Colorectal cancer is a disease that starts in the colon or rectum, which are parts of your large intestine. It often begins as small growths called polyps. Over time, some polyps can slowly turn into cancer if they stay unnoticed.
Table of Contents
ToggleScreening for colorectal cancer focuses on finding these polyps or early cancers before they cause harm. Through stool tests and visual exams like colonoscopy, screening for colorectal cancer can catch hidden bleeding, abnormal cells, or early tumors.
In many cases, screening prevents cancer by removing risky polyps early. Regular screening for colorectal cancer , started at the right age and repeated on schedule, remains one of the most effective ways to lower death rates from this disease.
What Is Colorectal Cancer Screening?
Screening for colorectal cancer is a planned check of your colon (large intestine) and rectum. You do it when you have no warning signs. Screening is not the same as testing because of symptoms. If you have bleeding, belly pain, or a major change in stools, you need diagnostic care. Screening is for the “before” stage.
Purpose Of Colorectal Screening Tests
Find polyps or cancer early and stop cancer from forming by removing certain polyps. Colonoscopy can do that in one visit.
A test for colorectal screening can also help you avoid emergency care later. Late disease can cause bowel blockage or heavy bleeding. Screening aims to prevent those crises.
How Screening Helps In Early Detection Of Colorectal Cancer
Many early cancers bleed a tiny amount. Stool tests can pick up hidden blood. Visual tests can spot small growths. That supports early detection of colorectal cancer when treatment is often simpler.
Screening also helps because it is repeated. One normal test does not protect you forever. Regular screening for colorectal cancer involves checking as you age.
Why Early Detection Of Colorectal Cancer Matters
Catching colorectal cancer early changes what happens next. It can change the type of treatment. It can change how long treatment lasts. It can change survival.
How Early-Stage Colorectal Cancer Differs From Late-Stage
Early-stage cancer stays in the colon or rectum. It may not reach lymph nodes (small immune glands). It has not spread to organs like the liver.
Late-stage cancer may spread to lymph nodes or distant organs. Doctors call that metastatic disease (spread). Treatment then often needs more than surgery. It may include chemo (medicine that kills cancer cells).
This gap explains why screening for colorectal cancer matters even when you feel fine.
Survival Rates With Early Detection
Survival rates vary by stage. U.S. SEER data show about a 91% 5-year relative survival for localized colorectal cancer. When cancer is distant, the 5-year relative survival drops to about 16%. Early finding helps many people live longer. That is a key reason to keep up with screening for colorectal cancer .
Impact Of Screening On Mortality Reduction
Screening does more than “find.” It lowers deaths in real studies. Long-term follow-up of randomized screening trials with fecal occult blood testing showed lower colorectal cancer deaths over decades. There is hard evidence that screening for colorectal cancer can save lives.
Colorectal Cancer Screening Age Guidelines
Age rules help you start at the right time. Many people used to start at 50. Several major guidelines now start earlier.
Recommended Screening Age For Average-Risk Adults
If you have average risk, the common starting point is 45. The U.S. Preventive Services Task Force recommends starting at 45 and continuing to 75. The American Cancer Society also recommends starting at 45 for average risk. So, for many adults, your screening age for colorectal cancer begins at 45.
Screening Age For High-Risk Individuals
You may need earlier screening if you have a higher risk. Examples include a strong family history, certain genetic syndromes, or long-term inflammatory bowel disease. If you fit a high-risk group, your clinician may set a different screening age for colorectal cancer and a different test plan.
When To Start Screening Earlier Than Average
You often start earlier than 45 if a close relative had colorectal cancer, especially at a young age. You may also start earlier with Lynch syndrome or familial adenomatous polyposis (inherited conditions that raise risk). You may start earlier if you have had ulcerative colitis or Crohn’s colitis for many years.
The exact age depends on your history. That is why you should share family details and past colon findings. It helps your clinician choose the safest screening plan for colorectal cancer for you.
How Often To Screen For Colorectal Cancer
Timing depends on which test you choose. It also depends on your risk level and your prior results.
Screening Intervals For Stool-Based Tests
Stool tests need repeat schedules. Many guidelines list FIT or high-sensitivity gFOBT yearly. Stool DNA testing can be done every 1 to 3 years. If you pick a stool option, you should stay on schedule. A missed year weakens screening for colorectal cancer .
Screening Intervals For Colonoscopy
For average risk with a normal result, colonoscopy is often recommended every 10 years. If polyps are found, you may need it sooner. The timing depends on the type, size, and number of polyps. That follow-up plan aims to keep screening for colorectal cancer effective.
How Screening Frequency Changes With Age And Risk
Routine screening is required through age 75. From 76 to 85, the decision becomes more personal. It depends on your health, past screening, and your expected benefit. If you have a higher risk, you may need earlier and more frequent checks. Your clinician sets this based on your history.
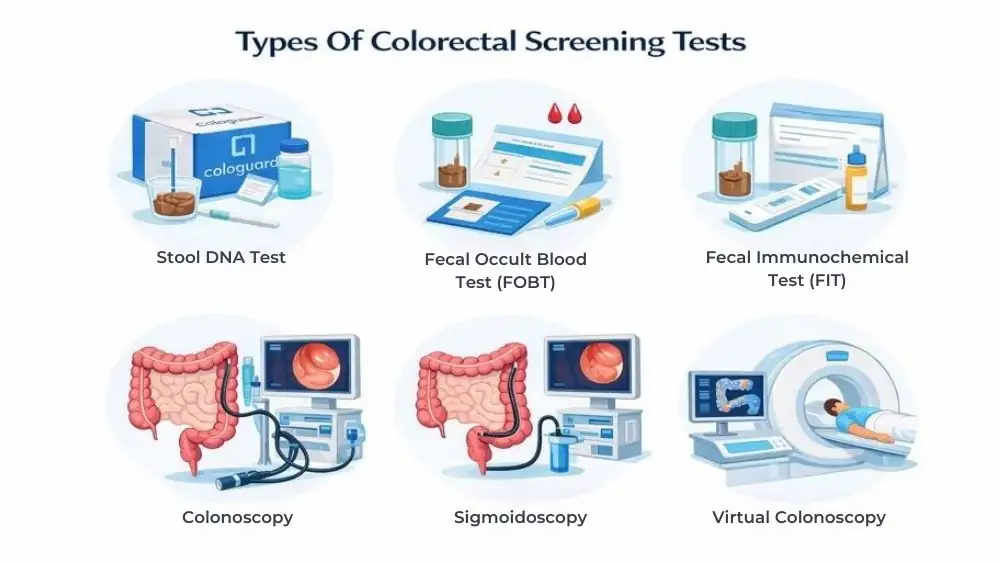
Types Of Colorectal Screening Tests
Stool-based tests look for signs of cancer in stool. Visual tests look at the colon and rectum directly. Both options can support screening for colorectal cancer . The best choice is the one you will complete and repeat.
Stool-Based Colorectal Screening Tests
These tests are done at home. They often look for hidden blood. Some also look for DNA changes that can happen with cancer. They are less invasive, but a positive result must be followed by a colonoscopy to find the cause.
Direct Visualization Colorectal Screening Tests
These tests let a clinician see the colon. Colonoscopy can also remove many polyps during the same exam. That is a prevention step, not just a check. CT colonography and flexible sigmoidoscopy are other visual options, with their own intervals.
Choosing The Right Colorectal Screening Test
Start with your risk level. Average risk often starts at 45. Higher risk may start earlier. Then consider what you can stick with.
If you avoid procedures, a stool plan may help you begin. If you want a longer interval between tests, a colonoscopy may fit. What matters most is that you commit to screening for colorectal cancer and follow the schedule.
Stool-Based Colorectal Screening Tests
You do stool tests at home by collecting a small sample. A lab checks it for warning signs. Many people start screening for colorectal cancer with stool tests because they feel simple.
A stool result can be negative even if a polyp exists. You need repeat testing on schedule to keep screening for colorectal cancer strong. The USPSTF lists FIT or high-sensitivity gFOBT every year and stool DNA-FIT every 1 to 3 years as options.
Fecal Occult Blood Test (FOBT)
FOBT looks for hidden blood in stool. Some FOBT types react to foods and medicines. That can cause false alarms. Many modern programs use “high-sensitivity” versions to improve results.
FOBT works best when you repeat it yearly. If FOBT shows blood, you need a colonoscopy to find the cause. A positive FOBT is not a cancer diagnosis. It is a signal to check deeper.
When you choose FOBT as your test for colorectal screening , follow the kit steps exactly. Small mistakes can change results.
Fecal Immunochemical Test (FIT)
FIT also checks for hidden blood. FIT aims at human blood proteins. That makes it more specific than older chemical FOBT methods. FIT should be done every year if you choose it.
FIT can miss some polyps and can also miss cancers that do not bleed much that day. That is why regular repeats matter. If FIT comes back positive, you need a colonoscopy soon. Cancers show up most often in the first months after a positive FIT, which supports quick follow-up.
Using FIT for screening for colorectal cancer helps most when you do not delay the next step after a positive test.
Stool DNA Test (Cologuard)
Stool DNA tests look for hidden blood and DNA changes linked to cancer or advanced polyps. The USPSTF lists stool DNA-FIT every 1 to 3 years as a screening option.
This test can trigger more follow-up colonoscopies because false positives can happen. Still, many people like it because you do it at home. If you pick stool DNA as your test for colorectal screening , you still need a colonoscopy after an abnormal result.
Colonoscopy And Other Visual Screening Tests
Visual tests let a clinician see the colon. Some tests can also remove polyps right away. This can prevent cancer, not just find it.
The USPSTF lists colonoscopy every 10 years, CT colonography every 5 years, and flexible sigmoidoscopy every 5 years as options.
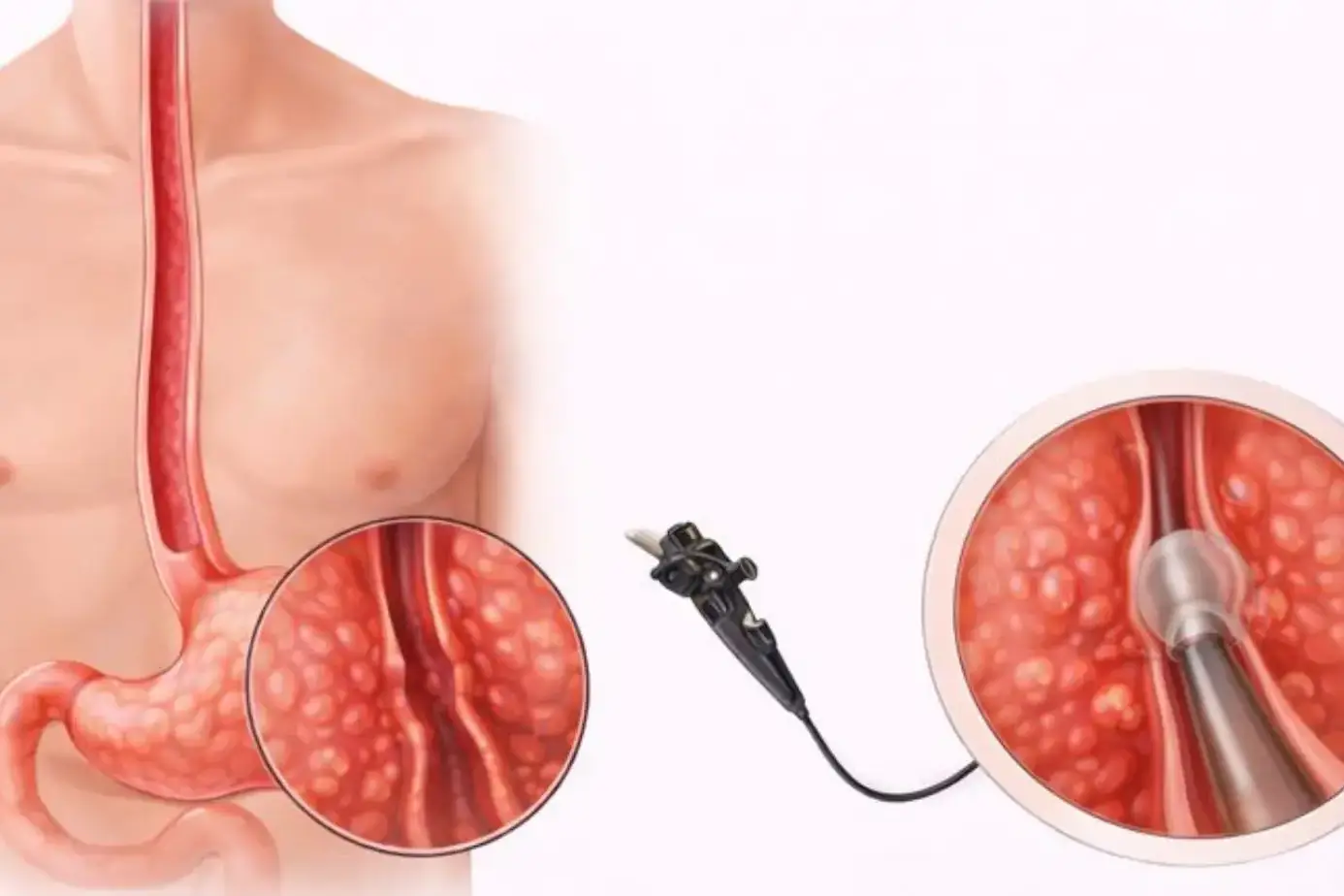
Colonoscopy Procedure Overview
A colonoscopy uses a thin, flexible camera tube. The clinician checks the whole colon and rectum. You usually get sedation (medicine that makes you sleepy).
Colonoscopy can remove many polyps during the exam. That makes it a strong tool for early detection of colorectal cancer and for prevention. A normal colonoscopy often means you can wait 10 years at average risk. Colonoscopy accuracy depends on bowel prep and the quality of the exam. Poor prep can hide polyps.
CT Colonography (Virtual Colonoscopy)
CT colonography uses a CT scan to create images of your colon. You still need bowel prep. A clinician does not place a scope through the whole colon.
The USPSTF lists CT colonography every 5 years as an option. If the scan finds a suspicious spot, you still need a colonoscopy to remove or biopsy it.
Flexible Sigmoidoscopy
Sigmoidoscopy checks the rectum and the lower part of the colon. It does not examine the full colon. This can matter if growths sit higher up.
Sigmoidoscopy is an option every 5 years, or every 10 years with yearly FIT. You might choose it if a full colonoscopy is not available or not a fit. You still need a follow-up colonoscopy after an abnormal result.
Colorectal Cancer Screening For High-Risk Individuals
Average-risk rules do not fit everyone. Your personal risk can change your screening age for colorectal cancer and your test choice.
Family History Of Colorectal Cancer
If a parent, sibling, or child had colorectal cancer, tell your clinician. Age at diagnosis matters. One close relative with early cancer can shift your plan. You may start earlier than 45. You may need a colonoscopy instead of stool testing.
Family history also affects how often you screen. Your clinician may shorten the interval to protect you.
Inflammatory Bowel Disease And Genetic Syndromes
Ulcerative colitis and Crohn’s colitis raise the risk after many years of inflammation. Lynch syndrome and familial adenomatous polyposis raise the risk even more. These conditions need a specialist plan.
Personalized Screening Plans
A good plan uses your family history, your past polyps, and your health. It also looks at what you will truly complete. Consistent screening for colorectal cancer beats a “perfect” plan you skip.
Preparing For Colorectal Screening Tests
Prep affects what the test can see. This matters most for colonoscopy and CT colonography.
Bowel Preparation Requirements
Bowel prep clears stool from your colon. Stool can hide polyps, and poor bowel prep raises miss rates for adenomas (pre-cancer polyps).
Your clinic will give a prep drink and timing steps. Follow them closely and ask questions early. Good prep makes screening for colorectal cancer safer and more useful.
Diet And Medication Adjustments Before Screening
Many clinics ask for a clear-liquid day before a colonoscopy. Some newer guidance suggests limiting diet changes to the day before for many low-risk patients, but your clinic’s instructions matter most.
Ask about blood thinners, diabetes meds, and iron pills. Do not stop meds on your own. Your clinician adjusts them based on your needs.
What To Expect On The Test Day
For a colonoscopy, you arrive on an empty stomach and get sedation. You will need a ride home because you might feel bloated from the air used during the exam.
For stool tests, the “test day” is at home. You collect the sample and send it back fast, as the kit directs.
What Happens After An Abnormal Screening Result
Abnormal does not equal cancer. It means you need a closer look.
Follow-Up Testing After Positive Stool Tests
A positive stool test needs a colonoscopy. Several measures and studies use “within 6 months” as a key target for follow-up colonoscopy after an abnormal stool test. If you delay, you lose the benefit of screening for colorectal cancer .
Diagnostic Colonoscopy After Abnormal Results
During the colonoscopy, the clinician looks for bleeding sources, polyps, or tumors. They can remove polyps and take biopsies (small tissue samples). This is how doctors confirm cancer.
Next Steps If Cancer Or Polyps Are Found
If doctors find polyps, they remove them when possible. Your next screening interval depends on polyp type and number.
If doctors find cancer, they stage it (check how far it has spread). Treatment varies by stage and health. Doctors may use surgery, chemo, radiation, or targeted drugs. Your team will explain options and limits. No single plan fits everyone.
FAQs
Is Colorectal Cancer Screening Painful?
Most stool tests do not hurt. Colonoscopy usually does not hurt because sedation helps. The hardest part is often prep. If you fear pain, tell your clinician. Screening for colorectal cancer should feel manageable, not scary.
Which Colorectal Screening Test Is Most Accurate?
Colonoscopy can find and remove many polyps in one visit. That gives it an advantage for prevention. Still, stool tests help when you repeat them on schedule. The “most accurate” test for colorectal screening depends on your risk and follow-through.
Can Screening Prevent Colorectal Cancer?
Yes, in many cases. Colonoscopy can remove polyps before they turn cancerous. Stool tests can also prevent cancer when they lead to a timely colonoscopy after a positive result. Screening for colorectal cancer protects you best when you act on abnormal results quickly.
Is Colorectal Cancer Screening Covered By Insurance?
Coverage depends on your plan and country. In the U.S., many plans cover recommended screening tests, but details differ. Ask how they cover follow-up colonoscopy after a positive stool test. Screening for colorectal cancer can cost less when coded as preventive care.
Key Takeaways On Colorectal Cancer Screening
Summary Of Screening Options
- Screening for colorectal cancer helps find cancer or risky polyps before symptoms appear, which improves treatment outcomes and survival.
- Most colorectal cancers begin as polyps, and some screening tests can remove these growths before they turn into cancer.
- For adults at average risk, the usual screening age for colorectal cancer starts at 45, based on strong evidence from large population studies.
- People with a family history, genetic conditions, or long-term bowel inflammation often need earlier and more frequent screening for colorectal cancer .
- Stool-based tests, such as FIT, FOBT, and stool DNA tests, are done at home and mainly look for hidden blood or DNA changes linked to cancer.
- Visual tests, including colonoscopy, CT colonography, and flexible sigmoidoscopy, allow doctors to see inside the colon and sometimes remove polyps during the same visit.
- Colonoscopy checks the entire colon and is often repeated every 10 years for average-risk adults with normal results.
- Stool tests must be repeated on a regular schedule to remain effective, and a positive result always requires a follow-up colonoscopy.
- A positive screening result does not mean you have cancer, but it does mean more testing is needed to find the cause.
The best test for colorectal screening is the one you are willing and able to complete on time and repeat as recommended.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin