Welcome to our comprehensive guide on understanding and managing Barrett’s Esophagus with Dysplasia. In this article, we will explore the risk factors associated with this condition, the available treatment options, and the importance of maintaining digestive health.
Table of Contents
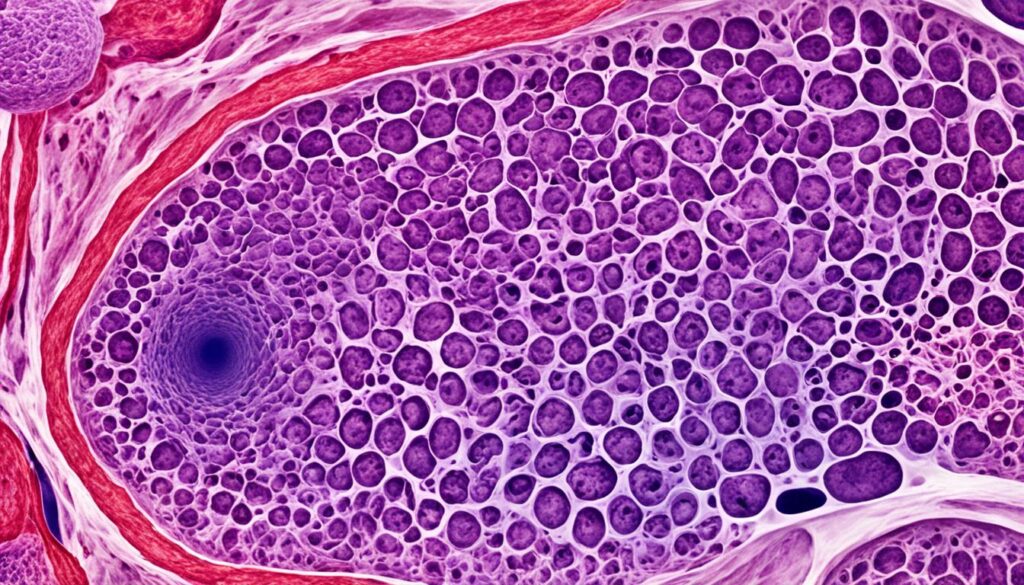
ToggleBarrett’s Esophagus is a condition where the normal tissue lining the esophagus is replaced by tissue similar to that of the intestinal lining. It is typically diagnosed through biopsy samples taken during an endoscopy. The presence of dysplasia, a pre-cancerous stage where the cells in Barrett’s Esophagus become more abnormal, plays a crucial role in managing the condition.
People with Barrett’s Esophagus have a higher risk of developing esophageal cancer, although it is important to note that most individuals with this condition do not develop cancer. Treatment options for Barrett’s Esophagus with Dysplasia vary depending on the degree of dysplasia and may include regular monitoring, medication, endoscopic resection, radiofrequency ablation, or surgery.
In this article, we will delve deeper into the definition of Barrett’s Esophagus, explore the risk factors associated with this condition, discuss the diagnosis and various treatment options available, and provide insights on how to manage and maintain digestive health when dealing with Barrett’s Esophagus with Dysplasia.
Read on to gain valuable knowledge and practical advice on understanding and managing Barrett’s Esophagus with Dysplasia for a healthier digestive system. Let’s empower ourselves to make informed decisions and take control of our well-being.
What is Barrett’s Esophagus?
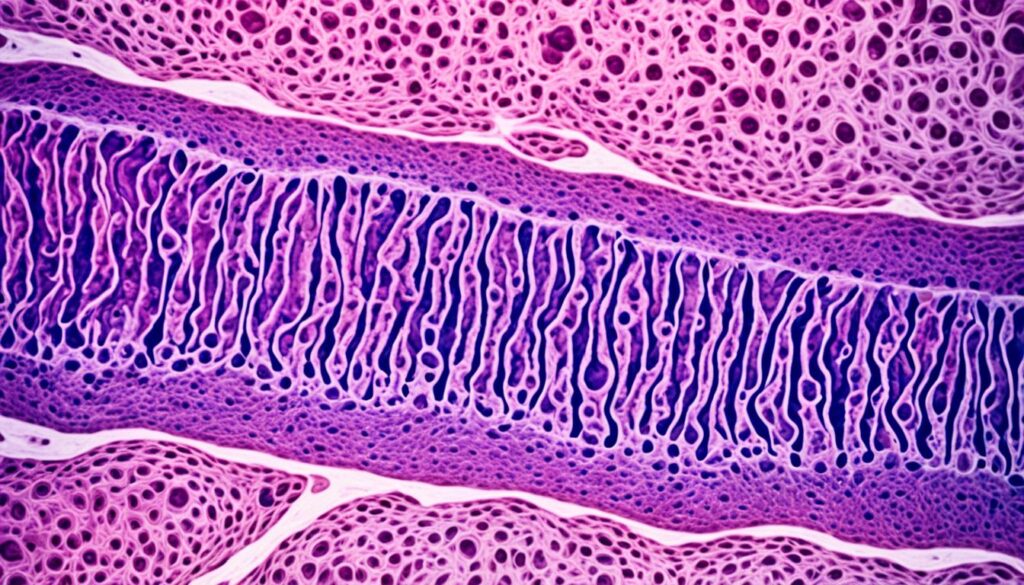
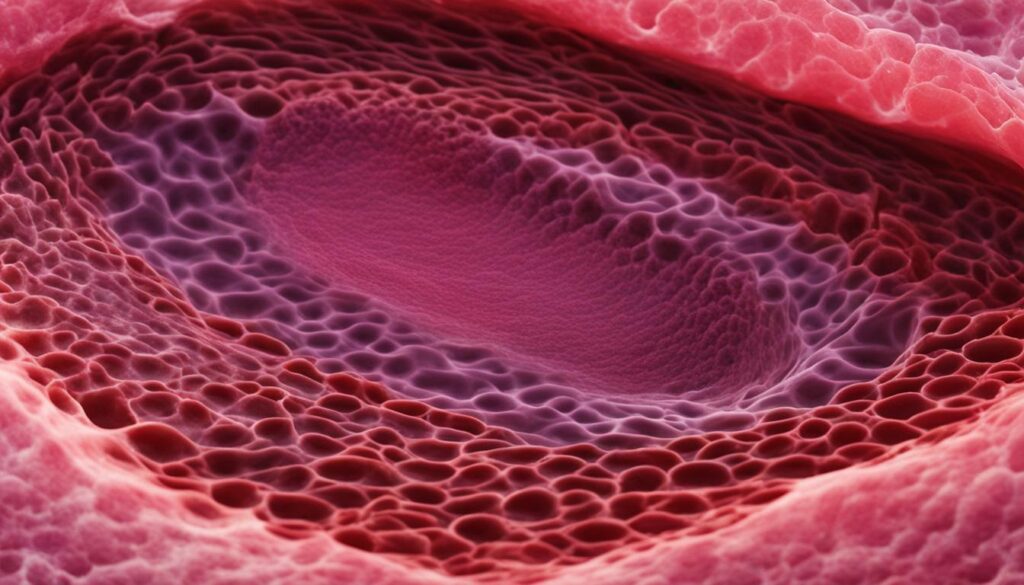
The esophagus is a tube that connects your mouth to your stomach. It plays a crucial role in the digestion process by carrying food and liquids from your mouth to your stomach. At the gastro-esophageal junction, there is a ring of muscle called the lower esophageal sphincter that allows the passage of food and liquids into the stomach.
In a healthy esophagus, the lining is made up of squamous cells, which are flat and thin. However, in some cases, long-term exposure to stomach acid can cause the normal squamous cells to be replaced by a different type of cell called goblet cells. Goblet cells are glandular cells typically found in the intestinal lining.
When the esophagus undergoes this change in cell type, it is referred to as Barrett’s esophagus. It is a condition where the squamous cells are replaced by goblet cells in the lining of the esophagus, typically in response to chronic acid reflux.
| Normal Esophagus | Barrett’s Esophagus |
|---|---|
| Squamous cells | Goblet cells |
| Flat and thin cells | Glandular cells found in the intestines |
This change in cell composition can be visually identified during an endoscopy, which is a procedure where a flexible tube with a camera is inserted into the esophagus to examine the lining. The presence of goblet cells in the esophageal lining confirms the diagnosis of Barrett’s esophagus.
It is important to note that Barrett’s esophagus itself is not a cancerous condition, but it does increase the risk of developing esophageal cancer over time. Regular monitoring and appropriate management are necessary to reduce this risk and ensure overall digestive health.
References:
- American Society for Gastrointestinal Endoscopy (ASGE). (n.d.). Barrett’s Esophagus. Retrieved from https://www.asge.org/home/for-patients/patient-information/understanding-barrett-s-esophagus
- Mayo Clinic. (2021, June 19). Barrett’s Esophagus. Retrieved from https://www.mayoclinic.org/diseases-conditions/barretts-esophagus/symptoms-causes/syc-20352810
Risk Factors for Barrett’s Esophagus
Barrett’s esophagus is influenced by several risk factors that increase the likelihood of its development. By understanding these risk factors, you can take proactive steps to protect your digestive health. The primary risk factor for Barrett’s esophagus is gastroesophageal reflux disease (GERD), a condition in which stomach acid flows back into the esophagus. Other significant risk factors include:
- Obesity: Excessive weight can put pressure on the stomach, causing acid reflux and increasing the risk of Barrett’s esophagus.
- Smoking: Tobacco smoke can weaken the lower esophageal sphincter, allowing stomach acid to flow into the esophagus more easily.
- Age: Individuals over the age of 50 are at a higher risk, as the incidence of Barrett’s esophagus tends to increase with age.
- Gender: Men are more likely to develop Barrett’s esophagus than women.
- Race: Caucasians are more susceptible to Barrett’s esophagus compared to other ethnic groups.
- Family History: If you have a family member with Barrett’s esophagus or esophageal cancer, your risk may be elevated.
- Abdominal Fat: Excess abdominal fat, particularly around the waist, can increase the risk of Barrett’s esophagus.
While men have a higher likelihood of developing Barrett’s esophagus, it’s essential for women to be aware of the risks as well, especially if they experience uncontrolled reflux or have other risk factors. By addressing these risk factors and adopting a healthier lifestyle, you can reduce the chances of developing Barrett’s esophagus.
| Risk Factors | Potential Impact |
|---|---|
| Gastroesophageal reflux disease (GERD) | Increases the risk of Barrett’s esophagus |
| Obesity | Exacerbates acid reflux and raises the likelihood of developing Barrett’s esophagus |
| Smoking | Weakens the lower esophageal sphincter, increasing the risk of acid reflux and Barrett’s esophagus |
| Age over 50 | Elevates the risk due to increased incidence with advancing age |
| Gender (male) | Men are more prone to developing Barrett’s esophagus compared to women |
| Race (Caucasian) | Caucasians have a higher susceptibility to Barrett’s esophagus |
| Family History | A family history of Barrett’s esophagus or esophageal cancer increases the risk |
| Abdominal Fat | Excess abdominal fat, particularly around the waist, raises the likelihood of developing Barrett’s esophagus |

Diagnosis of Barrett’s Esophagus with Dysplasia
Diagnosing Barrett’s esophagus with dysplasia involves a thorough evaluation using a procedure called endoscopy. During this procedure, a flexible tube equipped with a camera is inserted into the esophagus to examine the tissue for any signs of abnormal changes. This allows healthcare professionals to visually assess the condition and determine the extent of dysplasia present.
In addition to the visual examination, tissue samples, known as biopsies, are taken during the endoscopy. These biopsies are then sent to a pathologist for further analysis. The pathologist carefully examines the samples under a microscope to identify the presence of dysplasia and assess the degree of abnormal cell changes.
The degree of dysplasia detected plays a crucial role in determining the appropriate treatment approach. Dysplasia can be classified into three levels:
- No Dysplasia: This indicates the absence of abnormal cell changes in the esophagus.
- Low-Grade Dysplasia: In this stage, there are mild abnormal cell features present.
- High-Grade Dysplasia: This stage represents more advanced and severe abnormal cell changes, indicating a higher risk of developing esophageal cancer.
By accurately diagnosing Barrett’s esophagus with dysplasia and determining the degree of dysplasia, healthcare providers can develop an individualized treatment plan to effectively manage the condition and reduce the risk of progression to cancer.
Management of Barrett’s Esophagus with Dysplasia
When it comes to managing Barrett’s esophagus with dysplasia, a personalized approach is essential. The management plan will depend on the level of dysplasia present in the esophageal tissue. Regular monitoring through endoscopy exams is typically recommended to closely observe any changes in the condition.
Medication can play a crucial role in the management of Barrett’s esophagus with dysplasia. Proton pump inhibitors, commonly prescribed, help reduce acid reflux and protect the delicate lining of the esophagus. They work by decreasing the production of stomach acid, providing relief and minimizing the risk of further damage.
In addition to medication and regular monitoring, follow-up care is crucial in managing Barrett’s esophagus with dysplasia. This includes maintaining a healthy lifestyle, managing any underlying conditions that can exacerbate symptoms, and adhering to the treatment plan provided by your healthcare professional.
There are various treatment options available depending on the degree of dysplasia. Let’s take a closer look at these options:
| Treatment Options | Description |
|---|---|
| Endoscopic Resection | This procedure involves removing abnormal tissue through an endoscope. It is often recommended for low-grade dysplasia. |
| Radiofrequency Ablation | This technique uses heat energy to destroy dysplastic cells. It can be effective for both low-grade and high-grade dysplasia. |
| Surgery | In some cases, surgery to remove the abnormal tissue or even part of the esophagus may be necessary, especially for high-grade dysplasia. |
These treatment options aim to remove or destroy the abnormal cells and reduce the risk of further progression to esophageal cancer. The choice of treatment will depend on the individual’s specific circumstances and should be discussed with a healthcare professional.
Remember, effective management of Barrett’s esophagus with dysplasia requires a collaborative approach between you and your healthcare team. By staying proactive, adhering to your treatment plan, and attending regular follow-up appointments, you can ensure the best possible outcome for your digestive health.
Low-Grade Dysplasia in Barrett’s Esophagus
Low-grade dysplasia is the early stage of precancerous changes in Barrett’s esophagus. It is characterized by mildly abnormal cell features. While low-grade dysplasia increases the risk of esophageal cancer, most people with this condition do not develop cancer. Treatment options may include regular monitoring with endoscopy exams, endoscopic resection to remove abnormal tissue, or radiofrequency ablation to destroy dysplastic cells.
If you have been diagnosed with low-grade dysplasia in Barrett’s esophagus, it is important to understand the potential risks and available treatment options. Low-grade dysplasia indicates the presence of abnormal cell changes, which can progress to a more advanced stage if left untreated. Regular monitoring with endoscopy exams allows doctors to closely observe any changes in your esophageal tissue and detect early signs of progression.
Endoscopic resection is a minimally invasive procedure that removes abnormal tissue from the esophagus. This procedure is typically performed using an endoscope, a flexible tube with a camera. It allows doctors to visualize and remove the dysplastic cells, reducing the risk of cancer development.
Radiofrequency ablation is another treatment option for low-grade dysplasia. It uses heat energy to destroy the dysplastic cells, promoting the growth of healthy tissue. Radiofrequency ablation is often performed during an endoscopy procedure and can be an effective way to eliminate precancerous cells.
It is important to discuss the available treatment options with your healthcare provider. They will carefully consider factors such as the extent of dysplasia, your overall health, and personal preferences to determine the most suitable treatment approach for you. With timely treatment and regular monitoring, many individuals with low-grade dysplasia in Barrett’s esophagus can effectively manage the condition and reduce the risk of cancer development.
| Treatment Options for Low-Grade Dysplasia in Barrett’s Esophagus |
|---|
| Regular monitoring with endoscopy exams |
| Endoscopic resection to remove abnormal tissue |
| Radiofrequency ablation to destroy dysplastic cells |
High-Grade Dysplasia in Barrett’s Esophagus
High-grade dysplasia is a more advanced stage of precancerous changes in Barrett’s esophagus. It indicates a higher risk of developing esophageal cancer. When high-grade dysplasia is detected, prompt intervention is crucial to prevent the progression of the condition.
Treatment Options
Treatment options for high-grade dysplasia in Barrett’s esophagus vary depending on the individual case and the recommendations of the healthcare professional. The primary goal of treatment is to remove or destroy the abnormal tissue to prevent the development of esophageal cancer.
1. Endoscopic Resection: Endoscopic resection involves removing the abnormal tissue using specialized tools during an endoscopy procedure. This minimally invasive approach allows for precise targeting of the dysplastic cells, reducing the need for more invasive surgeries.
2. Esophagectomy: In some cases, when the high-grade dysplasia is severe or widespread, an esophagectomy may be recommended. This surgical procedure involves removing part or all of the esophagus and reconstructing it using parts of other organs. Esophagectomies are typically reserved for more advanced cases or when other treatment options have been unsuccessful.
It’s important to note that the choice of treatment depends on the individual case and should be discussed extensively with a healthcare professional. Factors such as overall health, the extent of dysplasia, and patient preferences play a role in determining the most suitable approach.

Prevention and Follow-Up Care
After treatment for high-grade dysplasia in Barrett’s esophagus, regular follow-up care and surveillance are essential. This helps monitor the condition and detect any recurrence or new abnormalities at an early stage.
Adopting a healthy lifestyle and managing risk factors can also help prevent the progression of Barrett’s esophagus. Strategies such as quitting smoking, maintaining a healthy weight, and managing gastroesophageal reflux disease (GERD) symptoms through medication and lifestyle modifications are crucial for reducing the risk of dysplasia.
Frequently Asked Questions
- Q: Can high-grade dysplasia lead to cancer?
- A: Yes, high-grade dysplasia indicates a significant risk of developing esophageal cancer. Prompt treatment is necessary to prevent the progression of the condition.
- Q: How often should follow-up exams be scheduled after treatment for high-grade dysplasia?
- A: The frequency of follow-up exams and surveillance will depend on the individual case and the recommendations of the healthcare professional. Regular monitoring is crucial to identify any recurrent dysplasia or new abnormalities.
Other Findings in Barrett’s Esophagus
In addition to dysplasia, there can be other findings in Barrett’s esophagus, such as reactive changes and inflammation. Reactive changes are the responses of esophageal cells to irritation, while inflammation is the body’s natural defense mechanism to injury or infection. When these findings occur in Barrett’s esophagus, it is important to identify and treat the underlying cause of the irritation to prevent further complications.
Reactive changes in the esophageal tissue can occur due to factors like acid reflux or infections. These changes are characterized by alterations in the appearance and behavior of the cells. Inflammation, on the other hand, can lead to redness, swelling, and pain in the affected area.
Diagnosing these findings may involve additional tests, such as imaging studies or laboratory analysis, to determine the extent of reactive changes or inflammation. Once diagnosed, the treatment options will depend on the underlying cause and severity of the findings.
If acid reflux is the primary cause, lifestyle modifications and medications like proton pump inhibitors may be recommended. In cases of infection-related inflammation, antibiotics or antiviral medications may be prescribed. Your healthcare provider will develop a personalized treatment plan based on your specific situation.
Regular follow-up examinations and monitoring are crucial to assess the progress of treatment and identify any changes in the esophageal tissue. Your doctor will guide you through the necessary steps to manage these findings effectively and minimize the risk of complications.
Remember, early diagnosis and appropriate treatment play a vital role in optimizing your health and well-being when it comes to Barrett’s esophagus and its related findings. Consult with a healthcare professional to discuss your concerns and develop a comprehensive management plan tailored to your needs.
Screening and Prevention of Barrett’s Esophagus
Screening for Barrett’s esophagus is essential to detect the condition early on and prevent further complications. If you experience frequent symptoms of gastroesophageal reflux disease (GERD) that don’t respond to medication, it’s important to undergo screening, especially if you have additional risk factors such as a family history of Barrett’s esophagus or esophageal cancer.
Endoscopy exams are commonly used to diagnose Barrett’s esophagus. During the procedure, a thin, flexible tube with a camera is inserted through the mouth and into the esophagus, allowing the doctor to examine the lining of the esophagus for any abnormalities.
Prevention strategies play a crucial role in managing Barrett’s esophagus and reducing the risk of complications. It is important to take steps to manage GERD symptoms effectively through medication and lifestyle changes. This includes avoiding trigger foods, eating smaller meals, maintaining a healthy weight, and elevating the head of your bed when you sleep.
Regular follow-up appointments with your healthcare provider are necessary to monitor the condition and review treatment options if needed. The earlier Barrett’s esophagus is detected, the better the chances of successfully managing it and preventing it from progressing to a more advanced stage.
Conclusion
Understanding Barrett’s esophagus with dysplasia is crucial for managing the condition and protecting your digestive health. With regular monitoring, medication, and treatment options such as endoscopic resection, radiofrequency ablation, or surgery, there are ways to effectively manage Barrett’s esophagus.
Working closely with your healthcare professionals is important to determine the best course of action based on your individual circumstances. They can provide guidance and help you make informed decisions for your long-term digestive health.
Remember, early detection and prompt treatment are key in managing Barrett’s esophagus with dysplasia. By staying informed and taking proactive steps, you can take control of your health and maintain a healthy digestive system. Don’t hesitate to reach out to your healthcare team for any concerns or questions you may have.
FAQ
What is Barrett’s Esophagus with Dysplasia?
Barrett’s esophagus with dysplasia is a condition in which the tissue lining the esophagus is replaced by tissue similar to that of the intestinal lining. Dysplasia refers to abnormal cell changes in the esophagus that can increase the risk of esophageal cancer.
What are the risk factors for Barrett’s Esophagus?
Risk factors for Barrett’s esophagus include gastroesophageal reflux disease (GERD), obesity, smoking, age over 50, being male, being white, having a family history of the condition or esophageal cancer, and having excess abdominal fat.
How is Barrett’s Esophagus with Dysplasia diagnosed?
Barrett’s esophagus with dysplasia is usually diagnosed through an endoscopy procedure. During this procedure, a flexible tube with a camera is used to examine the esophagus and take tissue samples for biopsy. A pathologist then determines the degree of dysplasia present.
What is the management for Barrett’s Esophagus with Dysplasia?
The management of Barrett’s esophagus with dysplasia involves regular monitoring through endoscopy exams. Medication, such as proton pump inhibitors, may be prescribed to reduce acid reflux and protect the esophageal lining. Treatment options may also include endoscopic resection, radiofrequency ablation, or surgery to remove abnormal tissue.
What is Low-Grade Dysplasia in Barrett’s Esophagus?
Low-grade dysplasia in Barrett’s esophagus is the early stage of precancerous changes in the esophagus. It is characterized by mildly abnormal cell features. While low-grade dysplasia increases the risk of esophageal cancer, most people with this condition do not develop cancer. Treatment options may include regular monitoring, endoscopic resection, or radiofrequency ablation.
What is High-Grade Dysplasia in Barrett’s Esophagus?
High-grade dysplasia in Barrett’s esophagus is a more advanced stage of precancerous changes that indicate a higher risk of developing esophageal cancer. Treatment options for high-grade dysplasia may include endoscopic resection to remove abnormal tissue or esophagectomy, which involves removing the esophagus and reconstructing it using other organs.
What are other findings that can be present in Barrett’s Esophagus?
In addition to dysplasia, other findings in Barrett’s esophagus may include reactive changes or inflammation. These are responses by the esophageal cells to irritation. It is important to identify and treat the underlying cause of irritation, such as infections or acid reflux, to prevent further complications.
How is Barrett’s Esophagus screened and prevented?
Screening for Barrett’s esophagus is recommended for individuals with frequent GERD symptoms that don’t respond to medication, especially if they have additional risk factors. Endoscopy exams are used to detect the presence of Barrett’s esophagus. Prevention strategies include managing GERD symptoms through medication, lifestyle changes, and maintaining a healthy weight.
How is Barrett’s Esophagus with Dysplasia important for understanding and managing the condition?
Understanding Barrett’s esophagus with dysplasia is crucial for managing the condition and protecting digestive health. Regular monitoring, medication, and treatment options such as endoscopic resection, radiofrequency ablation, or surgery play a key role in the management of Barrett’s esophagus. It is important to work closely with healthcare professionals to determine the best course of action based on individual circumstances and to ensure long-term digestive health.
Source Links
- https://www.mayoclinic.org/diseases-conditions/barretts-esophagus/diagnosis-treatment/drc-20352846
- https://www.news-medical.net/health/Barretts-Esophagus-with-Dysplasia.aspx
- https://www.cancer.org/cancer/diagnosis-staging/tests/biopsy-and-cytology-tests/understanding-your-pathology-report/esophagus-pathology/barrets-esophagus.html


