If you have been diagnosed with Barrett’s esophagus, it is essential to explore the various treatment options available to manage your condition effectively. Barrett’s esophagus occurs when the tissue lining the esophagus becomes abnormal due to acid reflux. This condition can increase the risk of developing esophageal cancer.
Table of Contents
ToggleFortunately, there are several treatment approaches that can help alleviate symptoms and reduce the chances of cancer development. The choice of treatment depends on the extent of abnormal cell growth and overall health.
In this article, we will discuss the diagnosis of Barrett’s esophagus, screening recommendations, and various treatment options based on the degree of dysplasia. We will also explain the importance of periodic surveillance and the role of medication in managing Barrett’s esophagus.
Stay informed and empowered as we dive into the world of effective Barrett’s esophagus treatment options.
Diagnosis of Barrett’s Esophagus
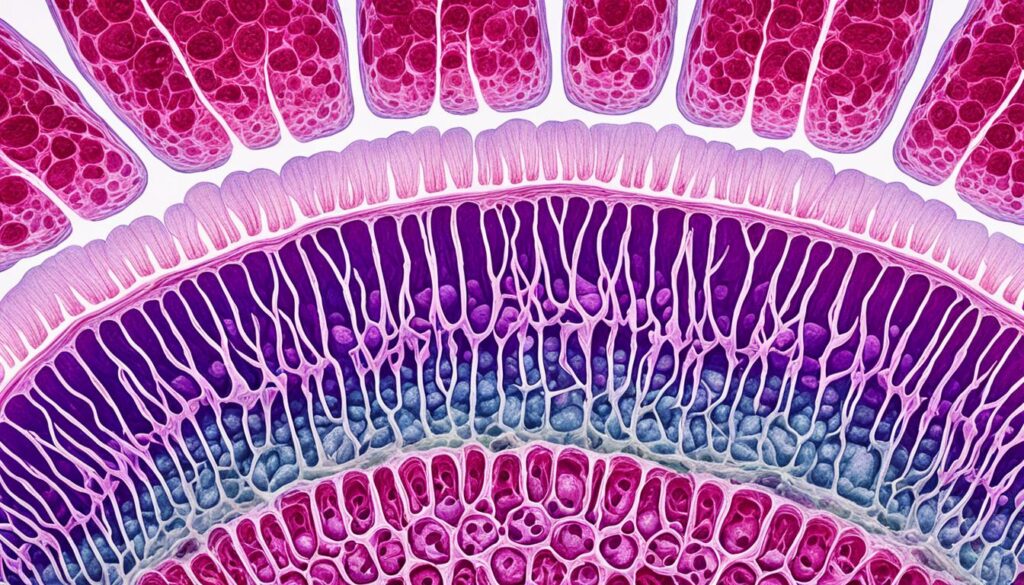
Diagnosing Barrett’s esophagus involves a procedure called endoscopy to examine the tissue lining your esophagus. This is the most effective method for detecting and evaluating any changes that may have occurred. During an endoscopy, a thin, flexible tube with a light and a camera at its tip is inserted through your mouth and into your esophagus. The camera allows the doctor to closely inspect the esophageal lining and identify any abnormalities or tissue changes.
If the doctor observes any suspicious areas, tissue biopsies will be taken for further analysis. These biopsies involve collecting small samples of the esophageal tissue using specialized instruments passed through the endoscope. The samples are then sent to a pathologist who specializes in gastroenterology pathology for examination under a microscope. The pathologist evaluates the tissue samples for the presence and degree of dysplasia – the abnormal growth and structure of cells that can indicate the presence of Barrett’s esophagus.
The degree of dysplasia is crucial in determining the risk of developing esophageal cancer. Dysplasia can range from no dysplasia (absence of abnormal cellular changes) to different levels of low-grade dysplasia (mild to moderate abnormal cellular changes) and even high-grade dysplasia (severe abnormal cellular changes that are often considered a precursor to cancer).
Endoscopy with tissue biopsy is a vital diagnostic tool for determining the presence of Barrett’s esophagus and assessing the severity of dysplasia. Early detection and diagnosis play a crucial role in guiding appropriate treatment decisions and improving patient outcomes.

| Dysplasia Level | Description |
|---|---|
| No Dysplasia | No abnormal cellular changes found in the tissue samples. |
| Low-Grade Dysplasia | Mild to moderate abnormal cellular changes observed in the tissue samples. |
| High-Grade Dysplasia | Severe abnormal cellular changes that may indicate a higher risk of developing esophageal cancer. |
The table above summarizes the different levels of dysplasia and their descriptions based on the assessment of tissue biopsies. It illustrates the spectrum of cellular changes that can occur in Barrett’s esophagus and emphasizes the importance of accurate diagnosis for appropriate treatment planning.
Screening for Barrett’s Esophagus
Screening for Barrett’s esophagus is an important preventive measure for individuals experiencing frequent symptoms of gastroesophageal reflux disease (GERD) and those with specific risk factors. By identifying the presence of Barrett’s esophagus early on, doctors can initiate appropriate treatment strategies to manage the condition effectively.
During the screening process, doctors assess the patient’s risk factors, including:
- Family history of Barrett’s esophagus
- Being male
- Being of white ethnicity
- Being over the age of 50
- Smoking
- Having abdominal fat
If you fall into any of these categories, undergoing an endoscopy exam is highly recommended. This procedure enables doctors to closely examine your esophagus and detect the presence of Barrett’s esophagus. An endoscopy exam involves the insertion of a thin, flexible tube with a camera and light source down your throat to capture detailed images of your esophageal tissue.
Screening Guidelines
Screening guidelines suggest that individuals with frequent GERD symptoms and risk factors should undergo an endoscopy exam every few years. The precise frequency of screening may vary based on individual risk factors and medical history.
To understand the importance of screening, let’s take a look at a table highlighting the main risk factors for Barrett’s esophagus:
| Risk Factors | Prevalence |
|---|---|
| Family History | 10-15% of cases |
| Being Male | 2-3 times more likely |
| White Ethnicity | Higher incidence rates |
| Over Age 50 | Increased risk with age |
| Smoking | Increased risk |
| Abdominal Fat | Higher risk for obesity |
By recognizing these risk factors and prioritizing regular screening, you can take proactive steps towards your health and well-being. Remember, early detection plays a crucial role in ensuring timely intervention and effective management of Barrett’s esophagus.
Treatment for No Dysplasia
If no dysplasia is found in the biopsy, your treatment for Barrett’s esophagus may involve periodic endoscopy to monitor the cells in your esophagus. This is to ensure early detection of any changes that may occur. Additionally, managing your symptoms of gastroesophageal reflux disease (GERD) through medication and lifestyle changes is also recommended.
GERD treatment may include:
- Taking medication such as proton pump inhibitors (PPIs) to reduce the production of stomach acid
- Adopting lifestyle changes like avoiding trigger foods and maintaining a healthy weight
Periodic endoscopy allows your healthcare professional to closely monitor the condition of your esophagus and ensure that any potential issues are addressed in a timely manner.

| Treatment for No Dysplasia | Benefits |
|---|---|
| Periodic endoscopy | Allows for monitoring of esophagus cells |
| GERD treatment | Helps manage symptoms and prevent further damage |
Treatment for Low-Grade Dysplasia
Individuals with low-grade dysplasia have several treatment options available to manage their condition effectively. These options aim to remove damaged cells and prevent the progression of dysplasia to more severe stages. Treatment for low-grade dysplasia in Barrett’s esophagus often involves a combination of endoscopic resection, radiofrequency ablation, cryotherapy, and ongoing management of GERD.
Endoscopic Resection:
Endoscopic resection is a minimally invasive procedure that allows for the removal of abnormal cells in the esophagus. During this procedure, a thin tube with a camera and specialized instruments is inserted through the mouth and guided to the affected area. The abnormal tissue is carefully removed, reducing the risk of further complications and progression of dysplasia.
Radiofrequency Ablation:
Radiofrequency ablation is another effective treatment option for low-grade dysplasia. It uses heat energy to destroy abnormal tissue in the esophagus. A specialized device is used to deliver controlled radiofrequency waves to the affected area, effectively eliminating the dysplastic cells. This treatment helps to restore healthy tissue and reduce the risk of cancer development.
Cryotherapy:
Cryotherapy involves the application of extremely cold temperatures to the affected cells in the esophagus. This freezing technique helps to destroy the abnormal tissue. A freezing agent, typically liquid nitrogen or carbon dioxide, is sprayed or circulated through a specialized device to target and eliminate the dysplastic cells. Cryotherapy is a safe and effective treatment option for low-grade dysplasia.

These treatment options can be used individually or in combination, depending on the specific case and the discretion of the healthcare provider. It is important to note that these treatments are typically accompanied by ongoing management of GERD symptoms and regular follow-up endoscopies to monitor the progress of dysplasia.
Next, we will discuss the treatment options for individuals with high-grade dysplasia, a more advanced stage of Barrett’s esophagus.
Treatment for High-Grade Dysplasia
If high-grade dysplasia is detected during the evaluation of Barrett’s esophagus, prompt treatment is crucial as it is considered a precursor to esophageal cancer. Several treatment options may be considered based on the individual’s health condition and the extent of dysplasia. These options include:
1. Endoscopic Resection
Endoscopic resection is a minimally invasive procedure that involves removing the damaged tissue in the esophagus using specialized tools passed through an endoscope. This procedure allows for precise targeting and removal of the dysplastic cells while sparing the remaining healthy tissue. Endoscopic resection is often recommended for localized areas of high-grade dysplasia.
2. Radiofrequency Ablation
Radiofrequency ablation (RFA) is a technique that uses heat energy to destroy the abnormal cells in the esophagus. During the procedure, a catheter with a specialized electrode is inserted through an endoscope and applied to the targeted area. The heat generated by the electrode destroys the dysplastic cells, allowing for the regrowth of healthy tissue. RFA is commonly used to treat larger areas of high-grade dysplasia.
3. Cryotherapy
Cryotherapy is a treatment method that involves freezing the dysplastic cells in the esophagus. Liquid nitrogen or a specialized cryoprobe is applied directly to the targeted area, causing the abnormal cells to freeze and subsequently die off. Cryotherapy is effective for both small and large areas of high-grade dysplasia.
4. Surgery
In cases where endoscopic treatments are insufficient or not advisable, surgery may be considered for the management of high-grade dysplasia. Surgical intervention involves the removal of the damaged part of the esophagus and reconnecting the remaining portion to the stomach. This procedure is known as esophagectomy and can be performed using open surgery or minimally invasive techniques like laparoscopy.
Following the treatment of high-grade dysplasia, lifelong medication to reduce acid production may be prescribed to prevent the recurrence of dysplastic cells and further protect the esophageal lining. Additionally, regular follow-up testing and surveillance endoscopies are essential to monitor for any changes and ensure early detection of any potential complications.
| Treatment Options | Procedure Description |
|---|---|
| Endoscopic Resection | Removal of dysplastic cells using specialized endoscopic tools |
| Radiofrequency Ablation (RFA) | Application of heat energy to destroy abnormal cells |
| Cryotherapy | Freezing of dysplastic cells using liquid nitrogen or cryoprobe |
| Surgery (Esophagectomy) | Removal of damaged part of the esophagus and reconnection of remaining portion to the stomach |
Periodic Surveillance Endoscopy
Periodic surveillance endoscopy is an essential aspect of managing Barrett’s esophagus. It involves regular examinations to monitor for signs of cancer development and assess the progression of dysplasia. Surveillance endoscopy plays a crucial role in identifying any changes in the esophageal tissue and detecting the presence of cancerous cells.
The frequency of surveillance endoscopies depends on the severity of dysplasia present. Individuals with high-grade dysplasia often require more frequent evaluations to closely monitor their condition and minimize the risk of cancer. Conversely, those with low-grade or no dysplasia may undergo less frequent endoscopies, primarily to track any changes in their esophageal health.
During a surveillance endoscopy, biopsies may be performed to obtain tissue samples from the esophagus. These samples are then examined by a pathologist to check for the presence of cancerous cells. Biopsies provide valuable information about the risk of cancer development and help guide future treatment decisions.
Regular surveillance endoscopies, combined with appropriate interventions, can significantly improve the management of Barrett’s esophagus and reduce the risk of cancer progression.

| Severity of Dysplasia | Frequency of Surveillance Endoscopies |
|---|---|
| No dysplasia or low-grade dysplasia | Every 1-3 years |
| High-grade dysplasia | Every 3-6 months |
Medication for Barrett’s Esophagus
When it comes to managing Barrett’s esophagus and GERD, medication plays a crucial role in reducing acid production and preventing further damage to the esophagus. One commonly prescribed type of medication is proton pump inhibitors (PPIs), which are highly effective in suppressing acid in the stomach.
Proton Pump Inhibitors (PPIs)
PPIs work by inhibiting the enzyme responsible for acid production in the stomach, effectively reducing the amount of acid that can reflux into the esophagus. These acid-suppressing medicines provide relief from heartburn and other symptoms of GERD. They also help heal the lining of the esophagus and reduce the risk of complications associated with Barrett’s esophagus.
Commonly prescribed PPIs include:
- Esomeprazole (Nexium)
- Omeprazole (Prilosec)
- Lansoprazole (Prevacid)
- Pantoprazole (Protonix)
- Rabeprazole (Aciphex)
It’s important to take PPIs as prescribed by your healthcare provider. These medications are usually taken once a day before a meal. However, the dosage and frequency may vary depending on the severity of your symptoms and the extent of Barrett’s esophagus.
Other Medications
In addition to PPIs, your doctor may recommend other medications to complement the treatment of Barrett’s esophagus and GERD. These may include:
- Antacids: Over-the-counter antacids provide temporary relief from heartburn by neutralizing stomach acid.
- H2 Blockers: H2 blockers work by reducing the production of stomach acid and can provide longer-lasting relief than antacids.
- Prokinetic Agents: Prokinetic agents help improve the movement of the digestive system, preventing acid from refluxing into the esophagus.
It’s important to discuss the use of these medications with your healthcare provider to ensure they are appropriate for your specific condition and to avoid any potential drug interactions.
| PPI | Brand Name |
|---|---|
| Esomeprazole | Nexium |
| Omeprazole | Prilosec |
| Lansoprazole | Prevacid |
| Pantoprazole | Protonix |
| Rabeprazole | Aciphex |
Endoscopic Ablative Therapies
When it comes to treating dysplastic cells in the esophagus, endoscopic ablative therapies offer effective solutions. These procedures are performed by specialized gastroenterologists or surgeons and include:
- Photodynamic Therapy: Using light-activated chemicals, photodynamic therapy targets and destroys abnormal cells in the esophagus. The light activates the chemicals, which then selectively destroy the dysplastic tissue.
- Radiofrequency Ablation: In this procedure, radio waves are used to selectively kill the abnormal cells in the esophagus. By applying controlled heat, radiofrequency ablation destroys the dysplastic tissue while minimizing damage to surrounding healthy tissue.
- Endoscopic Mucosal Resection: This technique involves removing the affected tissue from the esophagus. The procedure is done using instruments passed through an endoscope, allowing for precise and targeted removal.
These endoscopic ablative therapies offer minimally invasive alternatives to surgery, providing patients with effective treatment options for dysplastic cells in the esophagus. Your healthcare professional will determine the most appropriate therapy based on your individual condition and needs.
| Procedure | Benefits |
|---|---|
| Photodynamic Therapy |
|
| Radiofrequency Ablation |
|
| Endoscopic Mucosal Resection |
|
Surgery for Barrett’s Esophagus
If other treatments have not been effective in managing your Barrett’s esophagus or if you prefer a surgical approach, surgery may be considered as an option. Two common surgical procedures for Barrett’s esophagus are esophagectomy and Nissen fundoplication.
Esophagectomy
Esophagectomy is a surgical procedure that involves the removal of the affected sections of the esophagus. After removing the damaged tissue, the remaining esophagus is reconstructed using tissue from either the stomach or the large intestine. This procedure is typically performed by a team of surgeons and may require a hospital stay.
Nissen Fundoplication
Nissen fundoplication is a surgical procedure that aims to treat both Barrett’s esophagus and gastroesophageal reflux disease (GERD). During the procedure, the upper part of the stomach is wrapped around the lower esophagus to strengthen the lower esophageal sphincter and prevent acid reflux. Nissen fundoplication can be performed using traditional open surgery or minimally invasive laparoscopic surgery.
Benefits of Laparoscopic Surgery
Laparoscopic surgery, also known as keyhole surgery, is a minimally invasive approach that offers several benefits compared to traditional open surgery:
- Smaller incisions, resulting in less pain and scarring
- Shorter hospital stay and faster recovery time
- Reduced risk of complications, such as infection
- Quicker return to normal activities
If you and your healthcare team determine that surgery is the best option for your Barrett’s esophagus, they will discuss the specific procedure and any potential risks or benefits with you. It’s important to have a thorough understanding of the surgical options and to ask any questions you may have.
Surgical Treatment Options for Barrett’s Esophagus
| Surgical Procedure | Description |
|---|---|
| Esophagectomy | Surgical removal of the affected sections of the esophagus and reconstruction using tissue from the stomach or large intestine. |
| Nissen Fundoplication | Wrapping the upper part of the stomach around the lower esophagus to strengthen the lower esophageal sphincter and prevent acid reflux. |
Conclusion
In conclusion, there are several effective treatment options available for managing Barrett’s esophagus. The choice of treatment depends on the extent of dysplasia and individual health factors. It is important to work closely with healthcare professionals to determine the most suitable approach for your specific condition.
Medication, such as proton pump inhibitors, can help reduce acid production and prevent further damage to the esophagus. Endoscopic ablative therapies, including photodynamic therapy, radiofrequency ablation, and endoscopic mucosal resection, are procedures that target and destroy dysplastic cells in the esophagus.
In some cases, surgery may be necessary, such as esophagectomy or Nissen fundoplication. Lifestyle changes, such as maintaining a healthy weight and avoiding trigger foods, can also play a role in managing symptoms. Periodic surveillance is crucial for monitoring the condition and detecting any changes.
Remember, early detection and intervention are key to preventing further complications. By staying proactive and working closely with your healthcare team, you can effectively manage Barrett’s esophagus and ensure the best possible outcomes for your long-term health.
FAQ
What is Barrett’s esophagus?
Barrett’s esophagus is a condition in which the lining of the esophagus is damaged, usually by acid reflux. This can lead to changes in the cells of the esophagus and increase the risk of developing esophageal cancer.
How is Barrett’s esophagus diagnosed?
Barrett’s esophagus can be diagnosed through an endoscopy procedure. During the endoscopy, a thin tube with a camera is inserted into the esophagus to examine the tissue. Biopsies may be taken to determine the degree of dysplasia present.
Who should be screened for Barrett’s esophagus?
Individuals with frequent GERD symptoms and certain risk factors should be screened for Barrett’s esophagus. Risk factors include a family history of the condition, being male, being white, being over 50, being a smoker, or having abdominal fat.
What are the treatment options for no dysplasia in Barrett’s esophagus?
If no dysplasia is found in the biopsy, treatment for Barrett’s esophagus may involve periodic endoscopy to monitor the esophagus cells. GERD treatment, including medication and lifestyle changes, is also recommended to manage symptoms.
What are the treatment options for low-grade dysplasia in Barrett’s esophagus?
Treatment options for low-grade dysplasia may include endoscopic resection, radiofrequency ablation, or cryotherapy. These treatments aim to remove or destroy the abnormal cells. GERD treatment and regular follow-up endoscopies are also recommended.
What are the treatment options for high-grade dysplasia in Barrett’s esophagus?
High-grade dysplasia is considered a precursor to esophageal cancer. Treatment options may include endoscopic resection, radiofrequency ablation, cryotherapy, or surgery. Surgery involves removing the damaged part of the esophagus and reconnecting the remaining portion to the stomach.
How often should surveillance endoscopy be performed for Barrett’s esophagus?
Periodic surveillance endoscopy is recommended for individuals with Barrett’s esophagus to monitor for signs of cancer development. The frequency of endoscopies depends on the severity of dysplasia, with high-grade dysplasia requiring more frequent evaluations.
What medications are prescribed for Barrett’s esophagus?
Medications, specifically proton pump inhibitors (PPIs), are often prescribed for individuals with Barrett’s esophagus and GERD. PPIs help reduce acid production and can prevent further damage to the esophagus. Other medications, such as antacids and H2 blockers, may be used in combination with PPIs.
What are endoscopic ablative therapies for Barrett’s esophagus?
Endoscopic ablative therapies are procedures used to destroy dysplastic cells in the esophagus. These include photodynamic therapy, radiofrequency ablation, and endoscopic mucosal resection. These procedures are performed by gastroenterologists or surgeons.
When is surgery considered for Barrett’s esophagus?
Surgery, such as esophagectomy or Nissen fundoplication, may be considered for individuals who do not respond to other treatments or prefer a surgical approach. Esophagectomy involves removing the affected sections of the esophagus and reconstructing it using tissue from the stomach or large intestine.
Source Links


