions Linked to Gut-Liver Axis Dysfunction
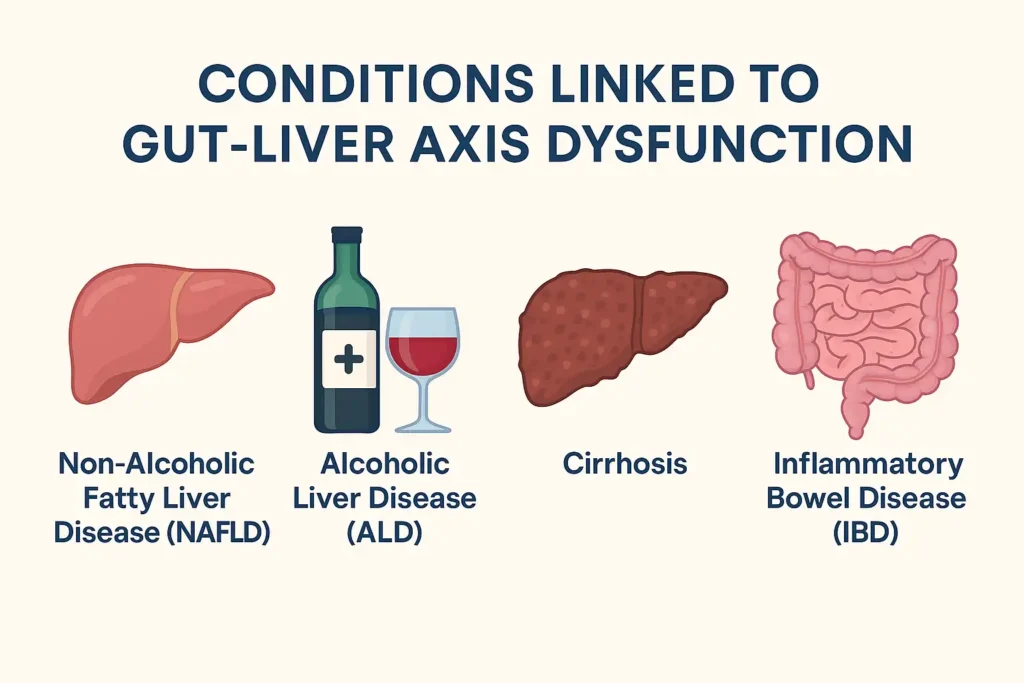
When the gut liver axis is disrupted, a chain reaction begins. Poor gut health can damage the liver, and an unhealthy liver can harm the gut. Some common conditions include:
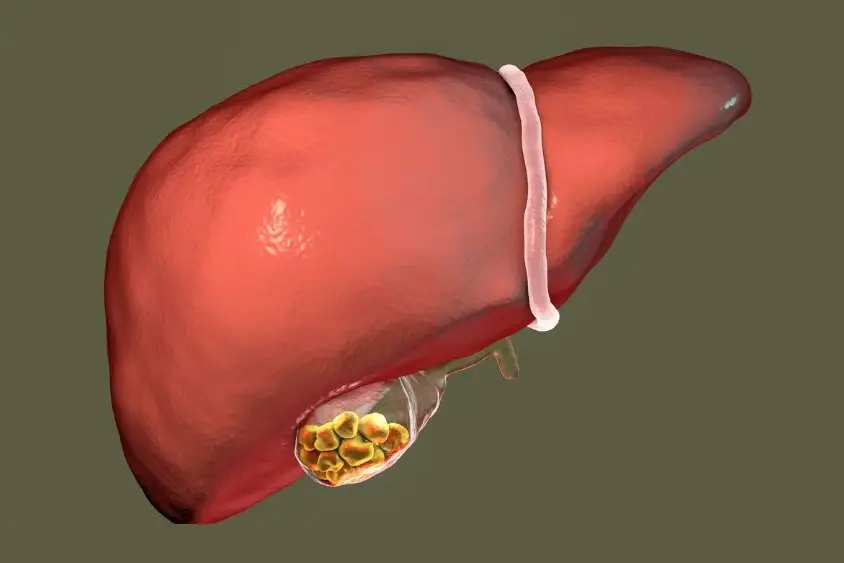
Non-Alcoholic Fatty Liver Disease (NAFLD)
In non-alcoholic fatty liver disease (NAFLD), fat builds up in the liver without alcohol as a cause. It is frequently connected to issues with gut permeability, liver disease, obesity, and poor diet. An unhealthy gut microbiome can send inflammatory signals through the bloodstream, triggering fat accumulation and scarring in the liver.
Alcoholic Liver Disease (ALD)
Also known as alcohol-related liver disease (ARLD), this develops when heavy drinking damages gut bacteria and the gut barrier function. Toxins then leak into the liver, increasing inflammation and worsening liver gut health.
Cirrhosis
When the liver produces scar tissue as a result of persistent infections, ALD, or NAFLD, cirrhosis results. This scarring affects liver microbiome interaction and changes gut bacteria balance, increasing infection risks.
Inflammatory Bowel Disease (IBD)
Conditions such as Crohn’s disease and ulcerative colitis can disrupt the gut lining and elevate hepatic inflammation. This ongoing inflammation stresses the liver, affecting overall gut health and liver stability.
Metabolic Syndrome and Insulin Resistance
When gut bacteria are imbalanced, the body becomes resistant to insulin. This worsens fat storage in the liver and disrupts liver and gut health, increasing the risk of diabetes and cardiovascular problems.
The Role of Diet and Lifestyle
Your daily habits shape liver and gut health more than you think. A diet rich in vegetables, fruits, whole grains, and lean proteins supports a healthy microbiome. Fiber feeds good bacteria, helping produce SCFAs that protect the liver.
Too much sugar, processed food, and alcohol harm the gut-liver axis. They feed harmful bacteria, cause gut-liver immune axis activation, and increase inflammation.
Regular exercise aids in enhancing blood flow, reducing liver fat, and maintaining a healthy balance of gut bacteria. Even small daily movements support gut liver axis function.
Managing stress is important too. High stress affects gut bacteria and can lead to poor liver function.
Therapeutic Approaches
Restoring the gut liver axis is possible with targeted strategies that improve both gut and liver function.
Diet changes are the first step. Eating a fiber-rich diet with vegetables, fruits, legumes, and whole grains feeds good bacteria. This supports gut and liver health by producing SCFAs that reduce inflammation. Healthy fats from fish, nuts, and olive oil improve liver gut health by lowering fat buildup.
Probiotics and prebiotics help correct dysbiosis and liver health problems. Probiotics bring in beneficial bacteria, while prebiotics (foods like garlic, onions, and bananas) feed them.
Reducing alcohol intake lowers liver stress and supports the microbiome. Even moderate drinking can harm the gut liver connection, so cutting back is essential.
Regular exercise improves blood flow, reduces fat in the liver, and helps maintain a diverse microbiome.
Medical treatments may include medications to improve bile flow, lower inflammation, or reduce bacterial overgrowth. Some therapies aim to regulate the gut-liver immune axis to prevent further damage.
Stress management is also important, as high stress can disrupt gut bacteria and weaken the immune system.
Conclusion
The gut liver axis is a powerful partnership that keeps you healthy. When this connection works well, nutrients are absorbed, toxins are removed, and inflammation stays low. But if the system breaks, it can lead to serious diseases.
By caring for gut health and liver function with better food choices, regular activity, and low stress, you can support this vital connection. Small steps can make a big difference in long-term liver and gut health.
Frequently Asked Questions
What is the gut-liver axis?
The gut liver axis is the two-way link between your digestive tract and liver. It involves nutrient transport, immune signaling, and microbiome activity that influence overall health.
Can gut health improve liver function?
Yes. A healthy microbiome strengthens the gut barrier function, reduces harmful toxin leaks, and lowers inflammation, which protects the liver and supports long-term liver gut health.
What foods support the gut-liver axis?
High-fiber foods, fruits, vegetables, lean proteins, and healthy fats promote gut and liver health. Limiting alcohol, sugar, and processed foods protects both organs.
How do I know if my gut-liver axis is imbalanced?
Signs include bloating, fatigue, poor digestion, and abnormal liver test results. Persistent symptoms may require testing for gut permeability and liver disease issues.
Are probiotics good for fatty liver?
Yes. Probiotics can correct microbiome imbalances, reduce inflammation, and improve fat metabolism, helping with non-alcoholic fatty liver disease (NAFLD) management.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.