Introduction
Metabolic dysfunction associated steatotic liver disease is one of the most common liver problems today, and it’s growing fast. It is often unnoticeable, revealing few symptoms until the damage has been inflicted. But with the right knowledge, you can catch it early, treat it effectively, and prevent it from coming back.
Table of Contents
ToggleThis guide will help you understand MASLD symptoms, causes, risks, diagnosis, and treatment. We will also talk about how to prevent it and live well with it.
What is MASLD?
MASLD is a liver condition where fat builds up in liver cells without significant alcohol use. It used to be called (nonalcoholic fatty liver disease) NAFLD but got a new name to better reflect its main cause — metabolic dysfunction.
It’s linked to problems like metabolic syndrome and liver health issues, high blood sugar, high blood pressure, and abnormal cholesterol. Many cases are tied to MASLD and obesity, but it can also happen in people with normal weight who have metabolic risk factors liver disease.
This condition develops when the liver stores too much fat (liver fat accumulation), often because the body is resistant to insulin (insulin resistance and liver fat). Over time, the fat can cause liver inflammation, liver fibrosis, and even non-alcoholic steatohepatitis (NASH).
Symptoms and Causes of MASLD
Symptoms
MASLD symptoms are often silent. Many people feel fine until the liver damage gets worse. When signs appear, they may include:
- Tiredness
- Discomfort in the upper right belly
- Trouble focusing
- Mild swelling in the belly or legs
- Yellow skin or eyes (in severe cases)
Causes
The main cause is liver fat accumulation from metabolic risk factors liver disease. These include:
- MASLD and obesity
- Liver disease and type 2 diabetes
- Metabolic syndrome and liver
- Insulin resistance and liver fat
- High cholesterol or triglycerides
- Family history of liver problems (can MASLD be hereditary?)
- Poor diet and lack of activity
In short, the causes of MASLD are linked to how the body processes sugar and fat.
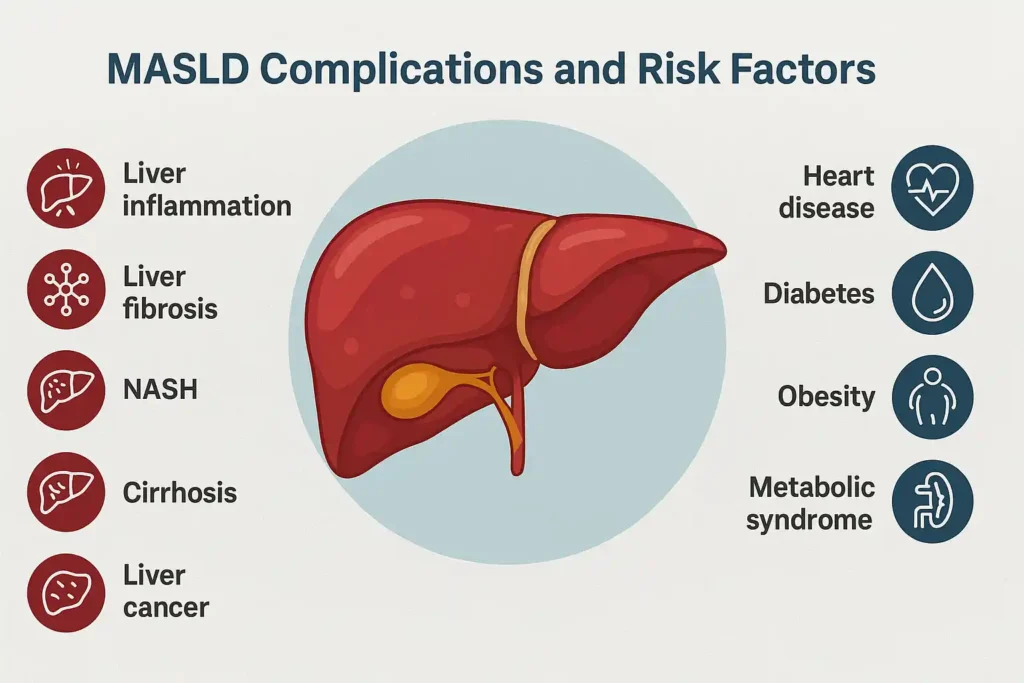
Complications of Metabolic Dysfunction-Associated Steatotic Liver Disease
If left untreated, MASLD can lead to:
- Liver inflammation
- Liver fibrosis (scar tissue)
- Non-alcoholic steatohepatitis (NASH) — a more serious form
- Cirrhosis (severe scarring)
- Liver cancer
- Heart disease
These problems can shorten life and reduce quality of living.
Diagnosis and Tests of MASLD
Blood Tests
Blood tests evaluate liver enzymes in MASLD, particularly ALT and AST levels. High levels can suggest liver stress or damage. Doctors may also check cholesterol, blood sugar, and other metabolic dysfunction markers.
Imaging Tests
An ultrasound is generally the first procedure employed to detect liver steatosis. More advanced imaging, such as FibroScan or MRI, can measure fat levels and check for scarring. These tests are painless and give a clear view of liver health.
Liver Biopsy
A liver biopsy is the most accurate way to diagnose MASLD and check for hepatic fat, inflammation, and scarring. It’s usually done when other tests can’t confirm the cause or stage of liver damage.
Management and Treatment of Metabolic Dysfunction-Associated Steatotic Liver Disease
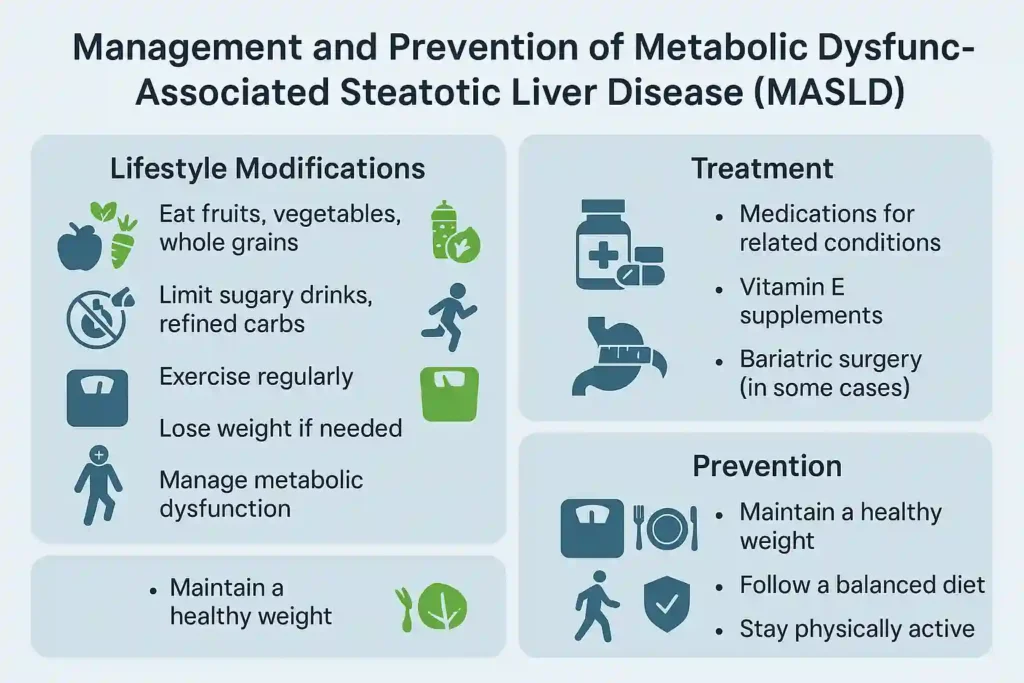
Lifestyle Modifications
The main MASLD treatment is lifestyle intervention for liver disease. This includes:
- Eating more fruits, vegetables, and whole grains
- Cutting sugary drinks and refined carbs
- Regular exercise (at least 150 minutes weekly)
- Losing 7–10% of body weight if overweight
- Managing metabolic dysfunction like high blood sugar or cholesterol
Medications
There’s no direct cure in pill form, but doctors may prescribe medicines for related conditions. For example, diabetes drugs like pioglitazone or GLP-1 agonists can improve liver fat accumulation and inflammation. Vitamin E supplements may help certain patients.
Bariatric Surgery
For severe obesity and advanced MASLD, bariatric surgery can reduce weight and hepatic fat, improve insulin sensitivity, and lower liver enzyme levels. It’s usually considered when lifestyle changes haven’t worked.
Is MASLD Reversible?
Yes, if caught early. Mitigating liver fat accumulation via weight loss, dietary adjustments, and exercise can restore the liver to its normal function. But advanced liver fibrosis may be permanent, making early MASLD diagnosis essential.
Prognosis and Life Expectancy
With early diagnosis and treatment, many people with metabolic dysfunction associated steatotic liver disease live normal lifespans. The danger comes if it progresses to NASH, Liver cirrhosis, or liver cancer.
Life expectancy depends on:
- Stage of liver fibrosis
- How well MASLD guidelines are followed
- Control of related conditions like diabetes and high cholesterol
Research shows that losing 10% of body weight can significantly reduce liver fat, inflammation, and scarring, improving long-term survival.
Prevention
You can lower your risk of MASLD by:
- Keeping a healthy weight
- Eating balanced meals
- Staying active daily
- Controlling blood sugar and cholesterol
- Avoiding unnecessary alcohol
Living With MASLD
Living with MASLD means regular doctor visits, following MASLD guidelines, and sticking to a healthy plan. Support from family, friends, or a dietitian can help.
When to See a Healthcare Provider
See a doctor if you:
- Have MASLD symptoms like unexplained fatigue or belly discomfort
- Have diabetes, high cholesterol, or high blood pressure
- Have a family history of liver problems
- Notice yellowing of the eyes or skin
Conclusion
MASLD is common, but you can take control. With early MASLD diagnosis and the right steps, the liver can heal. Managing weight, blood sugar, and lifestyle habits will not only protect your liver but also your heart and overall health. Don’t wait for symptoms; take action today to protect your liver.
Frequently Asked Questions
Does alcohol cause MASLD?
No. MASLD develops in people who drink little or no alcohol and is linked mainly to metabolic health problems, not alcohol use.
Can lifestyle changes really reverse MASLD?
Yes. Weight loss, healthy diet, and regular activity can reduce liver fat accumulation and reverse early stages of MASLD.
Is MASLD the same as NAFLD?
Yes. MASLD is the updated term for NAFLD (nonalcoholic fatty liver disease), highlighting its link to metabolic dysfunction.
Can MASLD occur in people who are not overweight?
Yes. Even people with normal weight can develop MASLD if they have metabolic dysfunction or insulin resistance.
What’s the difference between MASLD and MASH?
MASH is a more severe stage of MASLD where there’s inflammation and damage, similar to non-alcoholic steatohepatitis (NASH).
How often should I get tested if I have risk factors for MASLD?
Yearly liver enzyme and imaging checks are recommended if you have metabolic risk factors.
What foods should I avoid if I have MASLD?
Avoid sugary drinks, refined carbs, fried foods, and processed meats to protect your liver.
Can MASLD be hereditary?
Yes. Genes can increase risk, especially when combined with poor diet and lifestyle.
Can children get MASLD?
Yes. Poor diet and inactivity can lead to MASLD in adults and children alike.
Is MASLD contagious?
No. It cannot spread from one person to another.
Do I need to see a liver specialist (hepatologist) if I have MASLD?
Yes, especially if you have advanced disease or unclear MASLD diagnosis results.
Does MASLD cause pain?
Sometimes. Discomfort in the upper right abdomen can happen, but many cases have no pain.
Can MASLD come back after being reversed?
Yes. It can return if unhealthy habits and weight gain resume.
Can MASLD affect pregnancy?
Yes. It may raise risks for gestational diabetes and pregnancy complications.
Will MASLD affect my eligibility for a liver transplant?
Yes. Eligibility depends on the severity of liver damage and overall health.
About The Author

This article is medically reviewed by Dr. Nivedita Pandey, Senior Gastroenterologist and Hepatologist, ensuring accurate and reliable health information.
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist specializing in pre and post-liver transplant care, as well as managing chronic gastrointestinal disorders. Known for her compassionate and patient-centered approach, Dr. Pandey is dedicated to delivering the highest quality of care to each patient.
→ Book a consultation to discover which remedies suit your needs best.
About Author | Instagram | Linkedin