Hi, I’m here to share some helpful tips on managing diverticulitis through diet. Diverticulitis is a condition that involves the inflammation of small pouches in the colon, causing discomfort and pain. While there is some debate about the best diet for diverticulitis, certain foods are recommended to avoid to help alleviate symptoms and promote digestive health.
Table of Contents
ToggleIt is of utmost importance to seek the guidance of a healthcare professional before embarking on any significant dietary changes. Their expertise and personalised advice based on your specific needs will provide you with the reassurance and confidence you need to manage diverticulitis effectively. In the meantime, here are 7 foods to avoid with diverticulitis.
The Best Diet for Diverticulitis
The best diet for diverticulitis is a healthy and balanced one that includes a variety of fruits, vegetables, proteins, and healthy fats. This type of diet provides essential nutrients and promotes overall digestive health.
It is important to note that doctors are divided regarding dietary recommendations for diverticulitis. While some believe avoiding certain foods can help reduce inflammation and irritation, others may have different opinions. Therefore, working with a healthcare professional or registered dietitian is crucial to safely adjusting your diet based on your needs and preferences.
A healthy diet for diverticulitis typically emphasizes the following:
- High-fiber foods are a cornerstone of a diverticulitis-friendly diet. They play a crucial role in promoting regular bowel movements and preventing constipation. However, it’s important to introduce fiber gradually and ensure adequate hydration to avoid discomfort. High-fiber foods include whole grains, legumes, fruits, and vegetables.Plenty of fluids: Staying hydrated is essential for maintaining good digestive health. Drinking adequate water throughout the day helps soften stool and prevents constipation.
- Lean proteins: Choose lean protein sources, such as poultry, fish, tofu, and beans. These options provide essential nutrients without excess fat.
- Healthy fats: Include sources of healthy fats in your diet, such as avocados, nuts, seeds, and olive oil. These fats can help reduce inflammation and support overall health.
Remember, everyone’s dietary needs and preferences may vary. By working with a healthcare professional or a registered dietitian, you can develop a flexible and personalised plan that aligns with your specific needs and ensures a balanced approach to managing diverticulitis symptoms. This flexibility empowers you to take control of your health and make choices that work best for you.
Key Takeaways:
When it comes to the best diet for diverticulitis:
- Focus on a healthy and balanced diet that includes fruits, vegetables, proteins, and healthy fats.
- Consult with a healthcare professional for personalized dietary recommendations.
- Gradually introduce high-fiber foods and drink plenty of water to avoid discomfort.
- Make sure to tailor your diet to your individual needs and preferences.
Here Are The 7 Foods To Avoid With Diverticulitis & There Alternatives
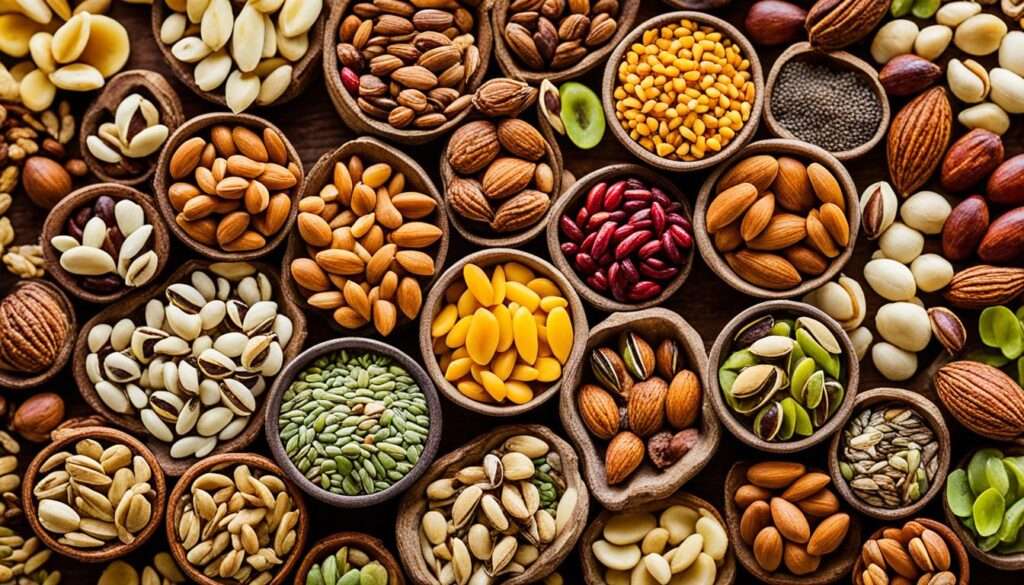
Seeds and Nuts
Diet plays a crucial role in managing diverticulitis. While high-fiber foods are generally recommended for a healthy digestive system, they can pose challenges for individuals with diverticulitis. Seeds and nuts, in particular, can be difficult to digest and may get lodged in the diverticula, leading to worsening symptoms.
Plenty of other nutritious alternatives are more accessible to digest and less likely to trigger symptoms than seeds and nuts. Including a variety of whole fruits such as bananas, apples, and oranges can provide the necessary fiber and nutrients without potential complications. Vegetables like carrots, broccoli, and cauliflower are also excellent options. Additionally, incorporating whole grains like quinoa, brown rice, and oats into your diet can offer fiber and essential nutrients.
By making these substitutions, individuals with diverticulitis can still enjoy a balanced, fiber-rich diet while minimizing the risk of discomfort and inflammation. These dietary changes can significantly improve your symptom management, giving you hope and optimism for a healthier future. It is important to remember that dietary management for diverticulitis may vary from person to person, so consulting with a healthcare professional or dietitian for personalized guidance is advised.
Diverticulitis-friendly Foods to Include:
- Whole fruits: bananas, apples, oranges
- Vegetables: carrots, broccoli, cauliflower
- Whole grains: quinoa, brown rice, oats
Substitutes for Seeds and Nuts
| Seeds and Nuts | Diverticulitis-friendly Alternatives |
|---|---|
| Chia Seeds | Ground Flaxseeds |
| Almonds | Sliced Avocado |
| Pumpkin Seeds | Steamed Broccoli |
| Walnuts | Blueberries |
Popcorn
During a diverticulitis flare-up, consuming popcorn can be challenging due to its high fiber content. The hulls of popcorn kernels can get trapped in the diverticula, causing irritation and potentially leading to inflammation. If you still want to enjoy popcorn, it is essential to chew it thoroughly to ensure easier digestion and reduce the risk of complications. Alternatively, consider opting for other crunchy snacks like pretzels that are gentler on the digestive system.
Popcorn Substitutes:
If you love snacking on popcorn but need to avoid it due to diverticulitis, here are a few alternatives:
- Pretzels
- Rice cakes
- Baked potato chips
- Crispy roasted chickpeas
These crunchy snacks can satisfy your cravings while minimizing the risk of diverticulitis complications. Always consult your healthcare professional or dietitian for personalized dietary recommendations.
Spicy Foods
Spicy foods can be incredibly tempting but can also be troublesome for individuals with diverticulitis. The heat from foods like hot sauces, chilies, wasabi, and curry dishes can irritate the already sensitive digestive system, potentially worsening diverticulitis symptoms. It’s essential to be mindful of these triggers, as they can lead to painful flares.
If you’re looking to add flavor to your meals without the risk of inflammation, consider using alternative spices that are milder and less likely to aggravate your condition. Some great options include herbs like basil, oregano, and thyme and mild spices like cumin and paprika. These alternatives can help you enjoy delicious meals while keeping your diverticulitis in check.

Spices and Herbs for a Diverticulitis-Friendly Diet
| Spice/Herb | Description |
|---|---|
| Basil | A fragrant herb that adds a hint of sweetness and freshness to dishes. |
| Oregano | A robust herb used in many Mediterranean dishes, known for its earthy flavor. |
| Thyme | A versatile herb with a slightly minty and lemony taste, perfect for enhancing savory dishes. |
| Cumin | A warm spice with a nutty flavor profile, commonly used in Indian, Middle Eastern, and Mexican cuisine. |
| Paprika | A mild spice made from dried and ground bell peppers, ideal for adding color and depth to dishes without overpowering the taste. |
Fried Foods
When managing diverticulitis, paying attention to the types of foods you consume is essential. Fried foods, in particular, can be problematic for those with diverticulitis due to their high fat content. These foods are challenging to digest and can contribute to inflammation and discomfort in the abdomen.
Eating a diet high in fried foods has been linked to an increased risk of constipation, which can strain the colon and potentially lead to the development of diverticula. Limiting or avoiding fried foods is recommended to support optimal digestive health and minimize the risk of flare-ups.
Effects of Fried Foods on Diverticulitis
The consumption of fried foods can have several adverse effects on individuals with diverticulitis:
- High Fat Content: Fried foods are typically high in unhealthy fats, such as saturated and trans fats. These fats can be challenging to digest and may lead to discomfort and bloating.
- Inflammation: The frying process can produce harmful compounds called advanced glycation end products (AGEs), which are associated with increased inflammation in the body.
- Colon Strain: A diet rich in fried foods can contribute to constipation, placing additional strain on the colon. This strain can increase the risk of diverticula formation and exacerbate existing symptoms.
Individuals with diverticulitis can help reduce inflammation, promote better digestion, and support overall digestive health by avoiding or minimizing the consumption of fried foods. Instead, focus on incorporating more nutritious options, such as lean proteins, fruits, vegetables, whole grains, and healthy fats.
Red Meat
Red meat’s impact on the digestive system should be carefully considered when managing diverticulitis. It is harder to digest than poultry. Red meat can contribute to inflammation in the digestive tract, which may worsen diverticulitis symptoms. Research has shown that high consumption of red meat can increase the risk of both irritating symptoms and the development of diverticulitis itself.
If you’re looking to support your digestive health while managing diverticulitis, consider leaner meats and poultry as alternatives to red meat. These options can be easier to digest and provide essential nutrients without the potential drawbacks associated with red meat consumption.

Dairy Products
Dairy products can be a bit tricky when managing diverticulitis. People with diverticulitis may experience discomfort such as bloating, gas, and diarrhea after consuming dairy products. There are two main reasons for this: possible lactose intolerance and the high-fat content in dairy.
Lactose intolerance occurs when the body has difficulty digesting lactose, the sugar found in milk and other dairy products. This can lead to digestive discomfort and symptoms such as diarrhea, exacerbating individuals with diverticulitis’s already sensitive digestive system.
Dairy products can also be high in fat and lactose. High-fat foods, including full-fat milk, cheese, and yogurt, can cause bloating and gas, which can be particularly uncomfortable for those with diverticulitis.
To manage symptoms, it is recommended to choose low-fat or non-fat dairy options. These alternatives are typically easier to digest and have a lower fat content, which can help reduce discomfort. Moderating the intake of dairy products can also be beneficial, as it allows for better control of symptoms.
When selecting dairy products, Greek yogurt and lactose-free milk are good options for individuals with lactose intolerance. These alternatives provide the benefits of dairy without the potential digestive issues.
If you are unsure about your tolerance to dairy products or need additional guidance on modifying your diet, consult your healthcare professional or a registered dietitian who can provide personalized advice.
Refined Grains and Sugars
When managing diverticulitis, it is essential to pay attention to the types of grains and sugars you consume. While whole grains can be beneficial for preventing constipation and reducing the risk of developing diverticulitis, refined grains, and sugars are best avoided. Let’s take a closer look at why.
The Impact of Refined Sugars
Refined sugars are highly inflammatory and can irritate diverticulitis symptoms, significantly increasing the risk of diarrhea. Consuming foods high in refined sugars, such as candy, pastries, and sugary beverages, can exacerbate inflammation in the digestive system and lead to discomfort.
The Role of Whole Grains
On the other hand, whole grains like brown rice, quinoa, and whole wheat bread can provide essential nutrients and fiber and promote regular bowel movements, thereby reducing the risk of constipation. Including these foods in your diet can support overall digestive health and help manage diverticulitis.
However, during a diverticulitis flare-up, refined grains may be easier to digest and provide relief. Consultation with a doctor or dietitian is crucial to receive personalized advice and guidance on the best grain choices during these times.
Remember, dietary management for diverticulitis can vary between individuals. Making informed choices about refined grains and sugars can better support your digestive health and reduce the risk of exacerbating diverticulitis symptoms.
The Importance of a Healthy Diet
In addition to avoiding certain foods, maintaining a healthy diet is crucial for optimal digestive health, especially when dealing with diverticulitis. A balanced diet can help reduce inflammation, improve bowel movements, and prevent complications. Here are some key points to consider:
1. Stay Hydrated
Drinking adequate water throughout the day is essential to prevent dehydration and maintain healthy bowel movements. Proper hydration helps soften stool, making it easier to pass and reducing the risk of constipation, which can aggravate diverticulitis symptoms. Aim to drink at least eight glasses of water daily to support your digestive health.
2. Include High-Fiber Foods
A healthy diet for diverticulitis should include a variety of high-fiber foods such as fruits, vegetables, and whole grains. These fibrous foods promote regular bowel movements, prevent constipation, and reduce the risk of developing diverticula. Some fiber-rich options to consider include:
- Fresh fruits like apples, berries, and pears
- Leafy green vegetables such as spinach and kale
- Whole grains like oats, quinoa, and brown rice
However, gradually increasing your fiber intake is essential to avoid sudden changes in your digestive system. Start with small portions and monitor your body’s response.
3. Cook Homemade Meals
Preparing homemade meals gives you more control over the ingredients you use. This allows you to choose nutritious, fresh, gentle ingredients for your digestive system. Cook meals using methods like grilling, baking, or steaming to minimize the use of added fats and oils. Homemade meals can also help you avoid processed foods containing harmful additives or preservatives.
4. Be Mindful of Personal Triggers
While there are general guidelines for a healthy diet, you must be aware of your triggers. Keep a food diary to track how different foods affect your diverticulitis symptoms. If you notice that certain foods worsen your symptoms, avoiding or limiting their consumption is best. Consulting with a healthcare professional or registered dietitian can provide additional guidance on identifying and managing personal triggers.

Remember, your diet plays a significant role in managing diverticulitis. You can support your digestive health and minimize symptoms by staying hydrated, including high-fiber foods, cooking homemade meals, and being mindful of personal triggers.
Physical Activity and Laxative Medication
Physical activity is crucial in managing diverticulitis and maintaining a healthy digestive system. Regular exercise helps prevent constipation and promotes healthy bowel movements. Engaging in activities such as brisk walking, jogging, cycling, or yoga can enhance the overall function of the colon and reduce the risk of diverticulitis flare-ups.
If dietary changes alone are insufficient to regulate bowel movements, a doctor may recommend using laxative medication. Laxatives, particularly bulk-forming laxatives, can help soften stool and promote regularity. They follow medical advice and guidelines while taking laxatives, essential to ensure their safe and effective use.
Staying well-hydrated is of the utmost importance when utilizing laxative medication. Adequate fluid intake can support the effectiveness of laxatives and aid in maintaining healthy bowel movements. Drinking enough water throughout the day is recommended, as dehydration can exacerbate constipation and hinder the benefits of laxative use.
Remember that physical activity and laxative medication should be incorporated into an individualized treatment plan in consultation with a healthcare professional or gastroenterologist. By combining regular exercise and appropriate use of laxatives, you can effectively manage diverticulitis and promote a healthy digestive system.
Conclusion
Managing diverticulitis through dietary choices is crucial for individuals with this condition. While there are specific foods to avoid, it is essential to remember that dietary management can vary for each person. Consulting with a healthcare professional or dietitian is necessary to develop a personalized plan that considers individual needs and triggers.
Individuals can better manage their diverticulitis symptoms and support their overall digestive health by making educated dietary choices. This includes avoiding high-fiber foods like seeds, nuts, popcorn, spicy foods, fried foods, and red meat. Moderating the intake of dairy products, refined grains, and sugars can also be beneficial.
In addition to dietary changes, adequate water intake is crucial for softening stool and reducing the risk of constipation. Staying well-hydrated and maintaining a regular physical activity routine can also help promote healthy bowel movements. Alongside these lifestyle adjustments, being mindful of personal triggers and working closely with healthcare professionals can help individuals effectively manage their diverticulitis symptoms and improve their quality of life.
FAQ
What are some foods to avoid with diverticulitis?
Certain foods can exacerbate diverticulitis symptoms and should be avoided. These include high-fiber foods like seeds and nuts, popcorn, spicy foods, fried foods, red meat, dairy products, and refined sugars.
What is the best diet for diverticulitis?
The best diet for diverticulitis is generally healthy and balanced. It should include a variety of fruits, vegetables, proteins, and healthy fats. However, doctors debate specific dietary recommendations for diverticulitis.
Why should I avoid seeds and nuts with diverticulitis?
High-fiber foods like seeds and nuts can be difficult to digest. They may get stuck in the diverticula, exacerbating symptoms of diverticulitis. It is recommended to substitute these foods with easier-to-digest alternatives like whole fruits, carrots, broccoli, cauliflower, and whole grains.
Can I eat popcorn if I have diverticulitis?
With its high fiber content, popcorn can be challenging to digest during a diverticulitis flare-up. The kernel hulls can also get stuck in the diverticula, leading to irritation and potential inflammation. If you choose to eat popcorn, chew it thoroughly and consider swapping it for other crunchy snacks like pretzels.
Should I avoid spicy foods if I have diverticulitis?
Spicy foods can irritate the digestive system, potentially worsening diverticulitis symptoms. Hot sauces, chilies, wasabi, and curry dishes can all trigger flare-ups. To add flavor to your meals without the heat, try using other spices that are less likely to cause inflammation.
Why should I limit or avoid fried foods with diverticulitis?
Fried foods, with their high-fat content, can be challenging to digest and may cause inflammation and discomfort in the abdomen. Eating a diet high in fried foods has been linked to an increased risk of constipation, which can strain the colon and contribute to the development of diverticula.
Is red meat rotten for diverticulitis?
Red meat, harder to digest than poultry, can contribute to inflammation in the digestive tract and potentially worsen diverticulitis symptoms. Research has even shown that high consumption of red meat increases the risk of both irritating symptoms and the development of diverticulitis itself. Consider opting for leaner meats and poultry to support digestive health.
Can I still consume dairy products if I have diverticulitis?
Dairy products like yogurt, cheese, and milk can be problematic for people with diverticulitis. Their high-fat content and possible lactose intolerance may cause bloating, diarrhea, and gas. Choosing low-fat dairy options or moderating intake can help manage symptoms.
Are refined grains and sugars allowed in a diverticulitis diet?
Refined sugars are highly inflammatory and can irritate diverticulitis symptoms, remarkably increasing the risk of diarrhea. On the other hand, whole grains can be beneficial for preventing constipation and reducing the risk of developing diverticulitis. Refined grains may be easier to digest during a flare-up and provide relief. Consult with a doctor or dietitian for personalized advice.
What is the importance of a healthy diet for diverticulitis?
In addition to avoiding certain foods, following a generally healthy diet is important for optimal digestive health. This includes staying hydrated by drinking enough water throughout the day. Adequate fluid intake helps soften stool and reduces the risk of constipation, which can contribute to diverticulitis. It is also essential to be mindful of personal triggers and to cook homemade meals when possible.
Can physical activity and laxatives help with diverticulitis?
Regular physical activity can help prevent constipation and maintain healthy bowel movements. If dietary changes are insufficient, a doctor may recommend laxative medication, typically a bulk-forming laxative, to help regulate bowel movements. It is important to follow medical advice and stay well-hydrated when taking laxatives.
Why is dietary management important for diverticulitis?
While there are specific foods to avoid with diverticulitis, it is important to remember that dietary management for the condition can vary. Consulting with a healthcare professional or dietitian is essential to develop a personalized plan that takes into account individual needs and triggers. By making educated dietary choices and tracking water intake, individuals can better manage their diverticulitis symptoms and support their overall digestive health.
Source Links
- https://www.mkuh.nhs.uk/patient-information-leaflet/dietary-advice-for-diverticular-disease
- https://www.kentcht.nhs.uk/leaflet/diverticular-disease-and-diet/


