If you’re living with chronic digestive discomfort, unexplained weight loss, or severe abdominal pain that keeps returning, chronic pancreatitis might be the silent culprit behind your symptoms. Unlike acute episodes that come and go, chronic pancreatitis is a persistent, progressive inflammation of the pancreas, often leading to irreversible damage.
Table of Contents
ToggleIn this blog, we will talk about what chronic pancreatitis really means, how to recognize it, what causes it, and how to live better with it for the long term. Whether you’re looking for answers for yourself or someone you care about, this guide can help.
What is Chronic Pancreatitis?
Chronic pancreatitis is when the pancreas stays swollen for a long time. This swelling doesn’t go away and leads to irreversible pancreas damage. Unlike acute pancreatitis, which comes on suddenly and goes away, chronic pancreatitis is long-lasting and progressive.
Over time, this condition destroys the parts of the pancreas that make digestive juices and hormones. This makes it harder for the body to digest food and control blood sugar.
Key Differences Between Acute and Chronic Pancreatitis
| Feature | Acute Pancreatitis | Chronic Pancreatitis |
|---|---|---|
| Onset | Sudden | Gradual, worsens over time |
| Duration | Days to weeks | Long-term, often lifelong |
| Pain | Sharp, severe | Persistent or recurrent |
| Damage | Temporary | Irreversible pancreas damage |
| Cause | Gallstones, alcohol | Alcohol, genetics, other causes |
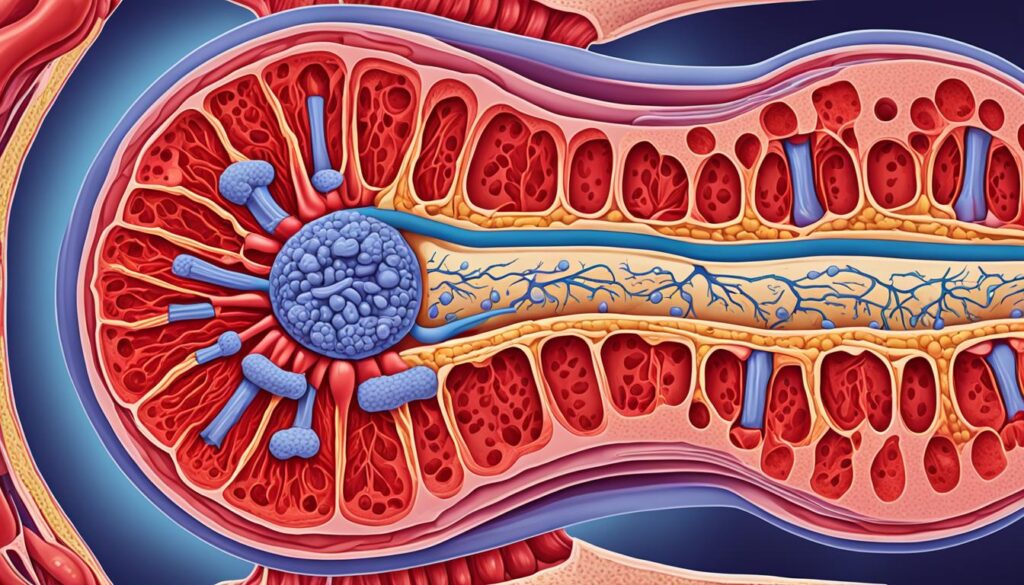
Pancreas: Functions and Importance
The pancreas does a lot for our bodies. It helps in digesting food with its enzymes and balances blood sugar with insulin. However, if it’s inflamed over time, these functions suffer.
It creates health problems when not working right. So, keeping the pancreas healthy is crucial for our well-being.
What Are the Symptoms of Chronic Pancreatitis?
Chronic pancreatitis often starts slow, with mild signs that grow worse over time. Knowing the early clues can help get treatment before serious harm happens.
At first, people may feel stomach pain that spreads to the back. Over time, the pain becomes stronger and lasts longer. Digestive problems, malabsorption and nutrient deficiency, and weight loss may show up next.
Common Symptoms to Watch For:
- Ongoing pain in the upper belly that may move to the back (chronic abdominal pain)
- Upset stomach, vomiting, and poor digestion
- Poor appetite and losing weight without trying
- Oily, floating poop (called steatorrhea)
- Pancreatic insufficiency leading to fewer digestive enzymes
- High blood sugar or diabetes as the pancreas fails
Stat: Up to 80% of people with chronic pancreatitis lose weight without trying.
How Do Symptoms Progress Over Time?
In the early stage, pain comes and goes. But later, the pain may never fully go away.
- At first, pain might only happen after meals or alcohol.
- Later, pain can become constant and severe.
- Other signs like oily stools or blood sugar changes may appear.
If pain becomes constant, it’s time to get medical help quickly.
What Are the Common Causes of Chronic Pancreatitis?
There are many causes of chronic pancreatitis. Some people get it because of lifestyle choices. Others have inherited it in their genes. Sometimes, no clear reason is found.
Main Causes Include:
- Drinking too much alcohol over time (alcohol-induced pancreatitis)
- Cigarette smoking
- Autoimmune pancreatitis
- Family history or genetic mutations (like PRSS1)
- High blood fats (triglycerides)
- Cystic fibrosis
- Blocked ducts or long-term pancreas inflammation
- Idiopathic (unknown cause in 10-30% of patients)
Stat: Alcohol use causes up to 70% of chronic pancreatitis cases in adults.
Alcohol and tobacco have a synergistic effect, meaning the combination significantly increases your risk.
Can Children Get Chronic Pancreatitis?
Yes. Kids can get it too, often due to gene mutations or inherited traits.
- Inherited forms usually show up earlier in life.
- These cases can be harder to manage due to ongoing symptoms.
- Children may face growth problems due to poor nutrition.
How is Chronic Pancreatitis Diagnosed?
Your doctor will start by asking you a lot of questions and checking you over. They’ll want to know about your health, drinking habits, and if anyone in your family has had pancreas issues. This helps them understand what might be causing your symptoms.
Blood Tests
Next, they might order some blood tests. These can show if your pancreas is inflamed or damaged. They also check how well your pancreas is working. These tests look at things like amylase, lipase, trypsinogen, and fecal fat levels.
Imaging Tests
Imaging tests are also important for finding chronic pancreatitis and seeing how bad it is. Your doctor could ask for tests like:
- X-ray: Looks for calcifications or changes in the pancreas.
- Ultrasound: Finds issues in the pancreatic ducts or calcium deposits.
- Computed Tomography (CT) scan: Gives detailed pancreas images, telling apart pancreatitis from cancer.
- Magnetic Resonance Cholangiopancreatography (MRCP): Offers detailed views of the ducts when a CT scan isn’t clear enough.
Endoscopic Procedures
Sometimes, endoscopic steps are needed for a clear diagnosis. These include procedures like:
- Endoscopic Retrograde Cholangiopancreatography (ERCP): Charts the way bile and pancreatic ducts look to find pancreatitis.
- Endoscopic Ultrasound (EUS): Gives detailed images from inside the digestive tract, helping rule out cancer.
Combining all this info helps your doctor pinpoint chronic pancreatitis. They can then plan how to best treat and manage your health.
Treatment Options for Chronic Pancreatitis
There is no cure for chronic pancreatitis, but you can manage it effectively to improve your quality of life and reduce flare-ups.
1. Lifestyle Modifications
- Stop drinking alcohol completely
- Quit smoking
- Eat a low-fat diet with small, frequent meals
- Stay hydrated
- Avoid caffeine
2. Pain Management
Chronic pain can be debilitating. Your doctor might recommend:
- Over-the-counter or prescription pain relievers
- Pregabalin or tricyclic antidepressants for nerve-related pain
- Behavioral therapy for coping with chronic pain and reducing stress.
3. Enzyme and Nutritional Support
Since your pancreas struggles to produce enzymes:
- You’ll need pancreatic enzyme replacement therapy (PERT) with every meal
- Supplement fat-soluble vitamins like A, D, E, and K
- A dietitian can help tailor your nutrition plan to prevent malnutrition
4. Diabetes Management
If chronic pancreatitis affects insulin production:
-
You may require insulin therapy to manage Type 3c diabetes (pancreatogenic diabetes)
5. Medical and Surgical Treatments
When complications arise or symptoms become unmanageable:
- Endoscopic procedures can remove stones or relieve duct obstructions
- Surgical options, such as the Puestow procedure or partial/total pancreatectomy, may be considered in severe cases

What Are the Long-Term Complications of Chronic Pancreatitis?
Over time, chronic pancreatitis can cause many serious health issues.
Possible Problems:
- High blood sugar and diabetes (Type 3c)
- Pancreatic cancer risk increases over time
- Poor digestion due to pancreatic insufficiency
- Weight loss, malabsorption and nutrient deficiency
- Constant pain that might lead to opioid use
Stat: People with chronic pancreatitis are 13x more likely to develop pancreatic cancer.
| Complication | How Often It Happens |
| Diabetes (Type 3c) | 30-50% |
| Chronic pain | 85% |
| Pancreatic cancer | 5-10% |
| Fat-soluble vitamin deficiency | 40-60% |
What Is the Recommended Diet for Chronic Pancreatitis?
Food choices play a big role in controlling chronic pancreatitis. A proper diet for chronic pancreatitis can ease symptoms and help prevent flare-ups.
What to Eat:
- Low-fat foods
- Lean proteins like chicken, tofu, and fish
- Fresh fruits and vegetables
- Whole grains
- Enzyme supplements
What to Avoid:
- Fatty or fried foods
- Alcohol
- Caffeine
- Sugary drinks
Stat: Limiting fat helps improve symptoms in up to 60% of patients.
| Foods to Eat | Foods to Avoid |
| Steamed veggies | Fried snacks |
| Boiled eggs | Sausages |
| Lentils | Creamy sauces |
| Rice, oats | Butter-rich dishes |
Do Supplements Help in Chronic Pancreatitis?
Yes, especially when digestion is poor.
- Enzymes to help break down food
- Fat-soluble vitamins (A, D, E, K)
- Vitamin B12 shots if levels drop
Supplements fill the gaps caused by poor absorption.

By following these suggestions, you can manage chronic pancreatitis better. Remember, working with your healthcare team is key. They can help you with a treatment plan that fits you.
How Can You Live Well With Chronic Pancreatitis in the Long Run?
Living with chronic pancreatitis is tough, but changes in daily habits can make life better.
- Stop drinking alcohol completely
- Quit smoking to slow pancreas damage
- Stick to a low-fat diet
- Get regular check-ups
- Join support groups for mental strength
Long-term care is about staying one step ahead of the disease.
Preventing Acute Pancreatitis Attacks
If you live with chronic pancreatitis, preventing acute attacks is key. These flare-ups are painful and can cause severe problems if not handled well. By using some important methods, you can lower the chance of getting [prevent pancreatitis attacks]:
- It’s important to not drink too much alcohol. Drinking too much is linked to both chronic and acute pancreatitis. If you already have chronic pancreatitis, stopping alcohol is necessary to avoid a worsening condition.
- Stopping smoking is crucial. It makes things worse for those with chronic pancreatitis and raises the chance of getting pancreatic cancer. Kicking the habit is vital for your health if you aim to [prevent pancreatitis attacks].
- Eat foods that are low in fat. High-fat, fried, and greasy foods can stress your digestive system and lead to problems. Choosing a diet that’s low in fat but high in lean proteins, fruits, and vegetables is smart.
- Think about taking extra enzymes. These can help your body break down food better and absorb nutrients more effectively. This can take some pressure off your pancreas, lowering the risk for [prevent pancreatitis attacks].
- If you need to manage pain, there are options. Medicines like acetaminophen or ibuprofen are good for mild to moderate pain in chronic pancreatitis. For really bad or constant pain, see a pain management doctor. They may suggest procedures like celiac plexus blocks to address the issue.
Using these strategies with the support of your healthcare team can help you avoid acute pancreatitis attacks. Early care and a holistic health approach are critical. Proactively managing your condition is essential for a good quality of life. For further tips on how to [prevent pancreatitis attacks], check out this useful resource.
When to Seek Medical Attention
If you have chronic pancreatitis, seeking instant medical help is vital if you feel severe abdominal pain that won’t go away. This pain might signal an acute pancreatitis attack. These attacks need fast treatment to avoid dangerous issues. If you’re unsure about when to see a doctor for pancreatitis, talk to your doctor right away.
Acute pancreatitis is very serious and can lead to life-threatening situations. Knowing when to see a doctor for pancreatitis is key. Look out for these warning signs:
- Sudden, severe abdominal pain that doesn’t improve with at-home remedies
- Nausea and vomiting that persists or worsens
- Fever, chills, or signs of infection
- Difficulty keeping down food or liquids
- Yellowing of the skin or eyes (jaundice)
If you have any of these symptoms, get medical help as soon as possible. Early treatment can prevent major problems and limit the effects of chronic pancreatitis. It’s important to know when to see a doctor for pancreatitis.
Genetic Factors in Chronic Pancreatitis
Your chronic pancreatitis might come from your family’s genes. Some gene changes make you more likely to get it. Knowing how genetics play a part helps in figuring out why it happens. It also helps in choosing the best type of treatment for you.
A mutation in the PRSS1 gene can lead to hereditary chronic pancreatitis (HCP). This is a rare type of the disease. These changes in the PRSS1 gene cause problems in the pancreas early. They make the body start digesting itself, which hurts the pancreas.
HCP seems to be quite common if you have PRSS1 mutations, affecting about 80% of those who inherit it. But, some people with these mutations might have very mild or no symptoms at all. These issues usually start showing up when you’re still a kid, earlier than when alcohol causes pancreatitis.
There are other genes that might also raise the risk of chronic pancreatitis. Differences in the SPINK1/PSTI and CFTR genes can lead to problems as well. Some combinations of these gene differences are more often seen in those with pancreatitis.
Genes that affect the CTRC enzyme could also play a part in getting chronic pancreatitis. And, changes in a gene for a calcium sensor could be a new clue. Researchers are always studying more about the genes behind this disease. So, doctors can do a better job in treating and caring for those with chronic pancreatitis.
When to Reach Out for Help: Book a Consultation with Dr. Nivedita Pandey
If you or a loved one is dealing with chronic pancreatitis, don’t wait. The damage is permanent, but your quality of life doesn’t have to be.
Dr. Nivedita Pandey, MBBS, Diplomate, American Board (Internal Med & Gastroenterology), is a U.S.-trained, board-certified Senior Gastroenterologist. She treats pancreas-related digestive problems, alcohol-induced pancreatitis, autoimmune pancreatitis, and helps manage chronic abdominal pain and more.
As one of South Delhi’s few female gastroenterologists, Dr. Pandey creates a safe, respectful space for women to talk about gut and hormone health. She specializes in fatty liver, NASH, viral hepatitis, cirrhosis, and pancreatic enzyme replacement therapy.
Book your appointment today for personalised pancreatitis treatment from expert gastroenterologist Dr. Nivedita Pandey. Don’t wait for symptoms to get worse, get answers now.
FAQ
What is chronic pancreatitis?
Chronic pancreatitis is pancreatic inflammation that keeps coming back. It causes ongoing harm. This problem starts as acute pancreatitis, a sudden illness, but then doesn’t go away.
What are the symptoms of chronic pancreatitis?
Abdominal pain is the main sign of chronic pancreatitis. At first, you might feel bloated or lose your appetite. You might also experience pain after meals and lose weight without trying.
Later, you could notice your stools look fatty or oily or feel dizzy. These are more serious signs.
What causes chronic pancreatitis?
Alcohol abuse and gallstones are the top reasons for this illness.
How is chronic pancreatitis diagnosed?
Doctors will check your medical history and do a physical exam. They’ll want to know about your symptoms, how much you drink, and your family’s health history. This helps them decide if you have chronic pancreatitis.
What are the treatment options for chronic pancreatitis?
Doctors aim to lessen your pain and manage other symptoms. They may give you enzymes, help control your blood sugar, and find and treat what caused the disease.
What are the potential complications of chronic pancreatitis?
Chronic pancreatitis can cause health problems like trouble digesting food and diabetes. It may also lead to more pain and, in some cases, pancreatic cancer.
What lifestyle changes are recommended for those with chronic pancreatitis?
Doctors might suggest you change your diet, stop drinking alcohol and smoking, and keep a healthy weight. These steps can improve your quality of life.
How can I cope with the challenges of living with chronic pancreatitis?
Getting help from your healthcare team, talking to a counselor, and joining a support group can make a big difference. They can help with your physical and emotional health.
How can I prevent acute pancreatitis attacks if I have chronic pancreatitis?
To avoid sudden pain from pancreatitis, lay off the alcohol, eat healthy, and quickly get help if your stomach starts hurting a lot.
Are there any genetic factors associated with chronic pancreatitis?
Yes, sometimes, genes play a role in causing chronic pancreatitis. Certain genetic mutations can raise your illness risk.
What new treatments and research are being explored for chronic pancreatitis?
Scientists are working on better ways to handle chronic pancreatitis. They’re looking into new drugs, treatments, and surgeries to help those with this disease.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin





