Liver lesions are areas of liver tissue that appear different from surrounding tissue during imaging. Most liver lesions are benign and never become cancer. They are often found accidentally during scans done for unrelated problems. Their significance depends on origin, structure, and liver health, not simply size. When clinicians evaluate liver lesions , they focus on imaging pattern, risk background, and biological cause before considering intervention.
Table of Contents
ToggleKey Takeaways
- Liver lesions are structural differences in liver tissue seen on scans
- Most liver lesions are non-cancerous and symptom-free
- They are commonly detected during routine imaging
- The causes of liver lesions determine the risk level
- Monitoring alone is often enough instead of active care
What Are Liver Lesions?
Liver lesions describe localized changes in liver structure visible through imaging technologies such as ultrasound, CT, or MRI. The term “lesion” does not define disease type. It signals altered tissue density, blood flow pattern, or composition. That alteration may reflect fluid, fat, blood vessels, scar tissue, or cellular growth.
A frequent misunderstanding equates liver lesions with cancer. That assumption is inaccurate. Radiologists routinely identify liver lesions during scans for kidney stones, trauma, or digestive complaints, and most require no action.
From a biological standpoint, the liver’s regenerative capacity contributes to lesion formation. Hepatocytes, which are liver cells responsible for metabolism and detoxification, replicate efficiently after injury. This regenerative behavior sometimes creates nodular growth patterns that appear as liver lesions but carry minimal clinical concern.
When liver lesions are found, interpretation focuses on imaging signature, patient age, metabolic status, and infection exposure rather than immediate alarm.
What Causes Liver Lesions?
The causes of liver lesions relate to how liver tissue changes. These changes come from growth, infection, fat buildup, blood vessel structure, or long-term stress.
- Some liver lesions develop from small groups of liver cells growing more than usual. This growth stays limited and harmless. Hormones or healing processes may influence this change.
- Infections also belong to the liver lesions . Bacteria or parasites may create localized inflammation or pus-filled areas. These appear as visible spots during imaging tests and need medical evaluation.
- The liver contains dense blood circulation. Minor changes in vessel arrangement create detectable differences. This mechanism contributes to the causes of liver Pain in many healthy people.
- Uneven fat accumulation inside liver cells changes the scan appearance. This effect appears in metabolic conditions and is counted among the causes of liver lesions .
- Chronic stress from alcohol use, viral infection, or metabolic illness alters the structure and forms additional liver lesions .
Cancer spread is another possibility within the causes of liver lesions . Cells from tumors in other organs may travel through the bloodstream and settle in the liver. This occurs less often but must be ruled out when evaluating findings.
Doctors focus on origin rather than size. Large benign findings may remain harmless. Small ones may require attention depending on the cause.
What Are The Types Of Liver Lesions?
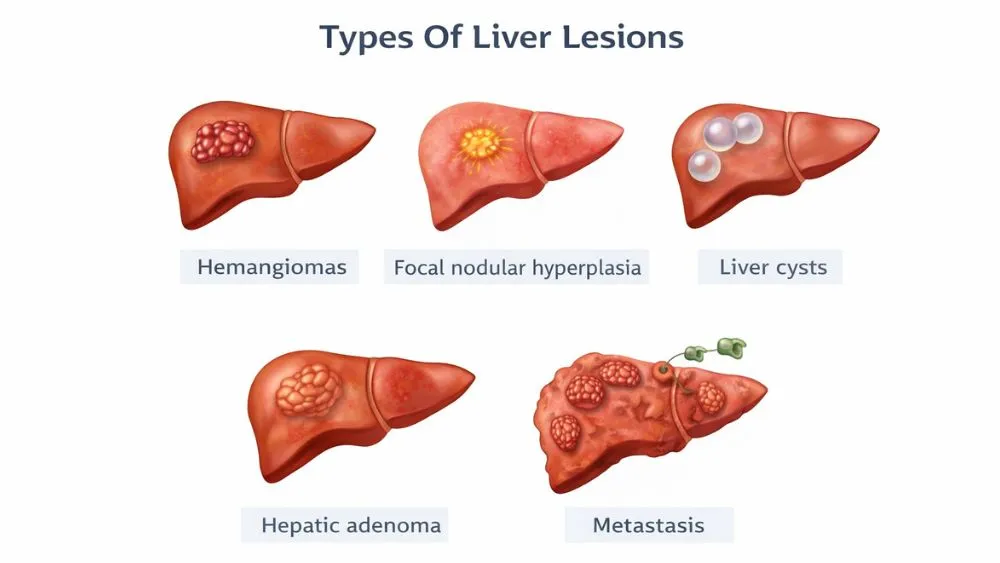
Medical classification organizes types of liver lesions according to cellular behavior. This approach separates benign from malignant categories, allowing clinicians to align monitoring intensity and intervention decisions with biological risk.
Benign Liver Lesions (Most Common)
Most types of liver lesions belong here and do not create health problems.
- Hemangiomas form from clusters of small blood vessels. They usually remain stable for life. You never know you have them.
- Focal nodular hyperplasia results from localized cell growth linked to blood flow differences. Imaging identifies it clearly, and treatment rarely becomes necessary. These types of liver lesions generally remain symptom-free.
- Liver cysts contain fluid enclosed in a thin wall. They often appear during scans without causing issues. These liver lesions usually stay unchanged and require no action.
- Hepatic adenomas relate to hormone exposure or metabolic factors. Compared with other benign types of liver lesions , doctors monitor them more closely because complications may occur in rare cases.
Overall, benign types of liver lesions rarely need treatment unless symptoms or structural changes develop.
Malignant Liver Lesions
Some types of liver lesions involve cancerous growth. These require a structured medical evaluation.
Primary malignant growth starts in liver cells. Long-term tissue stress increases the chance of such development. Secondary malignant growth occurs when cancer spreads from another organ. These liver lesions show different scan patterns that alert specialists to investigate further.
Symptoms Of Liver Lesions
Most liver lesions do not cause any physical signs. The liver can keep working normally even when small structural changes exist. Because of this, you live with liver lesions without noticing anything unusual. Symptoms usually appear only when the lesion grows, bleeds, or develops along with another liver problem.
The symptoms of liver lesions usually start when pressure builds in the upper abdomen or when nearby organs get compressed. Larger lesions can stretch the outer covering of the liver, which contains pain-sensitive nerves. Inflammation can also affect energy levels and appetite.
Typical symptoms of liver lesions include discomfort on the upper right side of the abdomen, bloating after eating, nausea, and ongoing tiredness. These symptoms of liver lesions also appear in many digestive disorders, so they cannot confirm diagnosis alone. Imaging tests remain necessary to identify cause and severity.
What Are The Risk Factors For Liver Lesions?
Long-term liver stress stands among the strongest risk factors for liver lesions . Chronic viral infections, regular heavy alcohol intake, or fatty liver conditions alter tissue structure over time. This environment encourages visible changes during imaging.
Hormonal exposure represents another group within the risk factors for liver lesions , especially prolonged estrogen-based medication use linked to adenoma formation.
Cancer history also matters because circulating abnormal cells may settle in the liver. Metabolic conditions such as obesity and diabetes expand risk factors for liver lesions by affecting fat storage and inflammation patterns.
How Are Liver Lesions Diagnosed?
Diagnosis aims to identify the nature of liver lesions rather than simply confirming their presence. Doctors combine imaging findings, blood testing, and personal health information.
Imaging Tests
Ultrasound commonly detects liver lesions first because it quickly shows tissue differences. CT scans provide more detail and track blood flow through the lesion. MRI offers the clearest information and often defines composition, helping distinguish fat, fluid, or cellular growth.
Radiologists study contrast patterns instead of size alone. For many liver lesions , imaging gives enough detail to guide care decisions without additional testing.
Blood Tests
Blood tests evaluate liver performance and screen for markers linked to disease activity. Abnormal enzyme levels indicate stress but do not specify lesion type. Doctors interpret results alongside imaging when assessing liver lesions .
These tests also check protein production and clotting ability. Stable results often support a benign interpretation. Normal findings frequently occur with harmless liver lesions , reinforcing that multiple data points guide diagnosis.
When Is A Biopsy Needed?
Biopsy becomes necessary only when scans cannot clearly define the lesion. A small tissue sample allows microscopic inspection of cell arrangement and structure. This helps classify uncertain liver lesions .
Modern imaging reduces the need for biopsy in most cases. Doctors weigh benefits against bleeding risk before recommending it. Only a minority of liver lesions require this step.
Treatments For Liver Lesions
Management depends on behavior, not detection alone. Many liver lesions remain stable and never need intervention. Care plans focus on protecting liver function while addressing potential risks.
When No Treatment Is Needed
Observation is the most common path among treatments for liver lesions . Doctors schedule follow-up scans to confirm stability. This prevents unnecessary procedures while ensuring safety.
Monitoring intervals vary based on lesion category and health history. If repeated imaging shows no change, active care often stops. This conservative strategy reflects how frequently treatments for liver lesions involve surveillance rather than action.
Medical Or Surgical Treatment
Intervention becomes appropriate when lesions grow, cause symptoms, or show a risk. Physicians assess structure, health status, and progression before selecting options within treatments for liver lesions .
Procedures may include removal, blood flow control, or infection management. Medication changes sometimes address hormone or metabolic influences. Exact drug choices depend on individual condition. Personalized planning defines modern treatments for liver lesions .
Treatment For Cancerous Lesions
Cancer-related liver lesions require specialist supervision. Care teams coordinate imaging review, surgical evaluation, and systemic therapy planning. Treatment direction reflects tumor spread and overall liver condition.
Early referral supports balanced decision-making between tumor control and organ preservation. Structured care pathways guide advanced treatments for liver lesions with malignant features.
Are Liver Lesions Dangerous?
No. Most liver lesions do not pose danger. Imaging surveys consistently show benign findings dominate detection rates. Risk depends on lesion behavior, growth speed, and overall liver health rather than presence alone.
Danger increases when patterns show irregular structure, rapid enlargement, or association with chronic disease. Doctors assess background health and scan results together. Careful interpretation transforms uncertain liver lesions into clear clinical categories.
Diet and Detox
FAQs – Liver Lesions
Are liver lesions cancerous?
No. Most liver lesions detected during imaging represent benign vascular clusters, cysts, or fat-related changes. Cancer risk rises in liver mainly when chronic hepatitis, cirrhosis, or prior malignancy exists.
Do liver lesions always need treatment?
No. Many liver lesions only require periodic imaging every six to twelve months to confirm stability. Active intervention usually begins when measurable growth, bleeding risk, or functional disruption appears.
Can liver lesions disappear on their own?
Yes. Certain liver lesions related to fat redistribution or hormonal influence may shrink after metabolic control or medication adjustment, sometimes becoming undetectable on later imaging scans.
Are liver lesions common?
Yes. Imaging surveys show incidental liver lesions appear in a notable share of adults undergoing abdominal scans, particularly after age 40, when vascular and metabolic variation increases.
Can fatty liver cause liver lesions?
Yes. Uneven fat storage alters imaging signals and ranks among established causes of liver lesions , especially in insulin resistance or obesity-linked metabolic disruption.
Is a biopsy always required?
No. Advanced MRI characterization identifies most types of liver lesions accurately. Biopsy typically occurs only when imaging cannot exclude malignancy confidently.
Do liver Pain cause symptoms early?
No. Early symptoms of liver Pain rarely occur because liver reserve capacity masks functional change until lesions enlarge or inflammation develops.
Should I worry if one is found accidentally?
No. Incidental liver lesions are usually benign. Concern increases only when imaging reveals aggressive vascular behavior or high-risk clinical background factors.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.