Diverticulosis, diverticulitis, and diverticular disease are common conditions that affect the colon. It’s important to have a clear understanding of these terms and their complications. Diverticulosis refers to the development of small pouches in the colon wall, while diverticulitis occurs when these pouches become inflamed. Diverticular disease is an umbrella term that encompasses chronic symptoms, diverticular bleeding, and diverticulitis.
Table of Contents
ToggleDiverticulosis is quite common, especially as people age. In fact, more than 30% of adults between the ages of 50 and 59 and over 70% of those older than 80 have diverticulosis. However, only a small percentage of people with diverticulosis develop diverticulitis. In the United States, around 200,000 people are hospitalized for diverticulitis each year.
The complications of diverticular disease can be serious and may include diverticular bleeding, abscess, fistula, intestinal obstruction, perforation, and peritonitis. It is essential to be aware of these potential complications and seek medical attention if any symptoms arise.
What is Diverticulosis?
Diverticulosis is a common condition that involves the formation of small pouches or diverticula in the wall of the colon, particularly in the sigmoid colon. These pouches, known as diverticulum in the case of a single pouch or diverticula in the case of multiple pouches, are often asymptomatic, meaning they do not cause noticeable symptoms or problems for most individuals.
However, it is important to note that diverticulosis can vary from person to person, and in some cases, these pouches may lead to symptoms or inflammation. Although asymptomatic diverticulosis is the most common presentation, it is essential to be aware of potential complications and remain vigilant for any changes or discomfort experienced in the abdomen.
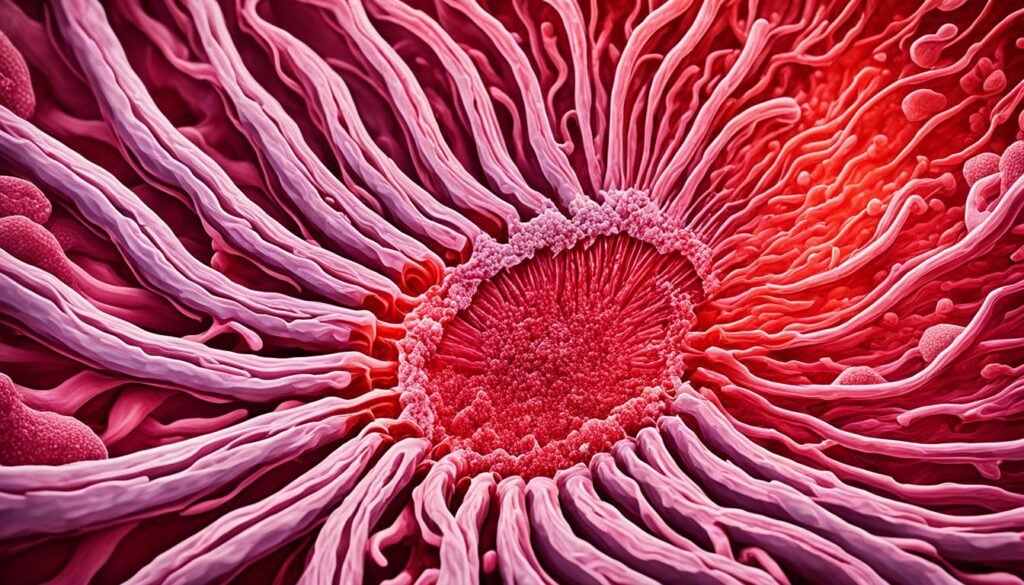
As shown in the image below, diverticula typically develop along the wall of the sigmoid colon, the ‘S’ shaped portion of the large intestine:

If you would like to learn more about diverticulosis and its impact on gut health, continue reading as I delve into the various aspects of this condition and provide valuable insights into its management and prevention.
What is Diverticulitis?
Diverticulitis occurs when the diverticula become inflamed, which can happen suddenly and lead to serious complications. Common symptoms of diverticulitis include constant and often severe abdominal pain, usually on the left side, but occasionally on the right side, fever, nausea, vomiting, changes in bowel habits such as constipation or diarrhea. Diverticulitis can be a painful and debilitating condition that requires medical attention.
What is Diverticular Disease?
Diverticular disease encompasses a range of conditions that can arise from diverticula, including chronic symptoms, diverticular bleeding, and diverticulitis complications.
Chronic symptoms of diverticular disease may include:
- Episodes of pain in the lower abdomen
- Changes in bowel habits
- Constipation
- Diarrhea
- Small amounts of blood in stools
Diverticular bleeding occurs when a blood vessel within a diverticulum bursts, leading to bleeding in the lower digestive tract.
Diverticulitis, another complication of diverticular disease, can cause the following complications:
- Abscess: a painful, swollen, pus-filled area caused by infection
- Fistula: an abnormal passage between the colon and another part of the body
- Intestinal obstruction
- Bowel perforation: a hole in the colon
- Peritonitis: an infection of the abdominal cavity lining
| Type of Complication | Description |
|---|---|
| Abscess | A painful, swollen, pus-filled area caused by infection |
| Fistula | An abnormal passage between the colon and another part of the body |
| Intestinal Obstruction | Blockage of the intestine that prevents the normal movement of food and waste |
| Bowel Perforation | A hole in the colon |
| Peritonitis | An infection of the abdominal cavity lining |
How Common is Diverticulosis, Diverticulitis, and Diverticular Disease?
Diverticulosis is a prevalent condition, especially among older adults. More than 30% of adults between the ages of 50 and 59 and over 70% of those older than 80 have diverticulosis in the United States.
However, it’s important to note that most people with diverticulosis will never develop symptoms or encounter any problems related to the condition.
On the other hand, diverticulitis, which is the inflammation of the diverticula, is relatively less common. Less than 5% of people with diverticulosis go on to develop diverticulitis.
Despite its lower prevalence, diverticulitis can still lead to significant health issues, and hospitalizations for diverticulitis are not uncommon. Around 200,000 people are hospitalized for diverticulitis in the United States annually.
Additionally, diverticular bleeding, another complication of diverticular disease, affects a significant number of individuals. Approximately 71,000 people are hospitalized for diverticular bleeding each year.
Who is More Likely to Have Diverticulosis, Diverticulitis, and Diverticular Disease?
The likelihood of developing diverticulosis and diverticulitis increases with age. Among individuals younger than 50 years, diverticulitis is more common in men, while among people aged 50 and older, diverticulitis is more common in women. Additionally, there are racial disparities in the prevalence of these conditions.
Age
Age is a significant factor in the development of diverticulosis and diverticulitis. As individuals grow older, their risk of developing these conditions increases. Diverticulosis is more prevalent among individuals over the age of 50, with more than 30% of adults between the ages of 50 and 59 affected and over 70% of those older than 80.
Gender
The gender distribution of diverticulitis varies depending on age. Among individuals younger than 50 years, diverticulitis is more common in men. However, among individuals aged 50 and older, diverticulitis is more common in women. The reasons for these gender differences are not yet fully understood, and further research is needed.
Racial Disparities
Racial disparities exist in the prevalence of diverticulosis and diverticular disease. In the United States, diverticulitis is more common in white Americans compared to other racial or ethnic groups. Conversely, diverticular bleeding, a complication of diverticular disease, is more common in Black Americans. These disparities suggest potential differences in risk factors or genetic predispositions among different racial and ethnic populations.
| Demographic | Diverticulosis | Diverticulitis | Diverticular Bleeding |
|---|---|---|---|
| Age | More prevalent in individuals over 50 | More common in individuals over 50, especially women | No specific age group prevalence |
| Gender | No significant gender differences | More common in men (under 50) and women (over 50) | No specific gender prevalence |
| Race/Ethnicity | No significant disparities | More common in white Americans | More common in Black Americans |
What Are the Complications of Diverticular Disease?
Diverticular disease can lead to various complications that require immediate medical attention. These complications include:
- Diverticular Bleeding: When a blood vessel within a diverticulum bursts, it can cause bleeding in the lower digestive tract.
- Abscess: Diverticulitis can result in the formation of a painful and swollen area filled with pus due to infection.
- Fistula: Diverticulitis can lead to the development of an abnormal passage between the colon and another part of the body.
- Intestinal Obstruction: In some cases, diverticulitis can cause a blockage in the intestine, leading to symptoms such as severe abdominal pain and constipation.
- Perforation: Diverticulitis can cause a hole or perforation in the colon, which can result in serious complications.
- Peritonitis: An infection of the abdominal cavity lining can occur if the perforation of the colon leads to the leakage of fecal matter into the abdominal cavity.
These complications can be serious and may require surgery or other interventions to treat and manage effectively.
Causes and Risk Factors of Diverticulitis
The exact cause of diverticulitis is unknown, but it is believed to be related to weak spots in the colon that develop as a result of a lack of dietary fiber. Without enough fiber, stools become hard, increasing pressure and strain on the colon. This can cause the development of diverticula.
Risk factors for diverticulitis include:
- Age: Diverticulitis is more common as people get older.
- Obesity: Excess weight can increase the risk of diverticulitis.
- Smoking: Smoking has been associated with an increased risk of diverticulitis.
- Lack of exercise: Sedentary lifestyle and lack of physical activity can contribute to the risk of diverticulitis.
In addition to these factors, a diet high in animal fat and low in dietary fiber is also associated with an increased risk of developing diverticulitis.
It’s important to address these risk factors through lifestyle modifications and dietary changes to reduce the likelihood of developing diverticulitis or experiencing recurrent episodes.
Diagnosing Diverticulitis
Diagnosing diverticulitis can be challenging and may involve various tests and procedures. When evaluating a patient for diverticulitis, healthcare professionals consider symptoms, medical history, and perform specific diagnostic tests. These tests help confirm the diagnosis and determine the severity of the condition. Some common diagnostic methods include:
- Blood tests: Blood tests are conducted to identify signs of infection in the body. Elevated levels of white blood cells and C-reactive protein (CRP) can indicate inflammation or infection, which are indicative of diverticulitis.
- Colonoscopy: A colonoscopy involves using a thin, flexible tube with a camera, known as a colonoscope, to visualize the inside of the colon. This procedure allows doctors to directly examine the colon, identify any abnormalities, and rule out other conditions.
- Barium enema X-ray: A barium enema X-ray is a diagnostic procedure where a contrast material called barium is inserted into the rectum. The barium fills the colon, and X-rays are taken to create detailed images. This test helps evaluate the presence of diverticula and any associated complications.
- CT scan: A computed tomography (CT) scan is often the most effective diagnostic tool for diverticulitis. It provides detailed cross-sectional images of the abdomen and pelvis, allowing doctors to visualize the diverticula and assess the severity of inflammation. CT scans can help determine the presence of complications such as abscesses or perforations.
During the diagnostic process, it is important to consider the patient’s symptoms and medical history. These factors, combined with the results of diagnostic tests, help healthcare professionals accurately diagnose diverticulitis and develop an appropriate treatment plan.
Treating Diverticulosis and Diverticulitis
Mild cases of diverticulosis can often be managed through self-treatment. When experiencing pain, acetaminophen can be taken as a pain management option. Additionally, increasing dietary fiber intake can help soften stools and regulate bowel movements, reducing discomfort and symptoms. Including fiber-rich foods such as whole grains, fruits, and vegetables in your daily diet can promote digestive health and prevent future episodes of diverticulosis.
When it comes to diverticulitis, treatment may involve a combination of antibiotics, pain medication, and a special diet. Antibiotics are prescribed to address the infection and reduce inflammation. Pain medication, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate discomfort. A special diet consisting of low-fiber or liquid foods may be recommended to rest the colon and allow it to heal.
However, in severe or recurring cases of diverticulitis, surgical intervention may be necessary. Surgery involves removing the affected part of the colon to prevent future complications and improve overall intestinal health. Your healthcare provider will evaluate your condition and recommend the most suitable treatment plan based on your individual needs and the severity of your diverticular disease.
Comparison of Self-Treatment and Medical Interventions for Diverticulosis and Diverticulitis
| Treatment Options | Self-Treatment | Medical Interventions |
|---|---|---|
| Pain Management | Acetaminophen | Pain medication (NSAIDs) |
| Dietary Fiber | Increasing intake of fiber-rich foods | Special low-fiber or liquid diet |
| Antibiotics | N/A | Prescribed to address infection |
| Surgery | N/A | Removal of affected part of the colon |
It is important to consult with your healthcare provider before attempting self-treatment. Proper diagnosis and guidance from a medical professional can ensure effective management of diverticulosis and diverticulitis.
Conclusion
Managing diverticulitis and diverticular disease can be a challenging journey, but with knowledge of symptoms, causes, and treatment options, individuals can take control of their condition and improve their gut health. It is crucial for those with diverticulosis or diverticulitis to work closely with healthcare professionals to develop a personalized treatment plan that caters to their specific needs.
By adopting a healthy lifestyle that includes a high-fiber diet and regular exercise, individuals can significantly reduce the risk of complications and promote overall well-being. The inclusion of dietary fiber helps soften stools and regulate bowel movements, while regular physical activity supports digestive health.
In cases of diverticulitis, treatment options may involve antibiotics to address the infection, pain medication for symptom management, and a special diet. However, severe or recurring cases may require surgical intervention to remove the affected part of the colon.
FAQ
What is diverticulosis?
Diverticulosis is a condition characterized by the formation of small pouches or diverticula in the colon wall, most commonly in the sigmoid colon. It is often asymptomatic and doesn’t typically cause problems for most people.
What is diverticulitis?
Diverticulitis occurs when the diverticula become inflamed, causing symptoms such as constant and often severe abdominal pain, fever, nausea, and changes in bowel habits. It can be a painful and debilitating condition that requires medical attention.
What is diverticular disease?
Diverticular disease is an umbrella term that encompasses chronic symptoms, diverticular bleeding, and diverticulitis complications. Chronic symptoms may include episodes of pain in the lower abdomen, changes in bowel habits, and small amounts of blood in stools.
How common is diverticulosis, diverticulitis, and diverticular disease?
Diverticulosis is quite common, especially among older adults. More than 30% of U.S. adults between the ages of 50 and 59 and over 70% of those older than 80 have diverticulosis. Less than 5% of people with diverticulosis develop diverticulitis. In the United States, around 200,000 people are hospitalized for diverticulitis each year. Additionally, approximately 71,000 people are hospitalized for diverticular bleeding annually.
Who is more likely to have diverticulosis, diverticulitis, and diverticular disease?
The likelihood of developing diverticulosis and diverticulitis increases with age. Among individuals younger than 50 years, diverticulitis is more common in men, while among people aged 50 and older, diverticulitis is more common in women. In the United States, diverticulitis is more common in white Americans than in other racial or ethnic groups, and diverticular bleeding is more common in Black Americans.
What are the complications of diverticular disease?
Complications of diverticular disease include diverticular bleeding, abscess, fistula, intestinal obstruction, perforation, and peritonitis. These complications can be serious and require immediate medical attention.
What are the causes and risk factors of diverticulitis?
The exact cause of diverticulitis is unknown, but it is believed to be related to weak spots in the colon that develop as a result of a lack of dietary fiber. Risk factors for diverticulitis include age, obesity, smoking, and lack of exercise. A diet high in animal fat and low in fiber is also associated with an increased risk of developing diverticulitis.
How is diverticulitis diagnosed?
Diagnosing diverticulitis can involve various tests and procedures. Blood tests can help identify signs of infection, while a colonoscopy allows a doctor to examine the colon using a thin tube with a camera. A barium enema X-ray can provide an image of the colon, and a CT scan is often the most helpful in diagnosing diverticulitis and determining the severity of the infection. Diagnosing diverticulitis also involves considering symptoms and medical history.
How is diverticulosis and diverticulitis treated?
Mild cases of diverticulosis can often be managed through self-treatment, including pain management with acetaminophen and increasing dietary fiber intake. For diverticulitis, treatment may involve antibiotics to address the infection, pain medication, and a special diet. In severe or recurring cases of diverticulitis, surgery may be necessary to remove the affected part of the colon.
Source Links


