Treatment for inflammatory bowel disease focuses on controlling long-term gut inflammation that damages the digestive tract and disrupts daily life. You do not treat IBD once and move on. You manage it over time using medicines, close monitoring, and lifestyle support. The disease mainly includes Crohn’s disease and ulcerative colitis.
Table of Contents
ToggleBoth cause immune-driven inflammation inside the gut. Without proper care, this inflammation leads to pain, bleeding, nutrient loss, and serious bowel damage. Early and structured care lowers flare risk and protects your gut.
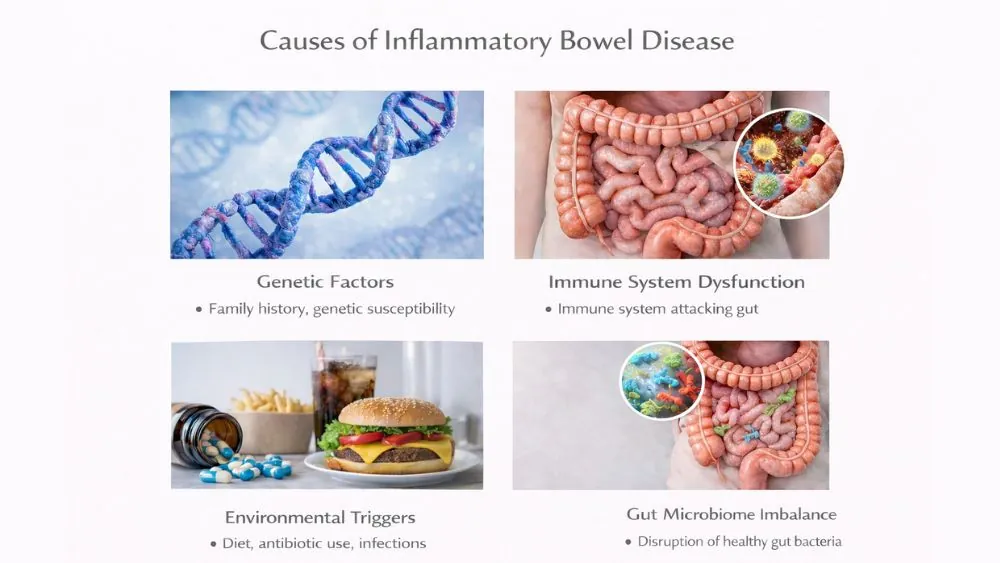
Causes of Inflammatory Bowel Disease
Inflammatory bowel disease develops when your immune system reacts abnormally inside the gut and fails to switch off. Genetics, gut bacteria imbalance, and outside triggers combine to damage the intestinal lining over time. These causes explain why symptoms differ from person to person and why treatment responses vary.
Genetic Factors
Genes affect how your immune system behaves. If a close family member has IBD, your risk increases. Certain genes affect how your gut barrier works. A weak barrier allows bacteria to trigger immune attacks. Genes do not guarantee disease. They raise vulnerability.
Immune System Dysfunction
Your immune system should attack harmful germs only. In IBD, it attacks healthy gut tissue. This response does not shut off. White blood cells stay active inside the bowel wall. This causes swelling, ulcers, and bleeding. This immune error explains why treatment for inflammatory bowel disease often targets immune signals rather than symptoms alone.
Environmental Triggers
Modern environments influence IBD risk. Early antibiotic exposure can alter gut bacteria. Diets high in processed foods may stress the gut lining. Repeated gut infections can activate immune responses. These triggers do not cause IBD by themselves. They push the disease to start in people already at risk.
Gut Microbiome Imbalance
Your gut contains helpful bacteria that protect the bowel lining. In IBD, these helpful bacteria decrease. Harmful strains increase. This imbalance weakens immune control. It also explains why symptoms worsen after infections or stress. Many treatments for inflammatory bowel disease now aim to restore balance rather than just suppress symptoms.
Symptoms of Inflammatory Bowel Disease
Symptoms appear when inflammation damages the gut wall and affects digestion, absorption, and nerve signaling. Some symptoms stay limited to the bowel, while others affect joints, skin, eyes, and energy levels. The pattern often shifts between flare periods and remission phases.
Digestive Symptoms
Abdominal pain is common. Diarrhea may last weeks or months. Blood in stool suggests active inflammation. Some people feel constant urgency. Appetite often drops. Weight loss may follow due to poor nutrient absorption.
Systemic and Extraintestinal Symptoms
IBD affects more than the gut. Fatigue is common even during mild disease. Joint pain may occur due to immune activity. Skin rashes and eye irritation can appear. Children may grow slowly when inflammation stays active. These symptoms signal that treatment for inflammatory bowel disease must control whole-body inflammation, not just bowel symptoms.
Symptoms During Flares vs Remission
Flares involve pain, diarrhea, and bleeding. Remission means symptoms reduce or disappear. Inflammation can still exist during remission. That is why ongoing care matters. Silent inflammation causes long-term damage even without pain.
Goals of IBD Treatment
The main goals of treatment for inflammatory bowel disease include stopping active inflammation, keeping the disease quiet long term, and preventing permanent bowel damage. Effective treatment also aims to protect growth, nutrition, mental health, and daily functioning across all life stages.
Reducing Inflammation
Inflammation drives all damage in IBD. Reducing it lowers pain and bleeding. It also prevents scarring of the bowel wall.
Achieving and Maintaining Remission
Remission means controlled disease activity. Symptoms fade, and the bowel lining heals. Long remission lowers cancer and surgery risk.
Preventing Complications
Uncontrolled disease leads to strictures, which are narrowed bowel segments. It can also cause fistulas, which are abnormal tunnels between organs. Early treatment for inflammatory bowel disease lowers these risks.
Improving Quality of Life
IBD affects sleep, school, work, and social life. Effective care restores energy and daily function. Mental health improves when symptoms stay controlled.
Medical Treatment for Inflammatory Bowel Disease
Medicines form the backbone of care. Doctors select drugs based on disease type and severity. Medical treatment for inflammatory bowel disease aims to calm immune activity, not just mask symptoms.
Aminosalicylates (5-ASA Drugs)
These drugs reduce inflammation in the gut lining. Doctors often use them in mild ulcerative colitis. They work best when the disease stays limited to the colon. They also help maintain remission once symptoms improve. This approach remains central in treatment for ulcerative colitis .
Corticosteroids
Steroids act quickly during flares. They suppress immune activity and reduce swelling. Doctors avoid long-term use due to side effects like bone loss and infection risk. Steroids serve as short-term control, not maintenance.
Immunomodulators
These drugs adjust immune responses over time. They reduce flare frequency and steroid dependence. Effects take weeks to appear. Doctors monitor blood counts and liver function regularly. This class supports long-term treatment plans for inflammatory bowel disease.
Biologic Therapies
Biologics target specific immune proteins that drive inflammation. They work well in moderate to severe disease. Many patients achieve deep remission with these drugs. They changed how doctors approach treatment for inflammatory bowel disease by focusing on precise immune control.
JAK Inhibitors
These oral medicines block immune signaling pathways inside cells. They act faster than older immune drugs. Doctors use them in select cases when other treatments fail.
Antibiotics
Antibiotics treat infections and complications like abscesses. They do not control IBD alone. They support other therapies during specific situations, especially in Crohn’s disease. This approach complements treatment for Crohn’s disease when infection complicates inflammation.
Diet Treatment for Inflammatory Bowel Disease
Diet affects symptom severity, bowel workload, and nutrient status during active disease and remission. While food does not cure inflammation, proper diet treatment for inflammatory bowel disease helps reduce irritation, maintain weight, and support healing alongside medication.
Role of Diet in IBD Management
Diet helps control bowel workload and irritation. During inflammation, the gut struggles to absorb nutrients. Poor intake worsens fatigue and weakness. A planned diet supports healing and improves response to medical treatment in inflammatory bowel disease strategies. No single diet works for everyone. You must adjust based on symptoms and disease phase.
Foods to Avoid During Flares
During flares, rough foods irritate the gut lining. Raw vegetables, seeds, nuts, and popcorn often worsen pain. Fatty and fried foods increase diarrhea by speeding bowel movement. Sugar alcohols and fizzy drinks can cause bloating. Avoiding these reduces stool volume and cramping while inflammation stays active.
Foods That May Help Reduce Symptoms
Soft, low-fiber foods digest easily. Cooked rice, bananas, eggs, and lean meats support energy needs. Soluble fiber, found in oats and applesauce, absorbs water and firms stool. These choices help you maintain weight while supporting diet treatment for inflammatory bowel disease plans.
Elimination and Low-Residue Diets
Elimination diets remove trigger foods to identify intolerance. Low-residue diets reduce stool bulk and bowel strain. Doctors often suggest these short-term measures during flares. Long-term use without guidance risks nutrient loss. These diets work best when paired with medical treatment for inflammatory bowel disease .
Enteral Nutrition
Enteral nutrition uses liquid formulas instead of solid food. This approach relaxes the bowel and reduces inflammation. It works especially well in children with Crohn’s disease. It supports growth while controlling disease activity. This method complements treatment for Crohn’s disease when symptoms stay severe.
Lifestyle Changes for Managing IBD
Lifestyle choices influence immune balance, flare frequency, and recovery speed. Stress control, sleep quality, physical activity, and smoking status all affect how well treatment for inflammatory bowel disease works over time.
Stress Management
Stress does not cause IBD. It triggers immune responses that worsen symptoms. Chronic stress increases gut sensitivity and pain perception. Breathing exercises, counseling, and structured routines reduce flare frequency. Mental calm supports physical healing.
Smoking Cessation
Smoking worsens Crohn’s disease by increasing gut inflammation and narrowing blood vessels. It raises surgery risk and medication failure. Quitting improves response to treatment for inflammatory bowel disease and lowers relapse rates.
Physical Activity
Light exercise improves circulation and bone strength. Walking and stretching reduce fatigue and joint stiffness. Overexertion during flares can worsen symptoms. Balance matters. Regular movement supports immune balance and mood stability.
Sleep and Mental Health Support
Poor sleep increases inflammation markers. Anxiety and depression affect many IBD patients. Untreated mental strain worsens symptom control. Sleep hygiene and mental health care improve treatment outcomes and quality of life.
Managing IBD During Remission
Even when symptoms disappear, inflammation may continue at low levels. Ongoing monitoring and maintenance therapy protect the bowel from relapse and long-term complications. Remission management reduces hospital visits and improves long-term outcomes.
Maintenance Medications
Doctors prescribe maintenance drugs to keep inflammation low. Stopping medication increases flare risk even if you feel well. Maintenance therapy protects the bowel lining and lowers cancer risk. This approach applies to both treatment for ulcerative colitis and Crohn’s disease.
Monitoring and Follow-Up Care
Blood tests track inflammation and nutrient levels. Stool tests detect hidden gut activity. Colonoscopy checks for healing and cancer risk. Regular monitoring allows early action before symptoms return. Follow-up protects long-term gut health.
Preventing Disease Relapse
Medication adherence matters. Skipped doses raise relapse risk. Stress control, sleep, and diet consistency support remission. Preventing relapse reduces hospital visits and surgery risk.
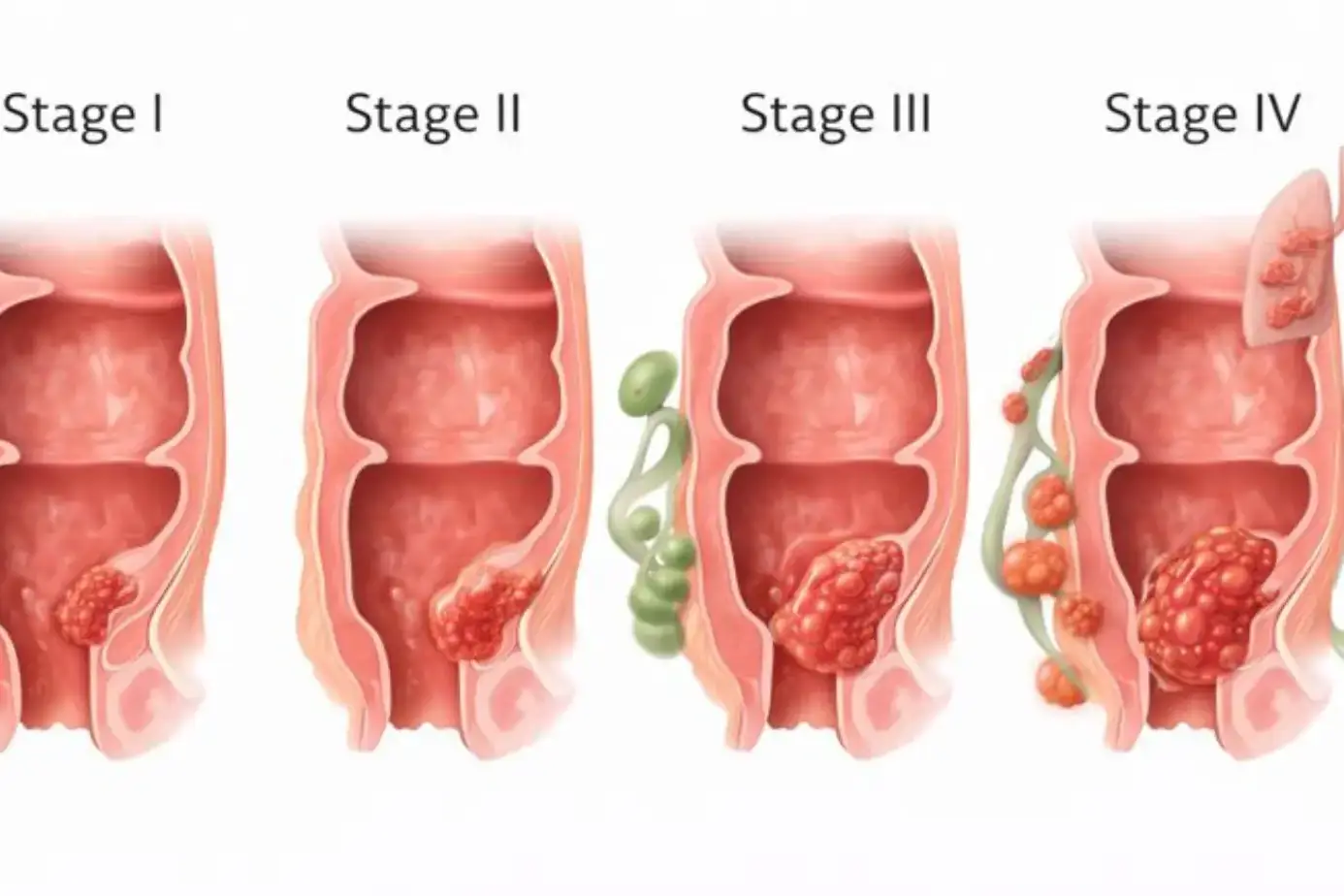
Complications of Untreated or Poorly Controlled IBD
Uncontrolled inflammation leads to structural bowel damage, nutrient deficiencies, and higher cancer risk. These complications develop slowly and often without warning signs.
Intestinal Complications
Chronic inflammation causes strictures, which block bowel flow. Fistulas form abnormal connections between organs. Abscesses can develop from trapped infection. These often require surgery when medical treatment for inflammatory bowel disease fails.
Nutritional Deficiencies
Inflamed intestines absorb nutrients poorly. Iron, vitamin B12, and vitamin D often drop. Deficiencies cause fatigue, nerve issues, and bone weakness. Nutrition monitoring remains essential.
Increased Cancer Risk
Long-standing colon inflammation increases colorectal cancer risk. Risk rises after years of active disease. Regular screening lowers death rates by catching changes early.
When to See a Doctor
Changes in symptoms, medication tolerance, or overall health require medical review. Early evaluation prevents flares from escalating into emergencies. Timely care improves safety and treatment success.
Worsening or Persistent Symptoms
Diarrhea lasting weeks signals active inflammation. Night pain or weight loss needs evaluation. Early treatment prevents escalation.
Signs of Severe Flare
High fever, severe abdominal pain, or heavy bleeding needs urgent care. These signs may indicate infection or bowel damage.
Medication Side Effects
Immunotherapies can raise infection risk. Report unusual bruising, fevers, or breathing issues promptly. Monitoring keeps treatment for inflammatory bowel disease safe.
FAQs
What Is the Most Effective Treatment for Inflammatory Bowel Disease?
The most effective treatment for inflammatory bowel disease depends on disease severity and location. Biologics work well for moderate disease, while mild cases respond to simpler drugs. Personalized care delivers the best results.
Can Inflammatory Bowel Disease Be Cured?
IBD has no permanent cure. Many people achieve long remission with proper treatment for inflammatory bowel disease and monitoring. Long symptom-free periods are common with consistent care.
What Is the Best Treatment for Ulcerative Colitis?
The best treatment for ulcerative colitis depends on how much of the colon is inflamed. Mild cases use anti-inflammatory drugs, while severe disease often needs biologic therapy for control.
How Is Crohn’s Disease Treated Differently From Ulcerative Colitis?
Crohn’s affects deeper bowel layers and multiple gut areas. Treatment for Crohn’s disease often includes immune-targeting drugs and nutrition support rather than surgery alone.
Does Diet Alone Treat Inflammatory Bowel Disease?
Diet alone does not control inflammation. Diet treatment for inflammatory bowel disease supports symptoms and nutrition but must work alongside medical therapy.
Are Biologics Safe for Long-Term IBD Treatment?
Biologics remain safe for many patients with proper monitoring. Doctors screen for infections and adjust care as needed during long-term treatment for inflammatory bowel disease .
When Is Surgery Necessary for IBD?
Surgery becomes necessary when complications develop or medicines fail. It treats strictures, fistulas, or cancer risk. Surgery supports care but does not replace ongoing treatment.
Can Stress Worsen Inflammatory Bowel Disease Symptoms?
Stress worsens symptoms by activating immune pathways. Managing stress improves response to treatment for inflammatory bowel disease and lowers flare frequency.
How Long Does It Take for IBD Treatment to Work?
Steroids may help within days. Biologics take weeks. Response time varies by drug and disease severity. Patience and monitoring guide adjustments.
Can Inflammatory Bowel Disease Go Into Remission Without Medication?
Spontaneous remission is rare. Most people need ongoing treatment for inflammatory bowel disease to maintain gut healing and prevent relapse.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.