If you frequently experience heartburn, regurgitation of stomach contents, or have difficulty swallowing food, it’s important to understand the signs and symptoms of Barrett’s Esophagus. This condition occurs when the lining of your esophagus becomes damaged by acid reflux, leading to changes in the cells. While these symptoms may also be associated with other digestive issues, it’s crucial to discuss any concerns with your doctor to determine the underlying cause.
Table of Contents
ToggleSome individuals with Barrett’s Esophagus may not experience noticeable symptoms of acid reflux. Therefore, it’s essential to be aware of the signs and consult with a healthcare professional if you have any digestive discomfort. Early detection and management of Barrett’s Esophagus can help prevent the progression to more serious conditions, such as esophageal cancer.
In the following sections, we will explore the causes, risk factors, complications, diagnosis, treatment options, and lifestyle changes associated with Barrett’s Esophagus. By gaining a comprehensive understanding of this condition, you can take proactive steps towards maintaining your digestive health and overall well-being.
Causes and Risk Factors of Barrett’s Esophagus
Barrett’s esophagus is a condition that occurs when the lining of the esophagus is damaged by long-standing gastroesophageal reflux disease (GERD). Despite its prevalence, the exact cause of Barrett’s esophagus is still unknown. However, several risk factors have been identified that increase the likelihood of developing this condition.
Family history: Having a family history of Barrett’s esophagus or esophageal cancer can significantly increase your risk. If any close relatives have been diagnosed with these conditions, it’s important to be more vigilant about your own digestive health.
Gender and race: Statistics show that men and individuals of Caucasian ethnicity are more prone to developing Barrett’s esophagus. This suggests that there may be genetic or environmental factors associated with these demographics that contribute to the condition.
Age: Advanced age, specifically being over the age of 50, is another risk factor for Barrett’s esophagus. As we get older, the likelihood of developing this condition increases.
Chronic heartburn and acid reflux: If you frequently experience heartburn and acid reflux, especially over a long period, the risk of developing Barrett’s esophagus is higher. Acidic stomach contents repeatedly flowing back into the esophagus can lead to cellular changes and damage to the lining.
Smoking: Both current and past smoking have been identified as risk factors for Barrett’s esophagus. Chemicals in tobacco smoke can irritate the esophagus and contribute to the development of this condition.
Weight: Being overweight or obese increases the risk of developing Barrett’s esophagus. Excess weight puts pressure on the stomach, leading to increased acid reflux and potential damage to the esophageal lining.
Helicobacter pylori (H. pylori) infection: Surprisingly, having an H. pylori infection may reduce the chances of developing Barrett’s esophagus. H. pylori is a bacterium known to cause stomach ulcers, but its presence may have a protective effect on the esophagus.
In order to understand the causes and risk factors of Barrett’s esophagus, it’s essential to assess your own health history and make any necessary lifestyle changes to mitigate these risks. By minimizing the contributing factors, you can take steps towards maintaining a healthy esophagus.
Complications of Barrett’s Esophagus
Barrett’s esophagus, a condition characterized by changes in the lining of the esophagus due to chronic acid reflux, carries a small but significant risk of developing esophageal cancer. Regular checkups and careful imaging of the esophagus are crucial in detecting any precancerous cells, known as dysplasia, and preventing the progression to esophageal cancer.
If you have been diagnosed with Barrett’s esophagus, it is imperative to be vigilant about your health and seek immediate medical help if you experience any of the following symptoms:
- Chest pain
- Difficulty swallowing
- Vomiting blood
- Passing black or tarry stools
- Unintentional weight loss
- Other concerning symptoms
Image:

| Complications of Barrett’s Esophagus | Signs and Symptoms |
|---|---|
| Esophageal Cancer | Chest pain, difficulty swallowing, unintentional weight loss |
| Stricture Formation | Difficulty swallowing, regurgitation |
| Barrett’s Ulcer | Abdominal pain, bleeding |
| Esophageal Perforation | Chest pain, difficulty swallowing, shortness of breath |
In addition to esophageal cancer, other complications associated with Barrett’s esophagus include:
- Stricture Formation: Narrowing of the esophagus makes it difficult to swallow food, leading to discomfort or pain.
- Barrett’s Ulcer: An open sore in the lining of the esophagus that can cause abdominal pain and bleeding.
- Esophageal Perforation: A rare but serious complication where a hole forms in the esophagus, causing chest pain, difficulty swallowing, and shortness of breath.
To minimize the risk of complications, it is crucial to undergo regular checkups and surveillance of your condition. Your healthcare provider will recommend the appropriate frequency of endoscopies and imaging tests to closely monitor any changes in the esophagus.
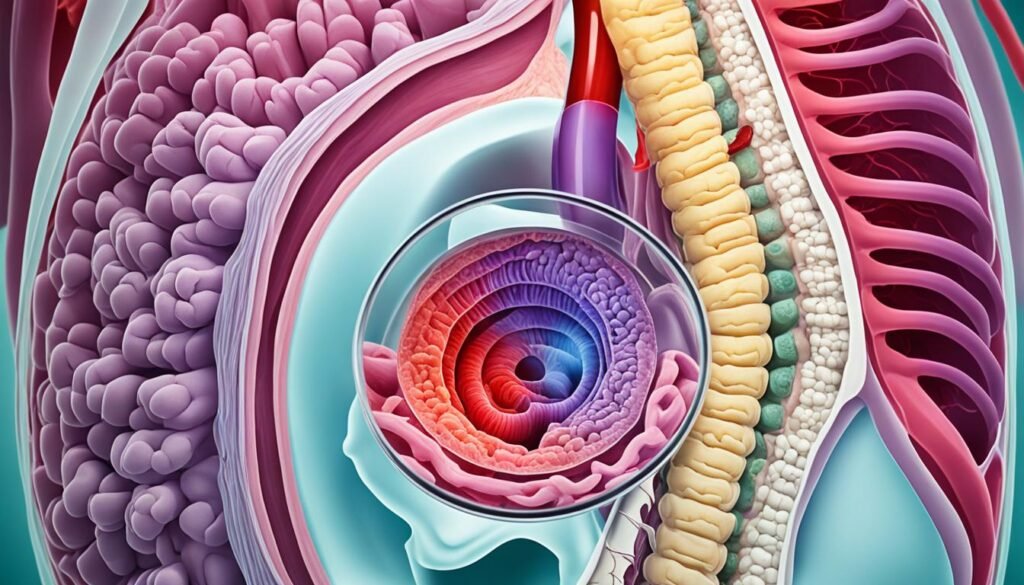
Diagnosis of Barrett’s Esophagus
Barrett’s esophagus, a condition caused by chronic acid reflux, can be diagnosed through an upper endoscopy. This procedure involves inserting a flexible tube equipped with a camera into your esophagus to visually examine the lining. During the endoscopy, a biopsy is usually performed to collect a small tissue sample for further examination under a microscope. This biopsy is crucial for confirming the presence of Barrett’s esophagus and identifying any precancerous or cancerous cells.
If you have been experiencing symptoms of acid reflux or have risk factors for Barrett’s esophagus, your doctor may recommend an upper endoscopy with biopsy. This diagnostic procedure allows for early detection and timely intervention, which can significantly improve treatment outcomes.
Regular endoscopies may be recommended for monitoring and surveillance, particularly if precancerous cells are identified. Monitoring the progression of Barrett’s esophagus is essential to ensure timely medical intervention and prevent the development of esophageal cancer.
Here is an overview of the diagnosis process for Barrett’s esophagus:
| Diagnosis Method | Procedure Description |
|---|---|
| Upper Endoscopy | Insertion of a flexible tube with a camera into the esophagus to visually inspect the lining |
| Biopsy | Collection of a small tissue sample during the endoscopy for further examination |
| Microscopic Examination | Analysis of the biopsy sample under a microscope to confirm the presence of Barrett’s esophagus and detect cancerous or precancerous cells |
Regular monitoring and follow-up through endoscopies are important to detect any changes in the esophagus and assess the risk of developing esophageal cancer. Remember to consult with your healthcare provider and follow their recommendations for checkups and surveillance.
Treatment Options for Barrett’s Esophagus
The main goal of treatment for Barrett’s esophagus is to prevent or slow the progression of the condition. There are several treatment options available to manage and address the symptoms and underlying causes of Barrett’s esophagus.
Medication
Medication can play a crucial role in reducing acid reflux symptoms and protecting the esophageal lining.
If you are experiencing acid reflux symptoms, your doctor may prescribe medication such as proton pump inhibitors (PPIs), which help reduce the amount of acid produced in the stomach. Antacids and histamine 2 blockers are also commonly used to neutralize stomach acid and provide relief from heartburn and other discomfort.
Medical Procedures
In cases where dysplasia or early signs of cancer are present, medical procedures may be necessary to remove or destroy abnormal cells in the esophagus.
Radiofrequency Ablation (RFA): This procedure involves using heat energy to destroy abnormal cells in the esophagus. A thin catheter is inserted through an endoscope and delivers radiofrequency energy, which eliminates the precancerous cells.
Endoscopic Mucosal Resection (EMR): EMR is a minimally invasive technique used to remove abnormal tissue from the esophagus. During the procedure, an endoscope with specialized tools is used to carefully remove the targeted tissue.
Endoscopic Spray Cryotherapy: This procedure involves spraying liquid nitrogen onto the abnormal tissue to freeze and destroy it. The frozen tissue is then naturally shed as part of the healing process.
Photodynamic Therapy (PDT): PDT is a treatment that uses a combination of photosensitizing drugs and laser light to destroy abnormal cells. The drugs are absorbed by the abnormal cells, which are then exposed to laser light, causing a reaction that destroys these cells.
Surgery
In severe cases, surgery may be required to remove the affected part of the esophagus.
If other treatment options are unsuccessful or the Barrett’s esophagus has progressed to a more advanced stage, your doctor may recommend surgery. The surgical procedure involves removing the damaged part of the esophagus and reconnecting the remaining healthy sections.
It’s important to discuss all available treatment options with your healthcare provider to determine the most suitable approach for your individual case.
Managing Barrett’s Esophagus
Effective management of Barrett’s Esophagus requires making lifestyle changes that can help reduce the risk of complications. By adopting healthy habits and making dietary adjustments, you can improve your quality of life and minimize the impact of acid reflux on your esophagus.
Diet plays a significant role in managing Barrett’s Esophagus. Some foods can exacerbate acid reflux symptoms, leading to discomfort and irritation. It’s important to avoid trigger foods that can worsen acid reflux, such as:
- Fatty foods
- Chocolate
- Caffeine
- Spicy foods
By eliminating or minimizing these trigger foods from your diet, you can significantly reduce acid reflux episodes and alleviate symptoms associated with Barrett’s Esophagus.
Quitting smoking and reducing alcohol consumption can also have a positive impact on managing Barrett’s Esophagus. Smoking and excessive alcohol intake can contribute to acid reflux and further damage the esophagus lining. Making a commitment to quit smoking and limiting alcohol consumption can help improve symptoms and support the healing process.
Additionally, maintaining a healthy weight through diet and exercise can reduce the pressure on your stomach and minimize the likelihood of acid reflux. Incorporate regular physical activity into your routine and focus on consuming a balanced diet that includes plenty of fruits, vegetables, whole grains, and lean proteins.
Elevate Your Sleeping Position and Opt for Smaller Meals
Simple changes to your sleeping position and eating habits can also make a difference in managing Barrett’s Esophagus. Elevating the head of your bed while sleeping can help reduce the likelihood of acid reflux during the night. You can achieve this by placing blocks under the headboard or using a wedge pillow to elevate your upper body.
Additionally, opting for smaller, more frequent meals rather than large, heavy meals can help prevent excessive stomach pressure that contributes to acid reflux. This eating pattern allows for better digestion and minimizes the chances of stomach contents flowing back into the esophagus.
Lifestyle Changes for Managing Barrett’s Esophagus
In summary, here are some key lifestyle changes to consider for managing Barrett’s Esophagus:
- Avoid trigger foods that worsen acid reflux, such as fatty foods, chocolate, caffeine, and spicy foods.
- Quit smoking and reduce alcohol consumption to improve symptoms and support healing.
- Maintain a healthy weight through a balanced diet and regular exercise.
- Elevate the head of your bed while sleeping to reduce the risk of nighttime acid reflux.
- Opt for smaller, more frequent meals to prevent excessive stomach pressure.

Implementing these lifestyle changes can have a positive impact on managing Barrett’s Esophagus and reducing the risk of complications. However, it’s essential to work closely with your healthcare provider to develop an individualized management plan that suits your specific needs and medical history.
Regular Monitoring and Follow-up
Regular monitoring and follow-up are essential for individuals with Barrett’s esophagus. To ensure the early detection of any changes or progression of the condition, periodic endoscopies are typically recommended. These endoscopies involve a thorough examination of the esophagus using a flexible tube with a camera.
The frequency of these endoscopies may vary based on factors such as the presence of dysplasia or other risk factors. Early detection of precancerous growths or cancer can significantly improve treatment outcomes and increase the chances of successful intervention.
To ensure effective surveillance and monitoring, it is vital for individuals with Barrett’s esophagus to adhere to recommended checkup schedules and follow-up appointments. By staying committed to these protocols, you can take a proactive approach to your healthcare and better manage the condition.
Regular monitoring and follow-up can provide peace of mind and help you stay informed about your health. It allows healthcare professionals to detect any changes in the esophagus promptly and initiate appropriate measures or treatment plans when necessary.

For individuals with Barrett’s esophagus, regular checkups and surveillance are crucial to ensure effective management of the condition and prevent any potential complications. By remaining diligent in your monitoring and follow-up, you can take control of your health and increase the chances of positive outcomes.
Education and Awareness
Increasing awareness and education about Barrett’s esophagus is important to promote early detection and better management of the condition. By understanding the signs and symptoms of Barrett’s esophagus, individuals can take proactive steps towards their well-being. Let’s explore some key information to enhance your understanding of Barrett’s esophagus.
Signs and Symptoms of Barrett’s Esophagus
The first step towards early detection is recognizing the signs and symptoms of Barrett’s esophagus. While frequent heartburn and difficulty swallowing food are common indicators, it’s important to remember that some individuals may experience little to no symptoms. If you have a history of acid reflux or any concerns related to your digestive health, it’s crucial to speak with your healthcare provider for a proper diagnosis.
Risks and Treatment Options
Understanding the associated risks and available treatment options is also essential. Individuals diagnosed with Barrett’s esophagus have an increased risk of developing esophageal cancer, although the risk remains relatively low. Regular checkups with your healthcare provider and careful imaging of the esophagus can help detect any precancerous cells and prevent the progression to esophageal cancer. Treatment options may include medication to reduce acid reflux symptoms or procedures like radiofrequency ablation or endoscopic mucosal resection to remove abnormal cells in the esophagus.
| Risks of Barrett’s Esophagus | Treatment Options |
|---|---|
|
|
Role of Healthcare Providers
Healthcare providers play a vital role in educating and supporting individuals with Barrett’s esophagus. They provide valuable information about the condition, its risk factors, treatment options, and regular checkup schedules. By following their guidance and maintaining open communication, you can actively participate in your healthcare journey and make informed decisions about your well-being.
Remember, early detection and management of Barrett’s esophagus can significantly improve outcomes. Stay informed, seek medical advice if needed, and prioritize regular checkups to ensure the best care for your digestive health.
Conclusion
Barrett’s esophagus is a condition that occurs due to chronic acid reflux, resulting in changes in the lining of the esophagus. Early detection of Barrett’s esophagus is crucial for preventive measures against the development of esophageal cancer. Although the risk of cancer is relatively low, regular checkups and surveillance are recommended for individuals with Barrett’s esophagus to monitor any potential progression of the condition. By staying vigilant and proactive, you can take control of your health and improve your overall well-being.
In addition to regular checkups, adopting lifestyle modifications and exploring treatment options can help manage symptoms and reduce the risk of complications associated with Barrett’s esophagus. This may include avoiding trigger foods that worsen acid reflux, quitting smoking, reducing alcohol consumption, maintaining a healthy weight through balanced diet and exercise, elevating the head of the bed while sleeping, and eating smaller, more frequent meals.
Education and awareness surrounding Barrett’s esophagus are also vital. By understanding the signs and symptoms of Barrett’s esophagus, individuals can seek medical attention promptly, leading to early detection and timely intervention. Healthcare providers play a crucial role in educating patients about the condition, ensuring they comprehend the importance of regular checkups, follow-up care, and adherence to surveillance protocols.
In conclusion, by being proactive in identifying the signs and symptoms of Barrett’s esophagus, seeking regular medical checkups, adopting healthy lifestyle modifications, and staying informed, you can better manage the condition and improve the outcomes of your health.
FAQ
What are the signs of Barrett’s Esophagus?
The most common symptoms of Barrett’s esophagus are frequent heartburn, regurgitation of stomach contents, and difficulty swallowing food. However, it’s important to note that some people with Barrett’s esophagus may have little to no symptoms of acid reflux.
What are the causes and risk factors of Barrett’s Esophagus?
The exact cause of Barrett’s esophagus is unknown, but it is often associated with long-standing gastroesophageal reflux disease (GERD). Factors that increase the risk of developing Barrett’s esophagus include a family history of the condition or esophageal cancer, being male, being white, age over 50, chronic heartburn and acid reflux, current or past smoking, and being overweight. On the other hand, having a Helicobacter pylori (H. pylori) infection may decrease the chances of developing Barrett’s esophagus.
What are the complications of Barrett’s Esophagus?
Barrett’s esophagus is associated with an increased risk of developing esophageal cancer, although the risk is relatively small. Regular checkups and careful imaging of the esophagus are important to detect any precancerous cells (dysplasia) and prevent the progression to esophageal cancer.
How is Barrett’s Esophagus diagnosed?
Barrett’s esophagus can be diagnosed through an upper endoscopy, which involves inserting a flexible tube with a camera into the esophagus to visually inspect the lining. A biopsy is usually performed during the endoscopy to collect a small tissue sample for further examination under a microscope. This biopsy helps confirm the presence of Barrett’s esophagus and allows for the detection of any precancerous or cancerous cells.
What are the treatment options for Barrett’s Esophagus?
The main goal of treatment for Barrett’s esophagus is to prevent or slow the progression of the condition. Treatment options may include medication to reduce acid reflux symptoms, such as proton pump inhibitors, antacids, or histamine 2 blockers. In cases of dysplasia or early signs of cancer, procedures like radiofrequency ablation, endoscopic mucosal resection, endoscopic spray cryotherapy, or photodynamic therapy may be performed to remove or destroy abnormal cells in the esophagus. In severe cases, surgery to remove the affected part of the esophagus may be necessary.
How can Barrett’s Esophagus be managed?
Managing Barrett’s esophagus involves making lifestyle changes to reduce the risk of complications. This includes avoiding trigger foods that can worsen acid reflux, such as fatty foods, chocolate, caffeine, and spicy foods. Quitting smoking and reducing alcohol consumption can also help improve symptoms. Additionally, maintaining a healthy weight through diet and exercise can reduce pressure on the stomach, decreasing the likelihood of acid reflux. Elevating the head of the bed while sleeping and eating smaller, more frequent meals may also be beneficial.
What is the recommended monitoring and follow-up for Barrett’s Esophagus?
Regular monitoring and follow-up are essential for individuals with Barrett’s esophagus. This typically involves periodic endoscopies to examine the esophagus for any changes or progression of the condition. The frequency of these endoscopies may vary depending on the presence of dysplasia or other risk factors. Early detection of precancerous growths or cancer can significantly improve treatment outcomes, so it’s crucial to adhere to recommended surveillance protocols.
How important is education and awareness about Barrett’s Esophagus?
Increasing awareness and education about Barrett’s esophagus is important to promote early detection and better management of the condition. Educating individuals about the signs and symptoms of Barrett’s esophagus, as well as the associated risks and treatment options, can empower them to take control of their health. Healthcare providers play a vital role in educating patients and ensuring they understand the importance of regular checkups and follow-up care.
What is the conclusion about Barrett’s Esophagus?
Barrett’s esophagus is a condition characterized by changes in the lining of the esophagus due to chronic acid reflux. Recognizing the signs and symptoms is crucial for early detection and timely intervention to prevent the progression to esophageal cancer. While the risk of cancer is relatively low, regular checkups and surveillance are recommended for individuals with Barrett’s esophagus. Lifestyle modifications and treatment options can also help manage symptoms and reduce the risk of complications. By staying informed and proactive, individuals can take control of their health and improve outcomes.
Source Links


