Stages of liver disease describe how liver damage develops over time, from mild swelling to severe failure. Damage often starts quietly. You may feel normal while harm builds inside. Early stages allow healing if you act fast. Late stages limit options and raise death risk.
Table of Contents
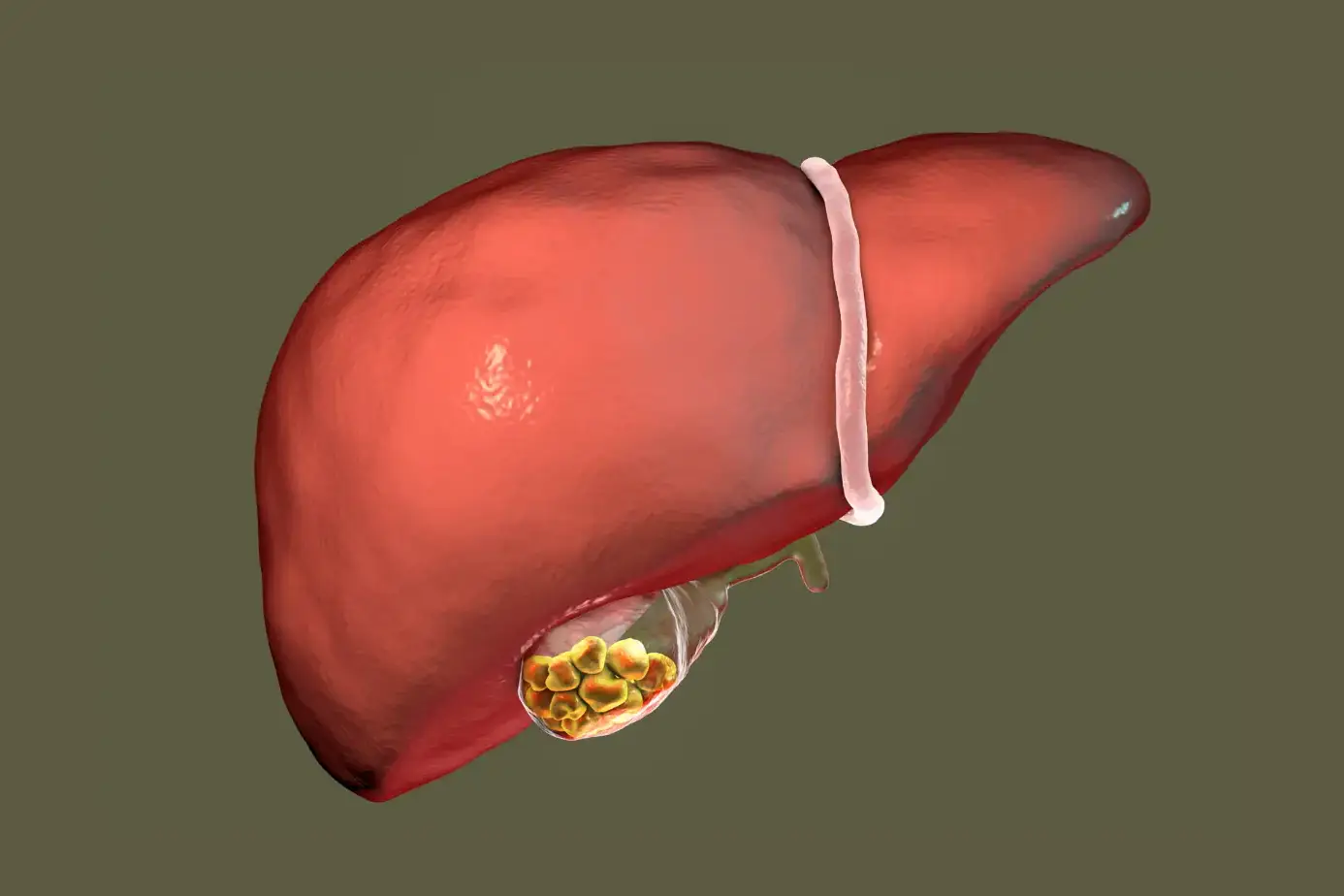
ToggleThe liver filters toxins, controls blood sugar, and supports digestion. When injury repeats, liver cells swell, scar, and fail. Alcohol, viral infections, excess fat, and immune attacks drive most cases. The stages of liver disease follow a predictable path, but the speed differs by cause and lifestyle.
5 Stages of Liver Disease
Doctors group liver damage into clear levels. These levels show how much healthy tissue remains and how well blood flows through the liver. Understanding the 5 stages of liver disease helps you know what can improve and what cannot.
Stage 1: Inflammation
This stage starts the injury process. Liver cells swell after repeated stress. Alcohol, hepatitis viruses, fatty buildup, and some drugs often trigger this response. At this point, liver structure stays mostly normal.
You may feel tired or notice mild pain on the upper right side of your belly. Many people feel nothing. Blood tests often show raised liver enzymes. Enzymes rise when liver cells leak their contents into blood. Inflammation is one of the stages of liver disease that can be fully reversed if you remove the cause.
Key facts you should know:
- Inflammation does not equal permanent damage.
- Enzyme levels can return to normal within weeks.
- Continued exposure pushes damage forward.
Stage 2: Fibrosis (Scarring)
Fibrosis begins when inflammation does not stop. The body lays down scar tissue to heal repeated injury. Scar tissue blocks blood flow between liver cells. Healthy cells receive less oxygen and nutrients.
You may notice weakness, poor appetite, or bloating. Symptoms stay mild because healthy tissue still works. Special scans can detect stiffness caused by scars. Fibrosis marks a serious shift in the stages of liver disease because scarring can spread even when symptoms stay quiet.
Important points:
- Fibrosis can improve if caught early.
- Ongoing injury makes scars thicker.
- Blood tests alone may miss this stage.
Stage 3: Cirrhosis
Cirrhosis means widespread scarring. Normal liver shape changes. Blood struggles to pass through. Pressure rises in nearby veins. Toxins build up in the body.
You may see yellow skin, itchy arms, swollen legs, and easy bruising. Confusion may appear due to toxin buildup in the brain. Cirrhosis represents advanced stages of liver disease . Scars do not reverse, but treatment can slow the decline.
Clinical insights:
- Cirrhosis increases infection risk.
- Minor injuries may cause heavy bleeding.
- Nutrition support becomes critical.
Stage 4: End-Stage Liver Disease (ESLD)
ESLD means the liver can no longer meet body’s needs. Detox fails. Protein production drops. Hormone balance breaks down.
You may experience severe swelling, confusion, vomiting blood, or kidney failure. Life expectancy falls without advanced care. ESLD sits among the most dangerous stages of liver disease and often leads to transplant evaluation.
Key clinical features:
- Fluid fills the belly due to low protein.
- Brain function worsens from toxin buildup.
- Infections turn life-threatening.
Stage 5: Liver Cancer
Long-term damage raises cancer risk. Most liver cancers develop on top of cirrhosis. Tumors block blood flow and destroy remaining tissue.
Symptoms include weight loss, deep belly pain, fever, and worsening jaundice. Treatment depends on tumor size, spread, and liver reserve. This final step completes the 5 stages of liver disease and carries the highest death risk.
Liver Disease Stages and Symptoms
Symptoms change as damage deepens. Some signs appear early. Others show only when harm becomes severe. Understanding liver disease stages and symptoms helps you act before options shrink.
Symptoms in Early Liver Disease
Early damage often stays quiet. You may dismiss signs as stress or aging. Common early symptoms include:
- Low energy
- Mild nausea
- Reduced appetite
- Light discomfort under the ribs
Blood tests often catch early damage before symptoms worsen. Early liver disease stages and symptoms respond best to lifestyle change and medical care.
Symptoms in Moderate Liver Damage
As scarring grows, signs become harder to ignore. You may notice:
- Daily fatigue
- Belly bloating after meals
- Swollen ankles
- Dark urine
These symptoms reflect poor blood flow and bile movement. Doctors often diagnose fibrosis or early cirrhosis during this phase. Recognizing moderate liver disease stages and symptoms can still slow progression.
Symptoms in Advanced Liver Disease
Advanced damage affects many organs. Severe symptoms include:
- Yellow eyes and skin
- Large belly swelling
- Mental confusion
- Nose or gum bleeding
These signs indicate failure of detox and clotting systems. Advanced liver disease stages and symptoms require urgent specialist care.
Silent Symptoms and Asymptomatic Stages
Some people feel fine until late disease. Fat-related liver damage often stays silent for years. Normal energy does not equal a healthy liver. Routine tests catch silent injury before it enters dangerous stages of liver disease .
Silent damage facts:
- Enzymes may stay near normal.
- Imaging may show fat or stiffness.
- Delay raises cancer risk later.
Liver Disease Stages Diagnosis
The diagnosis of liver disease stages relies on patterns. Doctors combine blood markers, imaging, and stiffness testing to estimate scarring and function. Accurate staging prevents both overtreatment and delayed care.
Blood Tests for Liver Damage
Blood tests measure enzymes, proteins, and clotting factors. High ALT and AST levels signal liver cell injury, not how severe scarring is. Low albumin and poor clotting suggest advanced damage.
Platelet counts drop when scarring blocks blood flow through the liver. These patterns help outline early versus advanced stages of liver disease , but blood work alone cannot confirm fibrosis or cirrhosis.
Doctors often repeat blood tests over months. Trends matter more than one result. Stable numbers suggest controlled disease. Rising abnormalities signal progression across liver disease stages and symptoms even if you feel fine.
Imaging Tests (Ultrasound, CT, MRI)
Imaging shows liver shape, texture, and blood flow. Ultrasound detects fat buildup, nodules, and fluid in the belly. CT and MRI reveal tumors, blocked veins, and internal bleeding. Imaging identifies complications linked to late stages of liver disease , such as enlarged spleen or portal hypertension (high pressure in liver veins).
Scans also guide cancer screening in cirrhosis. Imaging does not replace lab tests. It adds structural detail needed for accurate diagnosis of liver disease stages .
Liver Fibrosis and Elastography Tests
Elastography measures liver stiffness using sound waves. Stiffer tissue means more scarring. This test helps detect fibrosis before symptoms appear. It reduces the need for biopsy in many cases.
Doctors use elastography to track changes over time. Falling stiffness suggests healing. Rising stiffness warns of progression through stages of liver disease even when blood tests appear stable.
Liver Biopsy
A biopsy removes a tiny tissue sample. It shows inflammation, fat, scarring, and cancer cells under a microscope. Doctors use biopsy when tests conflict or when treatment choices depend on exact staging.
Biopsy carries small risks, so it is not routine. When used, it gives the clearest picture of diagnosis of liver disease stages , especially in mixed or unclear cases.
Liver Disease Stages Treatment
Treatment for liver disease stages focuses on stopping injury first, then managing damage already done. Early treatment supports liver cell repair. Advanced stages require complication control and transplant planning rather than cure attempts.
Treatment in Early Stages
Early inflammation responds well to cause removal. You stop alcohol. You treat viral infections. You reduce liver fat through weight control. Liver cells regenerate fast when stress ends.
Doctors may monitor without medication. Enzymes often normalize within weeks. Early treatment for liver disease stages can fully restore function when action is timely.
Medical Management of Fibrosis
Fibrosis needs tighter control. Doctors manage blood sugar, cholesterol, and blood pressure. Medications reduce inflammation and insulin resistance. Some patients need antiviral or immune-modifying drugs.
Lifestyle control remains essential. Fibrosis can improve if scarring stays mild. Medical treatment for liver disease stages aims to slow or halt scar expansion.
Managing Cirrhosis and Complications
Cirrhosis care focuses on stability. Doctors treat fluid buildup with diet changes and medications. They prevent bleeding using endoscopy and drugs. Infections require fast antibiotics.
Nutrition plays a major role. Protein intake must balance muscle loss and brain symptoms. Cirrhosis care represents complex treatment for liver disease stages that requires specialist follow-up.
Liver Transplant for Advanced Disease
A transplant replaces the damaged liver with a healthy one. It is considered when survival drops despite care. ESLD and certain cancers qualify.
Patients undergo strict screening. After transplant, lifelong medication prevents rejection. Transplant remains the final option in treatment for liver disease stages when recovery is no longer possible.
Prevention of Liver Disease Stages
Prevention liver disease stages strategies work even after damage begins. Removing alcohol, managing weight, and controlling metabolic disease slows or halts progression. Prevention reduces cancer risk and improves long-term survival.
Lifestyle Changes to Slow Progression
Regular movement reduces liver fat and inflammation. Even modest weight loss improves enzyme levels. Sleep helps hormone balance that protects liver cells. These steps slow progression across stages of liver disease regardless of cause.
Diet and Alcohol Avoidance
Alcohol directly poisons liver cells. No safe level exists once damage starts. Diet should focus on whole foods, fiber, and lean protein. Excess sugar feeds fat buildup in the liver. Diet control forms a core pillar of preventing liver disease stages .
Managing Underlying Conditions
Diabetes, high cholesterol, and viral hepatitis accelerate damage. Tight control slows scarring. Vaccination prevents viral infections that destroy liver tissue.
Managing root causes strengthens the prevention of liver disease stages more than supplements or detox products.
Regular Monitoring and Follow-Up
Routine tests catch silent worsening. Imaging screens for cancer early. Follow-up allows treatment adjustment before symptoms explode.
Monitoring is often the difference between stability and rapid decline in stages of liver disease .
Risk Factors That Accelerate Liver Disease Progression
Alcohol misuse, viral infection, fat buildup, and immune disorders cause continuous liver cell stress.
Alcohol Use Disorder
Alcohol inflames liver cells and blocks regeneration. Continued use pushes inflammation to cirrhosis fast. Abstinence remains the strongest predictor of survival.
Viral Hepatitis
Untreated hepatitis causes constant immune attack. Over time, this leads to fibrosis, cirrhosis, and cancer. Early treatment changes long-term outcomes.
Fatty Liver Disease
Excess fat disrupts liver metabolism. Inflammation follows. Obesity and insulin resistance worsen progression through the stages of liver disease .
Metabolic and Autoimmune Disorders
Immune attacks and genetic metabolic errors injure liver tissue. Early diagnosis limits scarring and complications.
When to See a Doctor
Medical review becomes urgent when symptoms reflect impaired detox or bleeding control. Delayed care allows silent progression through late stages of liver disease , where treatment options narrow quickly.
Warning Signs of Advanced Liver Disease
Yellow skin, swollen belly, confusion, and frequent bleeding require immediate evaluation. These signs reflect dangerous stages of liver disease .
Emergency Symptoms
Vomiting blood, black stools, severe confusion, or collapse signal life-threatening failure. Emergency care saves lives in late stages of liver disease .
FAQs
Can Liver Disease Be Reversed in Early Stages?
Yes. Inflammation and mild fibrosis can heal if the cause stops. Early stages of liver disease respond well to alcohol avoidance, weight control, and proper medical care.
How Fast Does Liver Disease Progress?
Progression varies widely. Alcohol misuse and obesity speed damage. Some people move through stages of liver disease within years, while others remain stable for decades.
Is Cirrhosis Always Fatal?
No. Many people live years with proper care. Cirrhosis marks advanced stages of liver disease , but monitoring and treatment can prevent fatal complications.
Can Liver Disease Exist Without Symptoms?
Yes. Many patients feel normal until late damage. Silent progression makes routine testing essential across all stages of liver disease .
What Stage of Liver Disease Needs Transplant?
Transplant is considered in ESLD or certain cancers when survival without surgery drops. These represent the final stages of liver disease .
When Is a Liver Biopsy Required?
Doctors use biopsy when noninvasive tests conflict or when precise staging guides treatment decisions across complex stages of liver disease .
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin