High GGT blood test results indicate increased activity of gamma-glutamyl transferase, an enzyme tied to liver processing and bile transport. When your report shows this elevation, it signals that something affects liver cell function or bile movement. This enzyme responds early to biological stress, often before structural damage becomes obvious.
Table of Contents
ToggleKey Takeaways
- A high GGT blood test shows elevated activity of a liver-linked enzyme
- It signals stress in bile flow or detox pathways
- Alcohol, disease, or drugs may raise levels
- It does not produce symptoms itself
- Doctors confirm meaning through repeat testing and related markers
A high GGT blood test matters because it helps clinicians detect subtle metabolic or toxic strain that other liver markers miss. Elevated activity often reflects the body reacting to chemical exposure, inflammation, or impaired bile flow.
Persistent elevation correlates with higher long-term cardiometabolic risk and liver disease progression. You should view a high GGT blood test as a biochemical signal requiring structured evaluation. Doctors examine medical history, alcohol intake, metabolic health, medication exposure, and companion lab values before drawing conclusions.
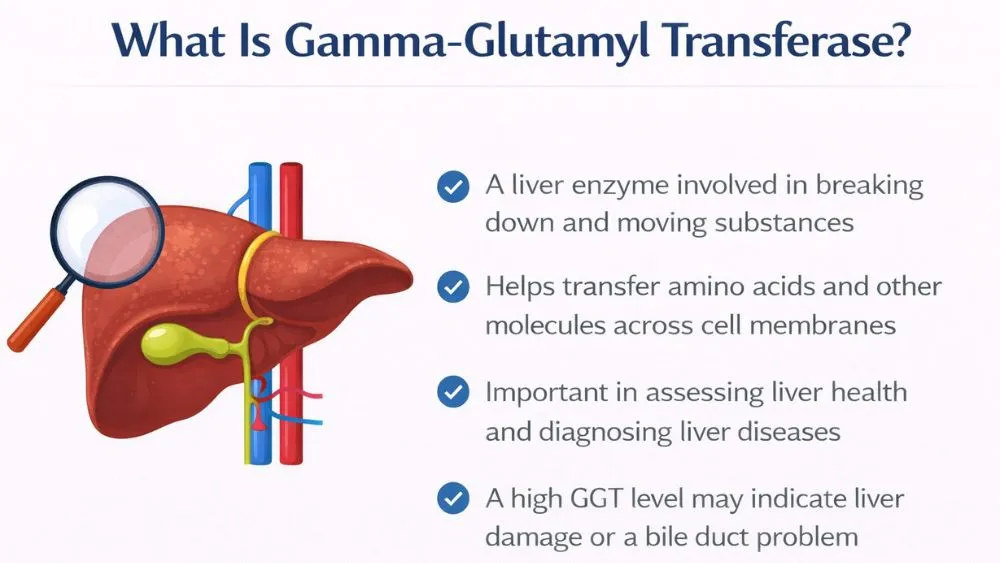
What Is Gamma-Glutamyl Transferase (GGT)?
Gamma-glutamyl transferase (GGT) is an enzyme that supports amino acid transport across membranes and assists in recycling glutathione, the body’s main cellular antioxidant. Glutathione protects tissues against reactive oxygen molecules produced during detoxification.
From a tissue perspective, gamma-glutamyl transferase (GGT) relates closely to anatomical distribution. Highest concentrations occur in:
- Hepatocytes, meaning liver cells responsible for metabolism
- Biliary epithelium, meaning the bile duct lining that carries digestive fluids
- Renal [kidney] tubular tissue and pancreatic cells in smaller quantities
A high GGT blood test often reflects enzyme leakage into circulation after membrane irritation or adaptive overproduction during chemical processing.
GGT is highly sensitive, meaning small disruptions cause measurable changes. It lacks specificity, meaning elevation does not identify the cause. Alcohol exposure, fatty accumulation, medication metabolism, and endocrine dysfunction may all raise levels through different mechanisms.
Biochemical research indicates enzyme induction occurs through gene expression activation in response to xenobiotics, which are foreign compounds processed by the liver. This cellular adaptation protects tissues but complicates interpretation. Because of this complexity, a high GGT blood test always requires correlation with additional markers and history rather than isolated reading.
Causes Of High GGT
Evaluating the causes of high GGT requires grouping triggers by biological pathway. This structure allows a clearer understanding of why elevation occurs.
Liver And Bile Related Causes
Among common causes of high GGT , metabolic fatty liver conditions dominate globally. Excess fat accumulation alters cellular metabolism and increases oxidative burden. Enzyme activity rises as detox pathways intensify.
Cholestasis (reduced or blocked bile flow) also contributes. Pressure buildup irritates ductal cells, allowing enzymes to enter circulation. Structural disease or inflammation can produce this effect.
Long-standing hepatic injury leads to remodeling of liver architecture. In those settings, enzyme release reflects chronic cellular stress rather than acute damage. A high GGT blood test in this category frequently appears alongside abnormal alkaline phosphatase, providing interpretive clues.
Industrial solvents and heavy metals affect liver detox mechanisms. Evidence documenting this effect exists but remains population-specific and requires careful contextual interpretation.
Alcohol-Related Elevation
Alcohol metabolism activates microsomal oxidation pathways inside hepatocytes. This biochemical stimulation ranks among the major causes of high GGT because enzyme production increases in response to sustained exposure.
Regular alcohol intake produces adaptive upregulation. Short, intense exposure causes temporary spikes.
Non-Liver Causes
Not all causes of high GGT originate within liver tissue. Metabolic syndrome alters inflammatory signaling and insulin sensitivity, affecting enzyme regulation. Pancreatic disorders occasionally affect readings due to shared ductal connections.
Cardiovascular associations exist as well. Elevated enzyme levels correlate with endothelial dysfunction markers, meaning impaired blood vessel lining behavior.
This range of mechanisms reinforces why a high GGT blood test cannot be reduced to a single explanation. Systemic context shapes meaning.
Medications That Increase GGT
Anticonvulsant agents stimulate hepatic enzyme synthesis to accelerate chemical breakdown. This adaptive response elevates circulating markers. Several antimicrobial drugs also influence liver enzyme pathways during metabolism.
Lipid-modifying medications occasionally alter hepatocyte signaling, producing modest elevation without structural injury. Analgesics (pain-relief medications) may contribute depending on metabolic load and duration of use. Doctors usually assess exposure rather than assume toxicity when evaluating a high GGT blood test .
The table below summarizes broad pharmacologic categories commonly reviewed:
| Medication Class | Mechanism Affecting Enzyme Activity | Clinical Interpretation |
| Anti-seizure drugs | Enzyme induction for metabolism | Persistent mild elevation possible |
| Select antibiotics | Temporary hepatic processing stress | Often reversible |
| Cholesterol therapy | Cellular signaling adaptation | Monitor trends |
| Pain medications | Increased metabolic workload | Variable impact |
High GGT Symptoms
A high GGT blood test does not produce physical sensations. The enzyme itself does not cause illness or discomfort. When you read about symptoms of high GGT , you must interpret them as signals from the underlying condition affecting liver or bile pathways rather than the laboratory value itself.
If you have symptoms of high GGT , you will experience fatigue linked to metabolic strain. Energy processing in the liver affects glucose regulation and toxin clearance. When those processes slow, you may notice reduced stamina, vague weakness, or daytime sleepiness.
Digestive discomfort represents another cluster associated with symptoms of high GGT . Reduced bile flow affects fat digestion. You might observe abdominal heaviness after meals, nausea, or irregular stool color. These signs reflect bile imbalance rather than enzyme elevation itself.
In advanced hepatobiliary stress, skin or eye yellowing may develop due to bilirubin retention. Dark urine or pale stools may follow. These findings indicate impaired bile excretion pathways. While less frequent, they demand prompt medical review when present with a high GGT blood test .
What Happens During A GGT Test?
A GGT test involves venous blood collection using standard sterile technique. Laboratory analysis quantifies enzyme activity through biochemical assays that measure substrate breakdown rates. Results integrate into larger metabolic panels to improve interpretation depth.
Preparation instructions form an important part of what happens during a GGT test .
- Alcohol intake within twenty-four hours can influence results.
- High-fat meals before testing may affect companion markers.
- Fasting is sometimes requested depending on panel composition.
Repeat measurement remains central during a GGT test workflow. Enzyme levels fluctuate due to short-term metabolic changes. Physicians often reassess after several weeks to identify persistence or normalization.
Laboratory interpretation also examines ratios between GGT and alkaline phosphatase. Combined elevation often points toward biliary involvement rather than isolated hepatocellular stress.
High GGT With Normal Other Liver Tests
A high GGT blood test may appear alongside normal ALT and AST values. This pattern occurs frequently because GGT responds to biochemical stimulation rather than structural injury alone. Alcohol exposure, medication metabolism, and early metabolic changes often trigger elevation before cellular damage develops.
Another mechanism involves antioxidant system activation. GGT supports glutathione recycling, which protects cells from oxidative stress. Increased activity can represent a defensive adjustment rather than an injury. Therefore, a high GGT blood test alone does not confirm disease when other values remain stable.
Doctors review sequential results rather than reacting to a single measurement. Stable isolated elevation may lead to observation and exposure review. Progressive change prompts imaging or additional testing.
When Should You Be Concerned About High GGT?
A high GGT blood test that remains elevated over multiple assessments indicates continuing biological stress requiring investigation.
Combined abnormalities increase clinical relevance. Elevation together with alkaline phosphatase or bilirubin suggests bile transport disruption. These combinations narrow diagnostic possibilities and guide imaging decisions. Physicians interpret clusters of findings rather than focusing on the numeric magnitude of a high GGT blood test alone.
Individuals with long-term alcohol intake, metabolic syndrome, or family history of liver disease receive closer monitoring. In these groups, clinicians shorten follow-up intervals and broaden testing when a high GGT blood test appears.
What To Do After A High GGT Result
Doctors usually repeat testing to verify persistence because temporary biological fluctuations occur. This verification ensures a high GGT blood test represents ongoing physiology rather than transient variation.
Doctors evaluate prescriptions and supplements that belong to medications that increase GGT categories. Adjustments occur only under supervision because abrupt changes may cause harm. This step prevents unnecessary concern over pharmacological effects influencing a high GGT blood test .
Further evaluation may include ultrasound imaging to assess liver texture and bile ducts. Expanded laboratory panels may analyze additional markers. These diagnostic tools clarify the biological source of a high GGT blood test elevation and guide management decisions.
Advanced assessment may involve fibrosis scoring or targeted imaging. These measures aim to identify underlying processes early without unnecessary intervention.
FAQs – High GGT Blood Test
What does a high GGT blood test mean?
It means enzyme activity rose above the expected range, signaling liver detox strain or bile flow disruption. A high GGT blood test alone identifies biochemical stress, not disease. Physicians correlate alcohol exposure, metabolic markers, medications, and repeat values before interpretation.
Is high GGT always due to alcohol?
No. Alcohol explains many cases, but a high GGT blood test also occurs with fatty liver, bile obstruction, anti-seizure drugs, metabolic syndrome, and toxin exposure. Exposure review and companion markers distinguish these mechanisms during clinical evaluation.
Can medications raise GGT levels?
Yes. Several medications that increase GGT alter hepatic enzyme production, especially anticonvulsants, lipid therapy, certain antimicrobials, and analgesics. A high GGT blood test linked to drugs often stabilizes after supervised adjustment rather than indicating injury.
Does high GGT cause symptoms?
No. A high GGT blood test causes no sensations. Reported symptoms of high GGT reflect underlying bile imbalance or liver strain, such as fatigue or digestion changes. Clinical assessment identifies the responsible physiological process.
Can GGT be high with normal ALT and AST?
Yes. A high GGT blood test commonly appears alone because enzyme induction occurs before structural injury. Alcohol exposure, medication metabolism, or oxidative stress activation often produce isolated elevation with otherwise stable panels.
Should high GGT be rechecked?
Yes. Physicians repeat measurement within weeks because what happens during a GGT test includes trend monitoring. Persistent elevation confirms biological relevance, while normalization suggests transient exposure influence or reversible metabolic fluctuation.
Is high GGT dangerous?
It depends. A high GGT blood test becomes concerning when persistent, rising, or paired with bilirubin or alkaline phosphatase abnormalities. Isolated stable elevation rarely signals acute danger but still requires evaluation for underlying contributors.
Does GGT reflect liver function or injury?
Mostly injury signaling. A high GGT blood test reflects oxidative stress or bile transport disturbance rather than functional capacity like protein synthesis. Interpretation alongside albumin and clotting markers clarifies true functional status.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.