What are antibiotics?
Antibiotics are medicines that kill germs that cause infections. They fight bacteria. They help when you have an ear or throat infection. They don’t work on viruses like a cold. They are strong. But they may also affect good germs in your body. That is why antibiotics matter.
Table of Contents
ToggleWhat are antibiotics used for?
Doctors use antibiotics to treat bacterial infections. They use them for a bad cough, urinary infection, or skin infection. Antibiotics help you get well faster. But we must use them only when needed. That way, we protect good germs too. what are antibiotics used for
Introduction to microbiota composition from infancy to adulthood
Your body has many tiny creatures called microbes. They live in your gut. From your first days as a baby, you get microbes from your mom and environment. The types of bacteria in your stomach increase as you grow. That mix helps digest food and keep you healthy. When you’re an adult, you have a balanced mix. This mix is called your microbiome.
Antibiotic types commonly administered
Some antibiotics target many germs. Some target only a few. There are pills, liquids, and injections. Examples are penicillin, amoxicillin, and cephalosporins. All fight bacteria. But they can antibiotics disrupt the gut microbiome, even when they help sickness.
Impact of Antibiotics on Gut Microbial Composition
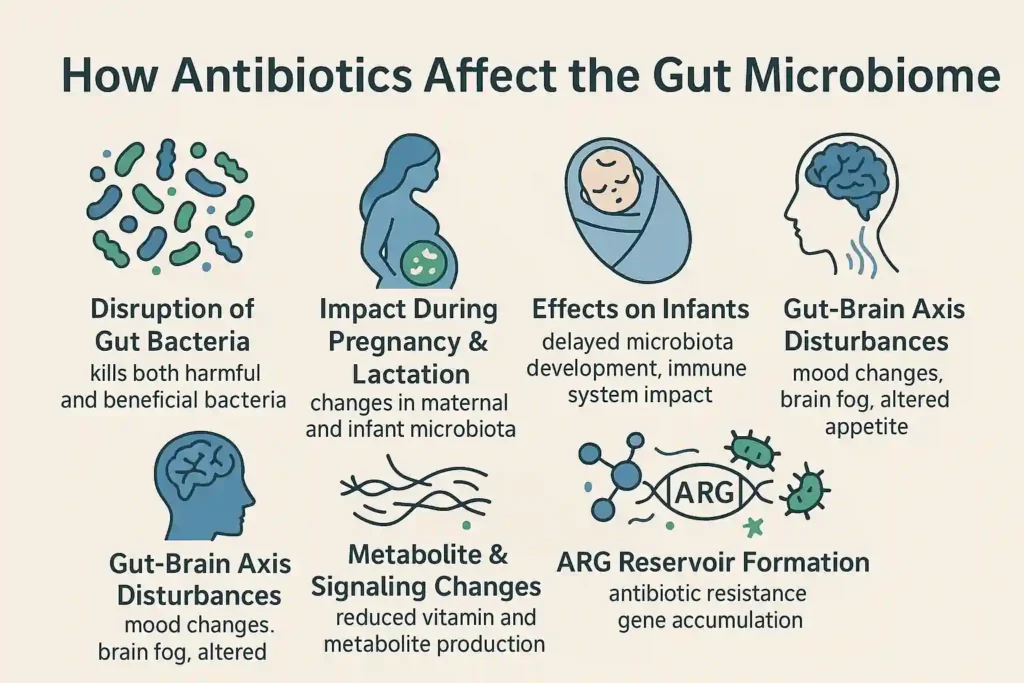
When antibiotics disrupt the gut microbiome, the changes can start within hours of taking the first dose. These medicines target harmful bacteria, but they also harm the beneficial bacteria that protect your health. The effects depend on the timing, type, and dose of antibiotics.
Impact of antibiotics during pregnancy and lactation
Antibiotics taken during pregnancy can cross the placenta, changing the baby’s gut bacteria even before birth. After delivery, they may pass into breast milk. This early disrupted microbiome can slow immune system development, raise allergy risks, and affect digestion.
If you’re wondering what disrupts the gut microbiome before a child is even born, maternal antibiotic use is one major factor. Limiting unnecessary prescriptions during pregnancy can protect both mother and child.
Impact of antibiotic administration directly to infants on the infant gut microbiota
Infants given antibiotics, often for ear or respiratory infections, lose key bacteria needed for digestion and immunity. This dysbiosis can last months, delaying healthy microbiota restoration.
Long-term, it may affect metabolism, immunity, and even mood through the gut-brain axis. Parents should discuss risks and benefits with a pediatrician before starting treatment.
Impact of antibiotics on the gut and oral microbiota in adults
Adults also experience a disrupted microbiome when taking antibiotics. Broad-spectrum drugs can wipe out microbial diversity, making it easier for harmful bacteria to overgrow. After taking antibiotics, this may result in inflammation, yeast infections, or diarrhea.
Oral bacteria can also shift, raising cavity or gum disease risks. Supporting gut health with prebiotics and probiotics during and after treatment helps reduce long-term effects of antibiotics.
Consequences of Antibiotic-Induced Microbiota Changes for Health and Disease
In adults
When antibiotics disrupt gut microbiome, nutrient absorption drops, immunity weakens, and harmful microbes thrive. This is why the link between antibiotics and immune system function is critical. Adults with a disrupted microbiome may face digestive issues, fatigue, and greater infection risk. Over time, long-term effects of antibiotics can include chronic gut disorders or increased susceptibility to pathogens.
During pregnancy and infancy
Changes to a baby’s microbiota can have lifelong effects. A newborn exposed to antibiotics directly or via the mother may face altered immune response modulation, raising risks for asthma, eczema, and food allergies. Understanding what disrupts gut microbiome in early life can help families make informed decisions. Proper use of antibiotics in these stages helps prevent antibiotics weakening the immune system from becoming a reality for the child later.
Changes in immune response
Good germs help your body learn to fight infection. When antibiotics lower those germs, your immune response modulation changes. Your body may react more to germs or fight less well. That means can antibiotics weaken the immune system? Yes, they can. Especially if they throw off the balance of germs.
Influence of Antibiotic-Induced Changes on Microbiota Functionality and Bacterial Behavior at the Single-Cell Level
Changes in metabolites
Gut microbes create metabolites that help digest fiber, make vitamins, and regulate inflammation. When antibiotics reduce these bacteria, metabolite production drops. This may impact the gut-brain axis and impede healing.
Accumulation of metabolites/xenobiotics
Without the right bacteria to break them down, waste and toxins called xenobiotics, build up in the gut. This can trigger inflammation after antibiotics, bloating, and poor nutrient absorption.
Changes in bacterial signaling pattern
Bacteria communicate through chemical signals. Antibiotics can distort these messages, making it harder for good bacteria to coordinate defense. This impacts digestion, immunity, and overall microbiota balance.
ARG reservoir
An antibiotic resistance gene (ARG) reservoir forms when surviving bacteria develop resistance. These genes can spread to other microbes, making future infections harder to treat and threatening both gut and systemic health.
Non-microbiota-associated effects of antibiotics
In pregnancy
Antibiotics may reach the fetus. They may slightly raise the risk of allergies or asthma. They may also affect how the baby’s immune system learns early on.
General effects
Antibiotics can cause side effects. You may get rashes or tummy pain. Sometimes you feel dizzy or nauseous. It is not about the microbiome. Still, it matters.
Antibiotic alternatives and use of probiotics for restoring the microbial community and betterment of health
Sometimes doctors use other options like narrow-target antibiotics. They aim at only the bad germs. Or they use shorter courses.
Probiotics are live good germs you can take in food or supplements. They help bring back good germs. You can also eat prebiotics and probiotics in yogurt, kefir, or fermented veggies.
These help with microbiota restoration. They help build beneficial bacteria again. They help your gut return to normal faster. This can help avoid long-term effects of antibiotics like weak immunity or tummy troubles.
The Bottom Line
Antibiotics can heal infections. But they can also disrupt gut microbiomes. They may weaken the immune system and harm gut health. This can affect babies, kids, and adults. But you can help. Eat good food. Use probiotics. Talk to your doctor. They can help avoid trouble. You don’t have to suffer. Your gut can heal. Let it.
Frequently Asked Questions
Do antibiotics mess up the gut microbiome?
Yes. Antibiotics disrupt gut microbiome balance by killing both harmful and good bacteria, reducing microbial diversity and affecting digestion, immunity, and overall health. Effects may last weeks or months without proper care.
How long to restore gut microbiome after antibiotics?
Recovery can take weeks to months. Diet rich in fiber, prebiotics and probiotics, and avoiding unnecessary antibiotic use can speed microbiota restoration and help prevent long-term effects of antibiotics.
How to protect gut microbiome while on antibiotics?
Eat high-fiber foods, take probiotics, and avoid processed sugar. Ask your doctor for narrow-spectrum antibiotics when possible. This limits what disrupts gut microbiome and helps retain beneficial bacteria.
Why is my gut messed up after antibiotics?
A disrupted microbiome from antibiotics reduces bacteria that aid digestion and immune defense. This imbalance can cause bloating, diarrhea, or food sensitivities until healthy bacteria repopulate.
What happens to your gut when you take too many antibiotics?
Excessive use increases antibiotic resistance, lowers microbial diversity, and weakens immunity. The body’s ability to fight infections drops, and can antibiotics weaken the immune system becomes a real concern.
Can antibiotics permanently damage the microbiome?
Yes, repeated or prolonged antibiotic use can cause lasting harm to the microbiome. However, healthy diet, probiotics, and avoiding unnecessary use can reduce long-term effects of antibiotics.
Do antibiotics kill both good and bad bacteria?
Yes. What are antibiotics designed to do is kill bacteria. But they cannot always tell good from bad, so beneficial bacteria also die, leading to a disrupted microbiome.
About The Author

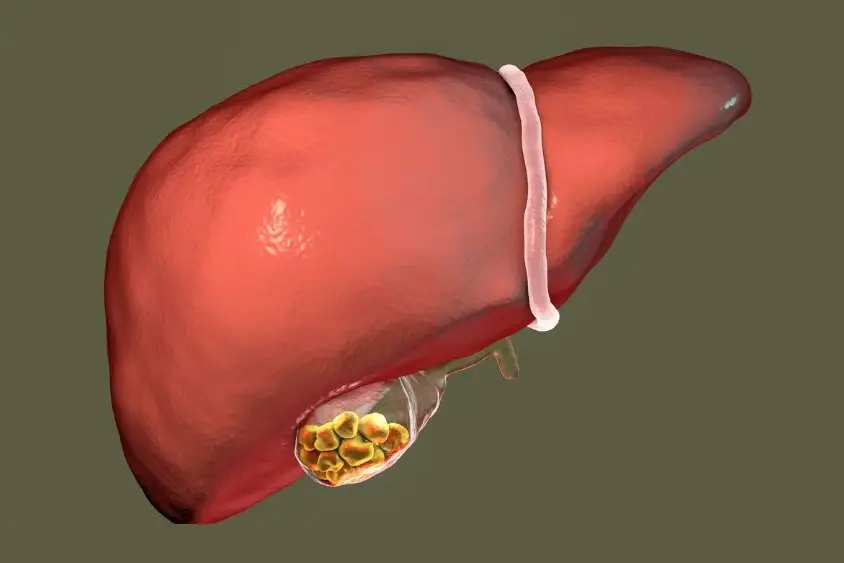
Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.