What causes nonalcoholic fatty liver disease? It might sound like a medical mystery, especially when alcohol isn’t part of the equation. But the truth is millions of people who never touch a drop of alcohol still end up with fat building up in their liver. That fat can quietly damage the liver for years without making any noise.
Table of Contents
ToggleSo, what’s really going on inside the body? Who’s at risk? And most importantly, can it be prevented?
In this blog, we will unpack what causes nonalcoholic fatty liver disease, highlight the red flags you shouldn’t ignore, and break down what steps you can take today to protect your liver.
What is Nonalcoholic Fatty Liver Disease (NAFLD)?
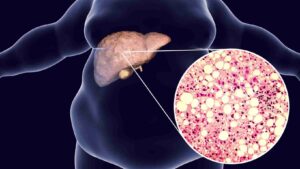
Nonalcoholic fatty liver disease (NAFLD) happens when too much fat builds up in the liver cells of people who drink little to no alcohol. It’s one of the most common liver conditions worldwide and is growing rapidly, especially in India.
How Does Fat Accumulate in the Liver Without Alcohol?
The liver usually processes fats efficiently. But when the body starts to resist insulin and stores more fat, some of that fat gets deposited in the liver.
- The body produces more insulin than needed, leading to insulin resistance.
- Excess calories and sugars get stored as fat.
- The liver stores this fat, leading to liver fat accumulation.
This buildup isn’t just harmless fat, it triggers liver inflammation and may lead to permanent damage over time.
What Are the Different Stages of NAFLD?
NAFLD is not a single disease. It has stages:
| Stage | Description |
|---|---|
| NAFL (Simple Fatty Liver) | Fat in liver without inflammation or damage |
| NASH (Nonalcoholic Steatohepatitis) | Fat with liver inflammation and damage |
| Fibrosis | Persistent inflammation leads to scarring |
| Cirrhosis | Severe scarring and possible liver failure |
Stat: According to the American Liver Foundation, NAFLD affects up to 25–30% of people worldwide.

What Causes Nonalcoholic Fatty Liver Disease?
Experts are still studying why the liver becomes fatty for some. But it’s clear that a few things, like nonalcoholic fatty liver disease (NAFLD) and its worse form, nonalcoholic steatohepatitis (NASH), are tied to several main issues. It’s key to know the causes of nonalcoholic fatty liver disease and the risk factors for NAFLD. This knowledge helps in preventing and handling this common health issue.
How is Insulin Resistance a Core Driver of NAFLD?
Insulin resistance makes it harder for the body to use sugar. The excess sugar gets stored as fat.
- More sugar in blood = more insulin needed.
- Body stops responding properly.
- Fat builds up in organs like the liver.
Insulin resistance is the main metabolic trigger for NAFLD.
Read: How Fatty Liver Disease Affects Pregnancy
Can Being Overweight or Obese Trigger Fatty Liver Disease?
Yes. Obesity is the leading contributor to fat buildup in the liver.
- Fat from belly area travels directly to the liver.
- Overweight individuals often have insulin resistance.
- 70–90% of obese people have NAFLD.
Stat: 70–90% of obese individuals have NAFLD (Source: NIH).
What Role Does Metabolic Syndrome Play in Liver Damage?
Metabolic syndrome is a cluster of conditions like high blood pressure, high blood sugar, and abnormal cholesterol. Together, they increase liver stress.
- High triglycerides and sugar worsen liver fat.
- Belly fat triggers chronic inflammation.
- Liver becomes overloaded and damaged.
Are High Cholesterol and Triglycerides Major Culprits?
Absolutely. They can speed up liver fat accumulation.
- High LDL (bad cholesterol) gets stored in the liver.
- Triglycerides cause fatty deposits.
- The liver can’t process this overload efficiently.
Can Rapid Weight Loss or Malnutrition Cause Fatty Liver Too?
Surprisingly, yes. Losing weight too quickly can confuse your liver.
- Body releases fat into the bloodstream during crash diets.
- Liver absorbs the sudden surge of fat.
- Malnutrition also causes fat metabolism problems.
Is There a Genetic Link to NAFLD?
Genes can make you more likely to develop fatty liver.
- PNPLA3 and TM6SF2 genes are associated with NAFLD.
- Family history increases risk.
- Even lean individuals can get NAFLD if genetically prone.
What Are the Common Risk Factors for Developing NAFLD?
Knowing nonalcoholic fatty liver disease risk factors can help you catch it early.
Does Type 2 Diabetes Increase Your Risk?
Yes, significantly. Diabetics often have insulin resistance, the main trigger for NAFLD.
- Poor blood sugar control stresses the liver.
- NAFLD worsens diabetes complications.
Stat: People with type 2 diabetes are 2 to 4 times more likely to develop NAFLD.
Can PCOS, Hypothyroidism, or Sleep Apnea Be Underlying Causes?
These conditions disrupt hormones and metabolism, affecting the liver.
- PCOS: Triggers insulin resistance in women.
- Hypothyroidism: Slows metabolism, promotes fat storage.
- Sleep apnea: Low oxygen levels damage liver tissue.
Are Men More at Risk Than Women?
Men are slightly more likely to get NAFLD, especially younger adults.
- Hormonal differences play a role.
- However, post-menopausal women catch up due to lower estrogen.
Can Medications Lead to Fat Buildup in the Liver?
Yes. Some medicines are linked to fatty liver.
- Corticosteroids: Promote fat storage.
- Tamoxifen: Affects liver metabolism.
- Methotrexate: Can cause liver toxicity.
To avoid the dangers of NAFLD and NASH, know these risk factors and take steps to care for your liver. Keep watch, make healthy life changes, and team up with doctors to face this serious health risk.
What are the Early Warning Signs You Might Have NAFLD?
NAFLD causes damage silently at first. Recognizing early clues helps.
Why is Fatty Liver Called a “Silent Disease”?
Because most people have no symptoms in early stages.
- Liver has no pain receptors.
- Damage builds quietly over years.
Read: Identifying Nonalcoholic Fatty Liver Disease Symptoms: What to Look For?
Can Fatigue, Upper Right Abdominal Discomfort Signal Liver Issues?
Yes. These are vague but common signs.
- Dull pain under right rib cage.
- General tiredness without cause.
- Poor concentration or weakness.
How Can Liver Enzymes (ALT, AST) Reveal Early Disease?
Elevated liver enzymes in blood tests are red flags.
- Liver function test checks ALT, AST, GGT.
- Elevated levels mean inflammation or damage.
Diagnosis and Testing
Finding out if you have nonalcoholic fatty liver disease is a big first step. It’s mainly found by chance in normal blood tests. These tests show if your liver enzymes are off. They can give us clues about your liver’s health.
Blood Tests and Imaging Techniques
Doctors often start with blood tests to check your liver’s working. They look at liver enzymes, lipids, and inflammation markers. This helps to tell if you have NAFL or NASH. NAFL is less severe than NASH. If needed, imaging like ultrasounds or CT scans can show fat or damage in the liver.
Liver Biopsy
But to be sure about NAFLD, a liver biopsy might be needed. It’s the most direct way to check your liver’s health. In this test, a small bit of liver is taken and looked at. This tells the doctor exactly what state your liver is in. Then, they can suggest the best treatment.
Treatment and Management
If you’ve been diagnosed with simple nonalcoholic fatty liver disease (NAFLD), focus on lifestyle changes. It’s essential to lose weight and improve your cholesterol levels. This reduces liver fat and prevents NASH, a more serious form of the disease.
Lifestyle Modifications
Healthy living is key for NAFLD patients. Start by getting to a healthy weight. A balanced diet and regular exercise are your best friends. Include plenty of fruits, vegetables, and whole grains in your meals. Try to cut out added sugars, refined carbs, and alcohol. Even brisk walking improves your health and your liver.
Read: Fatty Liver Diet: Foods to Eat and Avoid for Better Liver Health
Medication Therapy
For NASH patients, doctors may use medicines. These can target issues like high cholesterol or blood sugar. No drug is directly for NASH, but there’s hope in ongoing research. Antioxidants and diabetes drugs are being tested for NASH.
Working closely with your healthcare team is crucial if you have NAFLD or NASH. A hepatologist or liver specialist can help you make a plan. This plan should fit your unique health needs and manage the disease well.
Prevention Strategies
The top way to fight off nonalcoholic fatty liver disease (NAFLD) is by changing how you live. Keeping a good weight through diet and exercise is key. Fill your meals with fruits, veggies, whole grains, and good fats. But, cut back on sugars, refined carbs, and alcohol. This can lower liver fat and hold off fatty liver disease. Regular exercise, like walking fast, also helps a lot.
If you already have NAFLD, these tips can slow down how fast it gets worse.
Maintaining a Healthy Weight
Getting to and staying at a healthy weight matters a lot. Extra weight, especially around your belly, can add to liver fat. If you eat well and work out often, even losing a bit of weight can make your liver healthier.
Dietary Recommendations
Diet is key for NAFLD, and balance is key. Eat plenty of fruits, veggies, whole grains, and good fats from nuts and olive oil. Try to eat less sugar, carbs, and alcohol since they can lead to NAFLD. A Mediterranean-style diet is good for your liver and can lower your risks for liver disease and cancer.
Regular Exercise
Moving around a lot helps keep NAFLD in check. Even just walking fast can lower liver fat and make your metabolism work better. Try to exercise for 150 minutes a week, or do 75 minutes of harder exercise. This can help you avoid fatty liver disease.
Read: 5 Ways To Deal With Fatty Liver | Dr Nivedita Pandey
Complications and Long-Term Effects
Nonalcoholic fatty liver disease (NAFLD) starts with a simple problem. It can become a serious issue called nonalcoholic steatohepatitis (NASH). NASH might cause liver scarring, known as cirrhosis. This can lead to liver failure, liver cancer, and more.
If left untreated, NAFLD and NASH become severe. They can harm your health in the long run.
NAFLD is common, affecting nearly a quarter of U.S. adults. NASH is less common but affects up to 6.5% of adults. It’s more likely to develop in older people, those with certain genetic risks, obesity, diabetes, and metabolic syndrome.
The long-term impact of NAFLD and NASH can be severe. They can lead to cirrhosis. This is when the liver has permanent scarring. Cirrhosis brings serious complications like liver cancer and end-stage liver failure.
It is key to prevent NAFLD from getting worse. Managing it effectively can avoid severe consequences. This means keeping a healthy weight, eating right, and staying active. These steps are crucial for controlling NAFLD and reducing risks.
Emerging Trends and Research
Scientists are looking into new ways to find, treat, and stop NAFLD and NASH. They are looking at new biomarkers and imaging methods to find liver disease early. Tests of new drugs for NASH are underway. These drugs aim to fight inflammation, scarring, and problems with how the body uses energy.
They are also studying how bacteria in the gut might affect NAFLD. This could mean using probiotics or bacteria from healthy stool to help. Since NAFLD is becoming more common, the hope is these new ideas will help us fight it better.
The USA is using special guidelines to diagnose and treat NAFLD. They have also come up with ways to check how bad the disease is. This can help doctors choose the right treatments and monitor how the disease changes over time.
For treatment, doctors have looked at using drugs like pioglitazone, vitamin E, and placebos for NASH. While there are no approved drugs specifically for NASH yet, this research shows promise. They are also testing if using MRI scans can replace checking liver samples under a microscope. This could make clinical trials easier and help rate new NAFLD treatments.
More young people are getting NAFLD and NASH, such as in Korea. This makes finding new treatments and ways to manage the disease very important. The ongoing efforts to develop better tests, treatments, and ways to prevent NAFLD offer hope. They aim to improve how we handle this serious health issue in the future.
Special Considerations
Once only seen in adults, nonalcoholic fatty liver disease (NAFLD) is now common in kids and teens too. This change likely links to the growing number of young people with obesity. Kids as young as 2-3 years old can get NAFLD. It’s vital to keep an eye on them and act early to stop serious liver issues.
Children and Adolescents
The number of kids with NAFLD is going up, much like obesity rates. Finding and treating NAFLD early is key. This stops it from getting worse and causing severe liver problems, like nonalcoholic steatohepatitis (NASH) or cirrhosis.
Pregnancy and NAFLD
Expecting mothers with NAFLD or NASH need extra attention. These liver conditions can affect the health of both the mother and the baby. Being pregnant might make NAFLD worse. It also raises the risk of gestational diabetes and preeclampsia. Doctors who specialize in livers (hepatologists) and pregnancy (obstetricians) working together is crucial. They ensure the best results for the mother and her baby.
Living with Nonalcoholic Fatty Liver Disease
If you have nonalcoholic fatty liver disease (NAFLD) or its more severe form, nonalcoholic steatohepatitis (NASH), changing your lifestyle is key. With the right steps, you can manage your health well. This lowers the danger of your condition getting worse over time.
Lifestyle Adjustments
Managing NAFLD starts with a healthy lifestyle. It means keeping a normal weight by eating well and staying active. Choose foods like fruits, veggies, whole grains, and lean meats. Limit or avoid added sugars, white bread, and unhealthy fats. Doing this can cut down on fat in your liver.
Getting moving is also important. Aim for activities like walking fast, swimming, or biking for at least 30 minutes on most days. Avoid or cut down on alcohol. Even small amounts can harm your liver more if you have NAFLD or NASH. Plus, it’s vital to control conditions like diabetes and high blood pressure to stop your liver disease from getting worse.
Monitoring and Follow-up
Keeping an eye on your liver health is a big part of managing NAFLD. You’ll have check-ups that might include blood tests to look at liver function. Doctors might also order scans to see how much fat is in your liver and if there’s any damage. In certain situations, a liver biopsy might be needed to get a detailed look.
Working with your healthcare team is crucial. This team could include a liver specialist, your primary care doctor, and other health professionals. They can guide you on the best ways to treat and monitor NAFLD. With their support, you can take charge of your health and keep your liver in good shape.
Take Charge of Your Liver Health Today
Fatty liver might be silent, but you don’t have to stay in the dark. Whether you’ve just found out about NAFLD or you’re trying to avoid it, the best time to take action is now.
If you’re worried about what causes nonalcoholic fatty liver disease, or want personalized care, book a consultation with Dr. Nivedita Pandey, a U.S.-trained, board-certified Senior Gastroenterologist and Hepatologist. She is the best and specializes in fatty liver treatment, NASH, liver inflammation, obesity-related gut issues, and post-liver transplant care. As one of South Delhi’s few female gastroenterologists, Dr. Pandey offers expert guidance in a comfortable space, especially for women managing hormonal and digestive health issues.
Take the first step. Your liver will thank you.
FAQ
What is nonalcoholic fatty liver disease (NAFLD)?
Nonalcoholic fatty liver disease (NAFLD) is when too much fat builds up in the liver. This happens without drinking a lot of alcohol. It ranges from just having a fatty liver to a more serious form known as nonalcoholic steatohepatitis (NASH). NASH can cause liver scarring and harm.
What are the symptoms of NAFLD?
Usually, NAFLD shows no symptoms. But if it does, signs may be feeling tired, general discomfort, or pain in the upper right belly. NASH and cirrhosis, a liver condition, can lead to worse symptoms like itchy skin, a swollen belly, and difficulty breathing.
What are the risk factors for developing NAFLD?
Main risk factors for NAFLD are being overweight, having an insulin problem, type 2 diabetes, and high blood fats. Certain genetics may also play a role. Conditions such as metabolic syndrome and age can increase risks too.
How is NAFLD diagnosed?
Doctors can find NAFLD by accident with blood tests showing liver enzymes are off. Imaging tests, like ultrasound, CT, and MRI, show fat in the liver. A liver biopsy is the best way to confirm NAFLD and check for damage.
How is NAFLD treated?
Managing NAFLD starts with changing your life. This means losing weight and getting your cholesterol, blood fats, and diabetes under control. For NASH, doctors might also prescribe medicines. No direct medications for NASH exist, but there’s active research.
How can I prevent or manage NAFLD?
The top way to deal with NAFLD is lifestyle changes. Keeping a healthy weight and moving more are key. A diet full of fruits, vegetables, whole grains, and good fats helps. Limiting sugars, carbs, and alcohol is important too.
What are the potential complications of NAFLD?
The biggest worry with NAFLD is it turning into NASH or cirrhosis. These can scar the liver permanently. Over time, that could lead to liver failure, cancer, or other very serious issues.
Are there any special considerations for NAFLD in certain populations?
Yes, more and more kids and teens are getting NAFLD, largely due to obesity. If a pregnant woman has NAFLD or NASH, it can be serious for both her and the baby. Here, teamwork between liver and pregnancy doctors is crucial.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.






