Liver parenchymal disease is damage to the liver’s working cells (hepatocytes) that reduces how the liver cleans blood, makes bile, stores nutrients, and helps blood clot. You should know common causes, early signs, and the tests doctors use so you can act early and reduce harm.
Table of Contents
ToggleWhat Is Liver Parenchymal Disease?
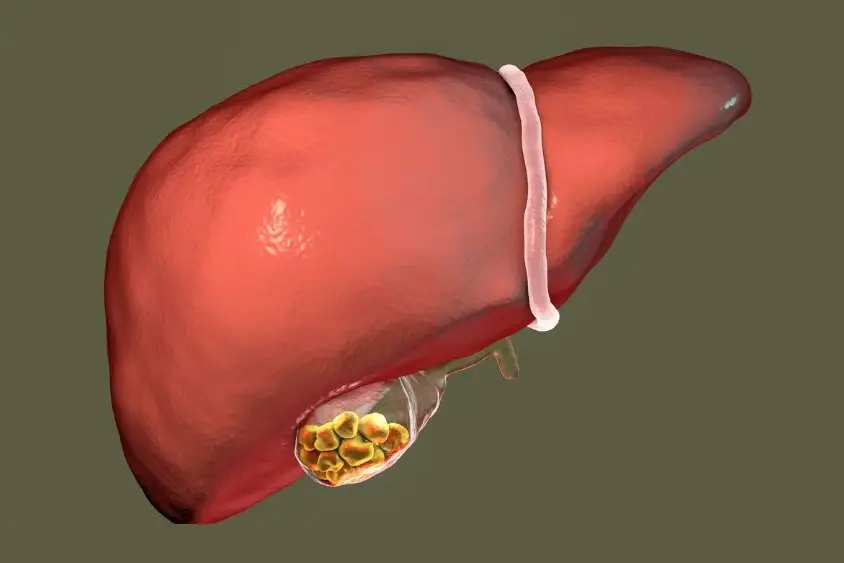
Definition of liver parenchyma
The liver parenchyma refers to the main liver tissue made of hepatocytes. These cells do most liver work: break down toxins, store sugar as glycogen, make proteins like albumin, and produce bile. When this tissue is injured, those functions fall.
Difference between parenchymal vs non-parenchymal liver disease
Parenchymal disease targets hepatocytes. Non-parenchymal disease affects other parts, like the bile ducts, blood vessels, or liver immune cells. For example, obstruction of bile ducts mainly injures the biliary structures rather than the hepatocytes. Tests and imaging help tell them apart because treatment differs.
How liver parenchyma damage affects function
When hepatocytes are inflamed or scarred, the liver cannot process toxins well. You can get jaundice (yellow skin or eyes), clotting problems, low albumin with swelling, and poor drug clearance. Over time, scarring (fibrosis) can become cirrhosis, which greatly lowers liver reserve and raises the risk of liver cancer. Early detection and treating the cause slows or stops progression.
Causes of Liver Parenchymal Disease
Viral hepatitis (Hepatitis B, C, A, D)
Viruses infect hepatocytes and cause acute or chronic inflammation. Hepatitis A usually causes short-term illness. Hepatitis B and C often cause chronic injury that may lead to scarring and cancer if untreated. Vaccination prevents hepatitis A and B; hepatitis C is now frequently curable with antiviral drugs. Testing identifies viral causes so treatment can begin.
Alcohol-related liver injury
Alcohol damages hepatocytes directly and triggers fat accumulation, inflammation, and cell death. Continued heavy drinking drives progression from fatty change to alcoholic hepatitis and cirrhosis. Stopping alcohol lowers the risk of further harm, but advanced scarring may not fully reverse.
Non-alcoholic fatty liver disease (NAFLD & NASH) (fatty liver parenchymal disease)
When fat collects in hepatocytes without heavy alcohol use, you have NAFLD. If fat plus inflammation and cell injury occur, that is NASH. NAFLD and NASH are linked to obesity, insulin resistance, high blood fats, and type 2 diabetes.
They are now a leading cause of chronic liver disease worldwide. Weight loss and metabolic control are the main treatments.
Autoimmune conditions (autoimmune hepatitis)
In autoimmune hepatitis, your immune system attacks hepatocytes. Blood tests for autoantibodies and liver inflammation help diagnose it. Doctors usually treat with immunosuppressing medicines to control inflammation and protect the liver.
Metabolic disorders (Wilson disease, hemochromatosis)
Some inherited conditions cause harmful metal buildup. Wilson’s disease causes copper to collect in the liver and brain. Hemochromatosis causes excess iron storage. Both damage hepatocytes and need specific tests and targeted treatment to remove the excess metal. Early diagnosis prevents severe injury.
Toxic & drug-induced liver injury
Many medicines, supplements, and toxins can injure hepatocytes. Damage ranges from mild enzyme rises to sudden liver failure. Always tell your doctor about all medicines and supplements you take. If severe toxicity is suspected, urgent care is needed.
Genetic disorders affecting liver parenchyma
Other inherited enzyme defects can impair hepatocyte function and cause chronic liver disease. Genetic testing and specialist care are used when these are suspected.
Vascular causes (Budd-Chiari syndrome)
Blocked veins that drain the liver cause congestion and hepatocyte injury. Sudden pain, liver enlargement, and rapid deterioration can follow. Treatments aim to restore blood flow and manage complications.
Chronic inflammation and fibrosis progression
Any long-term injury drives fibrosis. Scars replace healthy hepatocytes and reduce function. Monitoring fibrosis is critical because progression to cirrhosis changes management and surveillance for cancer. Noninvasive tests now help track fibrosis without routine biopsy.
Liver Parenchymal Disease Symptoms
Early symptoms: fatigue, mild pain, loss of appetite
Early symptoms are often mild. You may feel tired, have a dull ache in the right upper belly, or eat less. These signs are not specific but should prompt testing when risk factors exist.
Right upper quadrant abdominal discomfort
A dull or sharp sensation under your right ribs can indicate liver inflammation or enlargement. Pain patterns and exam findings help your clinician decide next steps.
Dark urine, pale stools, jaundice
If bilirubin builds in your blood because the liver cannot process bile, your skin and eyes turn yellow. Urine becomes dark, and stools may pale. These are clear signals to seek prompt medical evaluation.
Bloating, nausea, vomiting
Digestive symptoms often occur with liver inflammation. If these persist, testing is appropriate.
Itching, swelling, easy bruising
Poor bile flow and low protein production can cause itching and fluid in the legs or belly. Low clotting factor production leads to bruising and bleeding. These signs suggest more advanced functional impairment.
Types of Liver Parenchymal Disease
Fatty liver (NAFLD & NASH)
Fatty change ranges from simple steatosis to NASH, which includes inflammation. Fatty liver parenchymal disease can progress if not addressed. Diet and exercise are central to treatment.
Alcoholic liver disease
This ranges from fatty liver to alcoholic hepatitis and cirrhosis, depending on drinking patterns and other risks.
Chronic hepatitis (viral or autoimmune)
Longstanding viral or immune injury can keep hepatocytes inflamed and lead to scarring. Antiviral and immune therapies reduce the risks of progression.
Cirrhosis and advanced fibrosis
Cirrhosis is widespread scarring with loss of normal structure. It often requires specialist care and changes the long-term prognosis.
Diagnosis Of Liver Parenchymal Disease
Doctors use tests that build a clear picture.
Blood tests (LFTs, bilirubin, enzymes)
Liver function tests, bilirubin, albumin, and clotting studies show how the liver performs. Abnormal tests prompt imaging and further evaluation.
Imaging tests (ultrasound, CT, MRI)
Ultrasound is a common first test for fat and size changes. CT and MRI give more detail when needed. Imaging helps detect nodules and advanced scarring.
FibroScan for fibrosis assessment
FibroScan measures liver stiffness and helps estimate fibrosis without a biopsy. It is useful to monitor progression.
Liver biopsy for definitive evaluation
When the diagnosis is unclear, a small tissue sample shows fibrosis and inflammation. Biopsy guides treatment decisions in complex cases. Evidence supports biopsy when noninvasive tests conflict.
Treatment For Liver Parenchymal Disease
Treatment Depends On The Underlying Cause
You cannot treat liver parenchymal disease with one fixed plan. Your doctor first finds the cause using blood tests, scans, and sometimes a biopsy. Then the plan targets the exact trigger. For viral hepatitis, the focus is on antiviral drugs that reduce virus levels and prevent cirrhosis.
For autoimmune causes, doctors use immune medicines that calm the attack on liver cells. For metal overload, therapies remove extra iron or copper. When causes of liver parenchymal disease include alcohol or obesity, lifestyle changes sit at the center of care.
Lifestyle Modifications (Weight Loss, Exercise, Diet)
For fatty liver parenchymal disease , lifestyle is your main tool. Strong data show that losing about 7-10% of body weight can reduce liver fat, improve inflammation, and even improve fibrosis.
You can start with three steps. First, reduce sugary drinks and highly processed foods. Second, choose more vegetables, whole grains, beans, and lean protein. Third, move more on most days of the week. Studies show both aerobic exercise and resistance training lower fat in the liver, even when weight loss is modest.
This lifestyle approach does not replace medical care. It works alongside other treatments for liver parenchymal disease chosen by your doctor.
Medications For Viral Or Autoimmune Hepatitis
For hepatitis B and C, antiviral drugs help protect your liver. The goal is to suppress the virus, prevent liver parenchymal disease symptoms , and reduce the risk of cirrhosis and liver cancer. The exact drug and dose depend on your virus type, viral load, and other health issues.
For autoimmune hepatitis, steroids and other immunosuppressants reduce inflammation in the parenchyma. Doctors usually start with stronger treatment and then lower doses once the disease is under control. Dosage varies by age, weight, and disease activity.
Alcohol Cessation And Support Programs
If alcohol is a key cause of your liver parenchymal disease , stopping drinking is essential. Early stages of alcoholic fatty liver can improve fully with complete abstinence. More advanced stages still gain benefit, as further injury slows. Support programs, therapy, and sometimes medicines help you stay alcohol-free.
Managing Metabolic Liver Conditions
If you have diabetes, high cholesterol, or metabolic syndrome, good control protects your liver. Medicines for blood sugar and lipids, plus weight loss, decrease liver parenchymal disease symptoms from fat buildup. For hemochromatosis, regular blood removal lowers iron. For Wilson’s disease, chelation drugs remove extra copper.
Monitoring Fibrosis Progression
You need regular follow-up once you have liver parenchymal disease . Doctors use blood scores, FibroScan, and imaging to watch scar build-up. If tests show rising stiffness or new nodules, they adjust treatment for liver parenchymal disease and consider cancer screening.
When Liver Transplant Is Required
If the liver can no longer support your body, a transplant may be the only option. This stage appears with repeated fluid buildup, bleeding varices, severe encephalopathy, or liver cancer that fits transplant rules. Transplant does not remove the original cause, so you still need care for viruses, alcohol use, or metabolic disease afterward.
Long-Term Management And Follow-Up
Chronic liver parenchymal disease means a long-term partnership with your care team. You may need six or twelve-month visits for labs and imaging. Vaccines for hepatitis A and B, flu, and pneumonia are often advised. Your plan may change as new drugs appear because research in this field grows quickly.
Fatty Liver Parenchymal Disease
Causes Of Fatty Infiltration In The Liver
In fatty liver parenchymal disease , extra fat builds up inside hepatocytes. Common causes of liver parenchymal disease here are excess calories, soft drinks, fast food, inactivity, and insulin resistance. New guidelines now group these under metabolic dysfunction-associated steatotic liver disease.
Risk Factors: Obesity, Insulin Resistance, Metabolic Syndrome
You have a higher risk if you carry central obesity, have type 2 diabetes, or have high triglycerides. Sleep apnea and polycystic ovary syndrome can add to that risk. Family history also plays a role.
Reversibility And Expected Recovery Timeline
The good news is that fatty liver parenchymal disease is often reversible. If you lose 7 to 10 percent of body weight over months, studies show major improvements in steatosis and inflammation. Weight loss over 10 percent may even improve fibrosis in many patients, although not all.
Diet Patterns That Reverse Fatty Liver
Several patterns help. A Mediterranean-style diet, rich in vegetables, fruits, olive oil, nuts, and fish, has strong support. Limiting added sugar and refined white flour is key. Regular meals with smaller portions support steady progress.
Supplements Shown To Support Fatty Liver Healing
Some studies suggest benefits from vitamin E and certain insulin-sensitizing drugs in select groups. Evidence for many herbal products is limited or mixed. You should not start supplements for liver parenchymal disease without medical advice, because some “natural” products can harm the liver.
Stages From Steatosis To NASH To Fibrosis
The pathway usually starts with simple fat, then moves to NASH when inflammation appears, and then to fibrosis. Not everyone moves through all stages. Early treatment for liver parenchymal disease lowers the chance that simple fat turns into scar tissue.
Complications Of Liver Parenchymal Disease
Fibrosis And Cirrhosis
Long-standing liver parenchymal disease leads to a scar that replaces healthy tissue. Once cirrhosis forms, the risk of liver failure and cancer increases. You then need close specialist follow-up.
Portal Hypertension
Cirrhosis raises pressure in the portal vein. This portal hypertension causes fluid in the belly, swollen veins, and spleen enlargement. It is one of the most serious results of chronic disease.
Liver Failure
In liver failure, the parenchyma can no longer keep toxins low or maintain normal clotting. Your skin may turn yellow, you may feel confused, and your body may swell. This state often needs transplant evaluation.
Hepatocellular Carcinoma (HCC)
Any long-standing liver parenchymal disease with fibrosis, especially cirrhosis, raises the risk of primary liver cancer. Most guidelines advise ultrasound every six months for high-risk patients.
Ascites, Varices, Encephalopathy
Ascites is fluid in the abdomen that makes your belly look swollen. Varices are thin-walled veins in the esophagus or stomach that can bleed suddenly. Encephalopathy is a brain change from toxins, often seen as confusion, sleep change, or personality change. These problems all point to decompensated disease and need urgent specialist care.
Prevention & Lifestyle Management
Alcohol Moderation Or Complete Avoidance
If you already have liver parenchymal disease , even small amounts of alcohol may worsen injury. Many experts advise full avoidance in this case.
Anti-Inflammatory Diet For Liver Health
Choose mostly whole, unprocessed foods. Eat plenty of vegetables, fruits, legumes, and healthy fats. Limit sugar, deep-fried snacks, and sugary drinks. This style protects liver cells and also improves heart and diabetes risk.
Weight Control And Exercise Routines
Aim for steady, realistic weight loss, not crash diets. Brisk walking, cycling, and simple strength exercises most days help control liver parenchymal disease symptoms from fat buildup. Exercise also improves insulin resistance even without a large weight change.
Medication Awareness (Avoid Hepatotoxic Drugs)
Tell your doctor about every pill, including over-the-counter drugs and herbal products. Some medicines are known to damage parenchyma. Your doctor can choose safer options if you already have liver parenchymal disease .
Viral Hepatitis Vaccination And Prevention
If you have chronic liver parenchymal disease , vaccination against hepatitis A and B is often recommended, unless you are already immune. Safe sex, clean needles, and safe medical procedures lower hepatitis risk.
Managing Diabetes & Cholesterol To Protect Liver
Tight control of blood sugar and cholesterol slows fat buildup and inflammation in the liver. It also reduces overall cardiovascular risk, which is high in people with fatty liver parenchymal disease .
When To Seek Medical Care
Persistent Abdominal Pain Or Jaundice
You should see a doctor quickly if you notice constant right upper abdomen pain, new jaundice, or dark urine. These may point to active liver parenchymal disease that needs fast testing.
Signs Of Advanced Liver Decompensation
Go to emergency care if you see vomiting blood, black stools, marked belly swelling, confusion, or severe shortness of breath. These signs suggest serious complications of liver parenchymal disease .
When Blood Tests Show Abnormal Liver Function
If routine blood work shows raised liver enzymes, raised bilirubin, or low albumin, you should not ignore it. Ask for further assessment to rule out significant causes of liver parenchymal disease .
High-Risk Groups Needing Early Evaluation
You should request liver checks early if you have diabetes, obesity, long-term alcohol use, chronic viral hepatitis, or a strong family history. Early diagnosis allows treatment for liver parenchymal disease before a major scar forms.
FAQ
Is Liver Parenchymal Disease Reversible?
Early liver parenchymal disease from fat, alcohol, or mild hepatitis can often improve or even normalize with treatment and lifestyle change. Advanced cirrhosis usually cannot be reversed, but you can still slow further damage.
Can Fatty Liver Cause Parenchymal Damage?
Yes, fatty liver parenchymal disease injures hepatocytes over time when inflammation appears. Persistent fat and inflammation can lead to fibrosis, cirrhosis, portal hypertension, and other serious liver parenchymal disease symptoms .
What Is The Life Expectancy With Parenchymal Liver Disease?
Life expectancy with liver parenchymal disease varies with cause, stage, and control of risks. Someone with early fatty liver may live a normal span, while advanced cirrhosis can shorten lifespan.
Which Foods Worsen Liver Parenchymal Disease?
Sugary drinks, refined white flour, deep-fried fast foods, and heavy alcohol intake all strain the liver. These choices worsen liver parenchymal disease symptoms and speed progression toward fibrosis or cirrhosis.
Can Liver Parenchymal Disease Be Cured?
Some causes of liver parenchymal disease , such as hepatitis C, can be cured with antivirals. Others, like autoimmune hepatitis or genetic disorders, cannot be fully cured but can be controlled long-term.
What Is The Best Diet For Liver Parenchymal Disease?
A Mediterranean-style pattern suits many people with liver parenchymal disease . It emphasizes vegetables, fruits, whole grains, nuts, and fish and reduces processed food, sugar, and alcohol.
Does Liver Parenchymal Disease Always Lead To Cirrhosis?
No, not every case of liver parenchymal disease progresses to cirrhosis. Early detection, removal of triggers, and strong lifestyle changes often stop progression, especially with metabolic or alcohol-related diseases.
How Often Should Patients Get Follow-Up Tests?
Follow-up for liver parenchymal disease depends on the stage and cause. Mild fatty liver might need yearly checks, while advanced fibrosis often needs blood tests and imaging every six months, plus cancer screening.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin