A parastomal hernia is a bulge next to a stoma where part of the bowel or fatty tissue pushes through a weak spot in your belly wall. It happens because the stoma passes through muscle. That opening never regains full strength. Pressure inside your belly then pushes on that weak area. Over time the opening can widen. The bulge grows when you stand, cough, or strain. It can flatten when you lie down.
Table of Contents
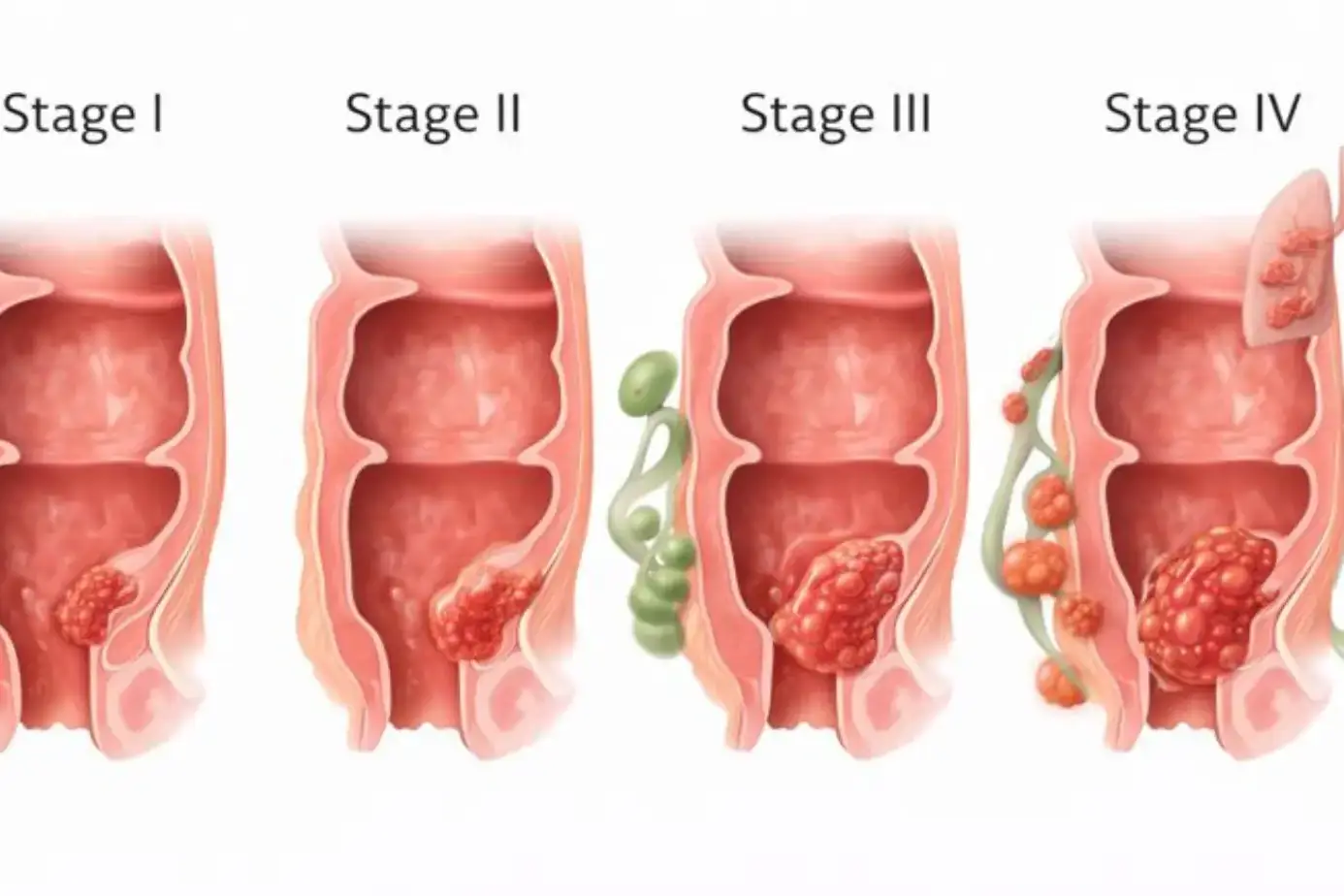
ToggleDoctors confirm the diagnosis with an exam and often with a CT scan, since imaging shows what sits in the hernia sac and whether there are signs of blockage. Rates rise with time, and long-term studies report that up to half of people with a permanent end colostomy will form this type of hernia, which is why prevention and smart care matter from day one.
What Is a Parastomal Hernia?
You live with a stoma that lets stool or urine leave your body through an opening in your belly wall. That opening passes through muscle and a tough layer called fascia. A parastomal hernia forms when tissue slips out beside that opening and bulges under the skin. The bulge often feels soft. It may grow larger later in the day when you have been on your feet. It often grows during a cough, a sneeze, or a strain on the toilet.
Imaging like CT helps separate this problem from a prolapse, which is when bowel slides out through the stoma itself rather than beside it. CT can also map the size of the defect and the contents of the hernia, which helps with planning.
How It Develops After Colostomy, Ileostomy, Or Urostomy Surgery.
All stomas need a hole through the muscle. That hole creates a weak spot. Daily pressure inside your belly pushes on it. If the opening gets wider, bowel or fat can slip through and form a sac. This can happen after colostomy, ileostomy, or urostomy. End colostomy carries the highest risk in many series. Factors such as cough, constipation, and weight gain increase the force that widens the opening.
Why It’s One Of The Most Common Long-Term Stoma Complications?
Time matters. The longer the stoma stays, the more cycles of pressure it faces. That is why rates climb on long follow-up. Major societies report long-term incidence commonly reaching 30 to 50 percent, with higher numbers for some permanent stomas. This frequency explains why teams now consider preventive steps at the first operation for high-risk cases.
Causes Of Parastomal Hernia
Weak Abdominal Muscles Around The Stoma Site.
Your rectus muscles and fascia act like a strong belt. If they are thin, scarred, or cut in a way that leaves less support, the opening stretches more easily. Older age, poor healing, and certain tissue types weaken this belt. CT studies show that larger abdominal wall defects and certain body shapes raise risk.
Increased Intra-Abdominal Pressure From Coughing Or Straining.
High pressure inside your belly pushes outward. Chronic cough, hard stools, trouble passing urine, or frequent lifting all increase that pressure. Repeated spikes stretch fibers at the stoma opening.
Over months or years, the gap grows and a parastomal hernia forms. Managing cough and keeping stools soft lowers these spikes.
Poor Surgical Placement Or Stoma Construction.
Good siting through the rectus muscle, at a flat spot, lowers strain on the appliance and the wall. If emergency conditions prevent careful siting, or if the opening is too large, risk rises.
Expert guidelines advise careful placement and, in selected high-risk end colostomy cases, consider a preventive mesh at the first operation to reduce later herniation.
Obesity, Age, And Postoperative Wound Infections.
Higher body mass index creates more pressure on the wall and more strain on closures. Age brings weaker connective tissue. Infections around the stoma weaken healing and make the wall less resistant. These elements add up and raise risk over time.
Lifting Heavy Objects Or Overexertion After Surgery.
Soon after surgery, your tissues are still healing. Heavy loads or sudden strain stretch the new opening. Later in recovery, bad lifting form and breath-holding still matter. Using a support belt during hard tasks helps distribute the load and protect the area.\
Symptoms Of Parastomal Hernia
Noticeable Bulge Or Swelling Around The Stoma Opening.
A lump forms beside the stoma. It can be small early on. It often grows when you cough or stand. It may shrink when you lie flat. This is the most common sign. Clinical exam plus imaging confirms what is inside the sac and how large the opening has become. This is where parastomal hernia symptoms usually start.
Discomfort, Pressure, Or Pain During Movement Or Coughing.
The bulge pulls on skin and fascia. That pull can ache during walking, bending, or coughing. Long days on your feet can make the ache worse. Good support and pacing ease this load.
Stoma Appliance Not Fitting Properly.
A changing belly shape breaks the pouch seal. You may notice creases under the wafer, more leaks, or a pouch that sits tilted. Appliance changes like convex wafers and barrier rings often help.
Leakage Or Changes In Stoma Output.
A kink in the bowel inside the hernia slows the flow, which causes thicker output and more gas. Leaks irritate skin and raise infection risk. Careful hydration and pouching support protect your skin while you sort the hernia.
Nausea, Bloating, Or Constipation.
These signs come from partial blockage. Gas builds up and makes the area tight. If output slows for many hours and pain grows, you need urgent assessment.
In Severe Cases
A firm, very tender bulge, fever, vomiting, no gas, or a dark stoma color are danger signs. Seek emergency care. Doctors use CT to check for trapped bowel, poor blood flow, or perforation, and then treat fast to avoid tissue loss.
How Common Is A Parastomal Hernia?
Occurs In Up To 50% Of People After Ostomy Surgery
Long-term series and society statements place the incidence between about 20 and 50 percent, depending on stoma type, body build, and how hernias are defined or imaged. The upper figures appear most often with permanent end colostomies.
More Common In Permanent Stomas And Elderly Patients
A permanent stoma sits for years, which means many cycles of strain. Older patients have weaker fascia and less muscle mass. These factors produce more parastomal hernia events with time.
Risk Factors
Extra weight, wound infection, chronic cough, and tissue quality push risk higher. Some imaging work shows that larger defects at creation correlate with later hernia. Paying attention to these factors early helps you plan prevention.
Diagnosing A Parastomal Hernia
Clinical Examination
The clinician inspects and gently presses the area while you stand, cough, and lie down. The exam spotlights the lump, skin issues, and how well the pouch sits. An experienced exam is the first step and often points to the correct diagnosis.
Imaging Tests
CT is widely used because it maps the hernia sac, its contents, and any complications. It is more sensitive than an exam alone and often more helpful than an ultrasound for surgical planning. Ultrasound can assist in some settings, especially when radiation is a concern.
Differentiating From Other Stoma Complications (Like Prolapse).
A prolapse is bowel sliding out through the stoma. A parastomal hernia is tissue that bulges next to the stoma under the skin. CT shows the difference and helps guide the plan. Accurate labeling matters because repair choices differ.
Parastomal Hernia Treatment Options
Nonoperative care aims to reduce symptoms, protect skin, and reduce pressure spikes. These steps can help many people live well even when a parastomal hernia is present.
Non-Surgical Management — Hernia Belts, Binders, And Stoma Support Garments
A well-fitted support garment smooths the contour and spreads the load across your belly. It can reduce aches during walking and chores, and it stabilizes the pouch seal. A stoma nurse can size the opening in the belt and choose the right stiffness for you.
Adjusting Stoma Appliances For Comfort And Seal
Convex wafers, barrier rings, paste, and custom cutting help you manage the uneven surface around a parastomal hernia. These changes often reduce leaks, protect skin, and delay the need for surgery. They are a core part of parastomal hernia treatment options.
Weight Management And Avoiding Strain
Even small weight loss lowers belly pressure and improves outcomes after surgery. Treat cough quickly. Keep stools soft with fluids and fiber, as advised. Do not hold your breath during effort. Exhale through the hard part of a lift.
Lifestyle Modifications
Simple pain relievers may help on busy days. Plan breaks between tasks that need bending or lifting. Walk often to help bowel motion. Use a belt during lawn care, shopping, or heavy housework. These habits support comfort while you weigh the next steps.
Parastomal Hernia Repair Surgery
Surgery is considered when symptoms persist despite support, when leaks prevent reliable pouching, or when there are complications like recurrent blockage. Choosing the method depends on the defect size, stoma type, prior surgery, and your overall health.
Indicated When Hernia Causes Pain, Obstruction, Or Appliance Issues.
Persistent pain, frequent leaks, or emergency symptoms point toward repair. Full blockage or suspected strangulation requires urgent treatment. Elective repair focuses on improving daily function and reducing the risk of sudden problems.
Surgical Techniques
Options include mesh reinforcement around the current stoma, repair with relocation to a new site, or occasionally reversal of the stoma when safe.
Mesh repairs spread force over a wider area than stitches alone, which lowers the risk of another hernia in most adult patients. Your surgeon weighs anatomy, infection risk, and prior operations before selecting the plan.
Keyhole (Sugarbaker) Repair: Mesh Placed Internally To Reinforce Abdominal Wall
There are two common mesh layouts. In a keyhole repair, the mesh has a slit and a central hole for the bowel. In a Sugarbaker repair, the mesh lies flat over the defect and routes the bowel laterally under the mesh.
Multiple studies and meta-analyses show that Sugarbaker repairs have fewer recurrences than keyhole repairs, with similar complication rates. These results apply across open and laparoscopic approaches in many series.
Stoma Relocation: Creating A New Stoma Site To Reduce Tension
Moving the stoma to a new, stronger area helps when the current site is scarred or infected, or when prior attempts have failed. Relocation creates a fresh opening through healthier tissue and allows closure of the old hole. It can solve local problems, but still carries the risk of a new parastomal hernia at the new site.
Long-term registry data show that resiting is not always superior to mesh-based local repair, so decisions are individualized.
Laparoscopic Repair: Minimally Invasive Option With Quicker Recovery
Many centers use laparoscopic or robotic methods for parastomal hernia repair. Small incisions often reduce wound issues and can shorten hospital stay. Reports from high-volume programs note faster recovery and excellent visualization of the defect. Technique selection depends on your anatomy and the team’s expertise.
Mesh Vs. Suture Repair: Why Mesh Offers Lower Recurrence Risk
Suture-only repair places heavy stress on a small line of tissue, which tends to fail over time. Mesh spreads force over a larger area, so the repair holds better. Guidelines recommend mesh for most adult elective repairs when contamination is not a major concern. The choice of mesh type and position depends on patient factors and surgeon experience.
Recovery After Parastomal Hernia Repair
Typical Hospital Stay
Hospital stay varies by method and by your health. Minimally invasive repairs often require shorter stays than large open operations. Teams discharge you when pain is controlled, bowels are moving, and you can manage the pouch.
Recovery Timeline
Early walking improves lung function and bowel motion. Most people resume desk tasks and short walks in two to four weeks. Heavier work waits longer. Your team gives a clear timeline for lifting limits and activity goals.
Tips To Avoid Recurrence
Drink enough water to keep urine light and stool soft. Eat fiber as advised. Treat cough quickly. Use a support belt for chores that push your core. Keep weight in a healthy range. These steps lower belly pressure and protect your repair.
When To Contact Your Surgeon After Repair?
Call if fever develops, if redness spreads around the incisions, or if drainage looks cloudy or smells foul. Call if the bulge returns, output stops, pain surges, or the stoma color darkens. Fast action prevents bigger problems.
Potential Complications After Repair
Recurrence Or Mesh Infection
Hernias can return even after good surgery. Meta-analyses show lower recurrence with Sugarbaker mesh than with keyhole layouts. Mesh infection is uncommon but serious. It may need antibiotics and sometimes another operation to remove infected material.
Stoma Retraction Or Poor Appliance Fitting
Swelling after surgery can change stoma height. A stoma nurse can resize your wafer and advise on convexity, paste, or rings. Good appliance fit protects skin and reduces leaks as swelling settles.
Pain Or Fluid Buildup At the Surgical Site
A small fluid pocket under the skin is common and often resolves. Your team may drain a large pocket if it causes pressure or delays healing.
Bowel Obstruction — Rare But Serious
Scar tissue or kinking can block flow. Severe cramps, vomiting, and no gas or stool are warning signs. This requires urgent medical care to protect your bowel.
Preventing Parastomal Hernia
Strengthen Core Muscles With Gentle Exercises.
Breathing drills, pelvic tilts, and simple core activation build support without strain. A therapist or stoma nurse can show you safe moves. Good form matters more than speed or load.
Use A Hernia Support Belt Post-Surgery.
A properly cut belt supports the area during coughs and tasks. Many teams encourage belts early, especially for people at higher risk. Wear it for shopping, yard work, and long walks as advised.
Avoid Heavy Lifting Or Sudden Pressure On the Abdomen.
Keep early loads light. Exhale during effort. Do not hold your breath. Break large jobs into smaller sessions. Protecting the repair now pays off later.
Maintain a Healthy Body Weight And Manage Chronic Cough.
Even a small weight drop reduces wall stress and improves healing. Control cough and treat constipation to avoid pressure spikes. These changes reduce the drive that forms a parastomal hernia.
Ensure Proper Stoma Placement And Technique During Initial Surgery.
Good preoperative marking, sitting through the rectus, and careful creation lower risk. For selected high-risk permanent end colostomies, guidelines support a prophylactic mesh at creation to reduce later hernia formation. Your surgeon balances benefits and risks for your case.
When To See A Doctor
Sudden Pain, Redness, Or Warmth Around Stoma.
These may signal a trapped loop or an infection. Seek care urgently so imaging and treatment can begin at once.
Vomiting, Bloating, Or Absence Of Stool/Gas.
These signs point to a blockage. Do not wait. Prompt evaluation protects bowel and prevents dehydration or perforation.
Changes In Stoma Color Or Output.
A dark, dusky, or purple stoma may reflect poor blood flow. Call at once. Fast action matters.
Appliance Leakage Or Poor Fit Despite Adjustments.
Leaks damage skin and raise infection risk. Ask a stoma nurse to review fit, convexity, and belt options. Fixing the seal often improves comfort and confidence.
FAQs
What Causes A Parastomal Hernia After Stoma Surgery?
A parastomal hernia comes from a weak spot next to the stoma where pressure pushes tissue outward. Obesity, chronic cough, constipation, wound infection, and poor tissue quality increase risk. Careful siting and good healing reduce it.
Is Parastomal Hernia Dangerous?
Many people have only a bulge and mild ache. Trouble starts when leaks, skin irritation, or blockage develop. Severe pain, vomiting, and no gas suggest an emergency. Seek urgent care if danger signs appear.
Can A Parastomal Hernia Heal Without Surgery?
The hole in the muscle does not close on its own. Belts, appliance changes, weight control, and cough control ease symptoms. Surgery treats the defect when symptoms persist or risk rises despite conservative care.
What Does A Parastomal Hernia Bulge Look Like?
You usually see a round swelling next to the stoma that grows when you cough or strain. The mound can make your pouch sit unevenly. It often flattens when you lie on your back for a few minutes.
How Do I Know If My Stoma Bulge Is A Hernia?
A clinician can tell by exam and confirm with CT when needed. CT shows the sac, its contents, and any complications. A clear diagnosis separates parastomal hernia from prolapse or other stoma issues.
What Are The Treatment Options For A Parastomal Hernia?
Nonoperative steps include belts, convex wafers, barrier rings, weight control, and symptom control. Operative options include mesh reinforcement, relocation, or reversal when suitable. Plans are tailored to your anatomy and goals.
Which Is Better — Keyhole Or Sugarbaker Repair?
Research shows Sugarbaker repairs have lower recurrence than keyhole repairs with similar overall complications. Your anatomy and surgeon’s experience still guide the final choice, so discuss specifics.
How Successful Is Parastomal Hernia Repair Surgery?
Success means less pain, better pouch fit, and no return of the bulge. Studies report variable recurrence, but Sugarbaker often performs better. Long-term data show some patients need another repair within years.
Can The Hernia Come Back After Repair?
Yes. Recurrence remains the main challenge after parastomal hernia repair. Technique, tissue quality, and weight control all influence risk. Sugarbaker mesh generally lowers recurrence compared with keyhole.
What Are The Symptoms Of A Strangulated Parastomal Hernia?
Severe pain, a firm, tender lump, fever, vomiting, a dark stoma, and no gas are danger signs. Go to emergency care. Doctors will use CT to assess and operate if needed to save the bowel.
How Long Is Recovery After Parastomal Hernia Surgery?
Walking starts early. Many people return to light tasks in two to four weeks, depending on approach and fitness. Laparoscopic or robotic methods can shorten stay and speed early recovery.
Can I Wear A Hernia Belt Daily?
Yes. A belt cut to your stoma supports the area during chores, work, walks, and cough episodes. Proper sizing by a stoma nurse improves comfort and reduces leaks for many users.
How Can I Prevent A Parastomal Hernia From Recurring?
Keep weight in a healthy range. Treat cough fast. Keep stools soft. Wear a belt for heavy tasks. Follow lifting rules from your team. These habits reduce pressure and protect your repair.
Does Weight Loss Help Reduce Hernia Risk?
Yes. Lower BMI reduces belly pressure and improves wound healing. Even modest weight loss helps. Pair it with good hydration, fiber, and exercise that builds safe core support.
When Should I Seek Emergency Care For A Stoma Bulge?
Seek care now if you have severe pain, vomiting, fever, a dark stool, or no gas or stool. These point to blockage or strangulation. Fast treatment protects your bowel and your life.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.