End-stage liver disease symptoms start when your liver stops doing many basic functions. The liver cleans blood, helps digestion, and controls fluid balance. When damage becomes severe, toxins stay in your body, and swelling begins. You may notice tiredness, weight loss, or mental changes.
Table of Contents
ToggleKey Takeaways
- End-stage liver disease symptoms include fatigue, swelling, yellow skin, and confusion
- Severe scarring blocks liver function
- Causes include long-term injury or infection
- Some warning signs need urgent care
- Treatment focuses on support or transplant
What Is End Stage Liver Disease?
End-stage liver disease means the liver has heavy scarring. Doctors call this cirrhosis. Scar tissue replaces healthy cells. At this stage, end-stage liver disease symptoms appear because the liver cannot perform normal tasks.
Your liver removes waste, stores energy, and helps blood clot. When function drops, waste builds up and fluids shift. This leads to many end-stage liver disease symptoms you notice in daily life.
Early liver disease may show few problems. Doctors call this the compensated stage. The body still manages basic work. End stage means decompensated stage. The body cannot manage anymore. Clear end-stage liver disease symptoms appear.
Damage rarely reverses now. Scar tissue cannot turn back into healthy tissue. Blood flow through the liver becomes blocked. Pressure rises inside veins. That pressure causes swelling and bleeding risk. These changes explain lasting end-stage liver disease symptoms .
End-Stage Liver Disease Causes
Fat buildup in the liver may cause inflammation. Inflammation means swelling inside cells. Over time, scarring forms. This pathway appears often among end-stage liver disease causes .
Long-term alcohol use damages liver cells directly. Repeated injury prevents repair. Scar tissue spreads. This is a major contributor to end-stage liver disease causes .
Chronic viral infections such as hepatitis also harms liver tissue. Ongoing inflammation destroys cells slowly. Continuous injury becomes one of the known causes of end-stage liver disease .
Autoimmune problems occur when the immune system attacks the liver. Genetic conditions may affect iron or protein handling. Both lead to repeated injury cycles. Years of damage explain why end-stage liver disease symptoms develop.
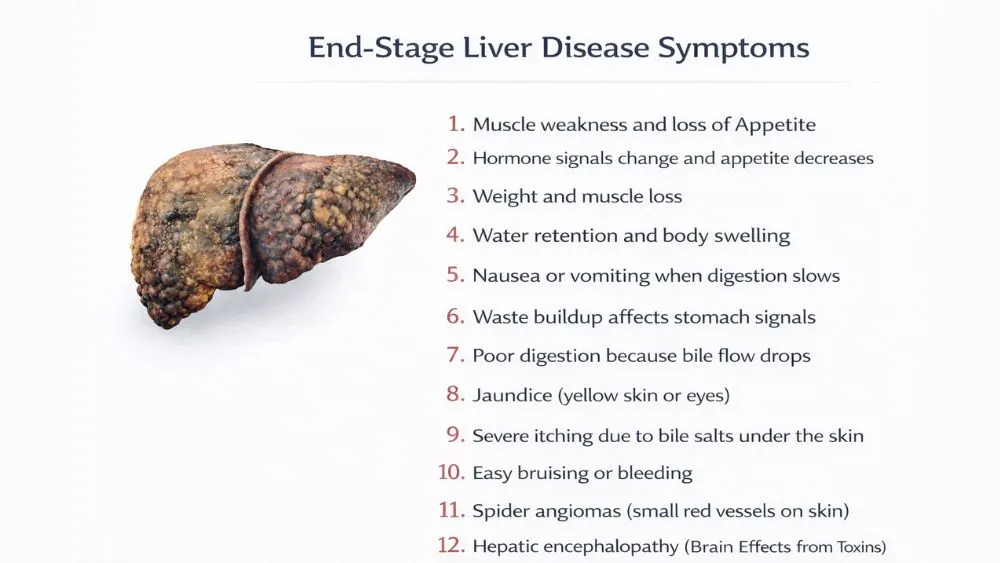
End Stage Liver Disease Symptoms
Doctors group end-stage liver disease symptoms by body area. This helps identify patterns. These end-stage liver disease symptoms vary between people but follow common clusters.
General & Systemic Symptoms
You often feel strong tiredness. Rest does not fix it. The body cannot store or release energy properly. This is one of the early end-stage liver disease symptoms .
Muscle weakness follows. The body breaks down muscle for fuel. Movement becomes harder.
Loss of appetite occurs. Hormone signals change. You eat less. This worsens nutrition. These changes increase end-stage liver disease symptoms .
Weight and muscle loss may happen together. The body uses stored tissue to stay active. This signals deep metabolic strain.
Digestive & Abdominal Symptoms
Ascites means fluid buildup in the abdomen. The belly enlarges due to pressure changes. Salt and water retention worsen swelling. This visible issue ranks among end-stage liver disease symptoms .
Abdominal discomfort appears due to stretching. Sitting or bending may feel harder. Nausea or vomiting develops when digestion slows. Waste buildup affects stomach signals.
Poor digestion occurs because bile flow drops. Bile helps break down fat. Nutrient use declines. This adds to overall end-stage liver disease symptoms impact.
Skin & Appearance Changes
Jaundice means yellow skin or eyes. It happens when bilirubin builds up. Bilirubin is a waste pigment. This change marks advanced end-stage liver disease symptoms .
Severe itching happens due to bile salts under the skin. Nerve irritation causes constant urge to scratch.
Bruising or bleeding occurs easily. The liver cannot produce enough clotting proteins. Minor injury leaves marks.
Spider angiomas are small red vessel patterns on skin. Hormone imbalance affects vessels. These visible features reflect systemic end-stage liver disease symptoms .
Brain & Nervous System Symptoms
Confusion appears when toxins affect brain cells. Memory or focus drops. This serious sign counts among end-stage liver disease symptoms .
Personality changes may develop. You may feel irritable or withdrawn. Brain chemistry shifts. Sleep pattern reversal can occur. You stay awake at night and sleep during day.
Hepatic encephalopathy means brain effects caused by toxins. Early signs include slower thinking. Later stages include disorientation.
Signs of End-Stage Liver Disease That Indicate Medical Emergency
Some signs of end-stage liver disease mean you need urgent medical care. These problems show sudden loss of body control. Quick treatment reduces serious harm.
Vomiting blood may occur when swollen veins in the food pipe burst. Black or bloody stool also points to internal bleeding. Both are dangerous signs of end-stage liver disease that require hospital care.
Severe confusion or unconsciousness happens when toxins affect brain function. Breathing problems may occur due to fluid or infection. Sudden kidney failure may reduce urine output sharply. Knowing these signs of end-stage liver disease helps you seek care without delay.
How Is End Stage Liver Disease Diagnosed?
Doctors assess liver function using tests and physical checks. Evaluation focuses on how well the liver works and on the end-stage liver disease symptoms you report. This combined approach guides treatment decisions.
Blood tests measure waste levels, clotting ability, and kidney markers. Results may change because hydration, infection, or medicine alters values. Imaging scans show shape changes or fluid buildup. These findings support discussion of end-stage liver disease life expectancy .
The MELD score uses lab values to estimate disease severity. A higher number means weaker liver function. This score helps place patients on transplant waiting lists. Doctors use this information when planning the life expectancy outlook for end-stage liver disease.
No single scan confirms the stage. Doctors combine symptom history, labs, and exam findings. Ongoing monitoring ensures updated evaluation. This process improves accuracy when discussing end-stage liver disease over time.
End Stage Liver Disease Life Expectancy
End-stage liver disease life expectancy differs greatly between people. Survival length depends on cause, complications, and care access. Doctors avoid fixed predictions because health status changes often.
Complications such as infection, bleeding, or kidney problems shorten survival. Control of these conditions improves stability. These factors strongly affect end-stage liver disease life expectancy .
Transplant access changes outcomes significantly. A successful transplant restores function and extends survival. Without transplant, treatment aims to reduce complications. This distinction shapes end-stage liver disease life expectancy discussions.
End-Stage Liver Disease Death Timeline
There is no fixed end-stage liver disease death timeline . Progression varies. Stable periods may occur before sudden decline.
Complications such as infection or bleeding often trigger rapid worsening. Medical support can stabilize or extend survival. These variables affect interpretation of end-stage liver disease death timeline .
Supportive care focuses on comfort and symptom control. Nutritional support and medication reduce distress. Doctors track mental state, kidney output, and breathing patterns. These signs guide realistic expectations.
Treatment Options For End Stage Liver Disease
Treatment manages complications linked to end-stage liver disease symptoms . Care plans change based on your condition. Doctors target fluid buildup, toxin control, and nutrition support.
Procedures remove abdominal fluid to reduce pressure. Medicines lower toxin levels to improve thinking. Other drugs relieve itching or nausea. These measures address daily end-stage liver disease symptoms .
Nutrition support helps maintain strength. Doctors guide calorie intake and monitor protein balance. Medication doses vary by patient needs. Adjustments depend on lab results and response to end-stage liver disease symptoms .
Liver transplant replaces damaged tissue with a donor organ. Eligibility requires careful screening. When successful, transplant reduces many end-stage liver disease symptoms , though long-term monitoring remains necessary.
FAQs – End-Stage Liver Disease Symptoms
Is end-stage liver disease fatal?
Yes. Without transplant or complication control, end-stage liver disease symptoms progress to organ failure. Bleeding, infection, or brain dysfunction often lead to death if untreated.
Are symptoms always severe?
No. Early end-stage liver disease symptoms may involve fatigue or appetite loss. Severe swelling, confusion, and bleeding appear later when liver function drops further.
Can end-stage liver disease be reversed?
No. Scar tissue cannot heal back to normal. end-stage liver disease symptoms remain. Transplant is the only method that restores liver function.
Does everyone with ESLD need a transplant?
No. Some people stabilize with monitoring and treatment of signs of end-stage liver disease, such as fluid buildup or confusion, though transplant becomes necessary if complications increase.
Is confusion a early signs of liver damage?
Yes. Toxin buildup affects brain activity and counts among early signs of liver damage . Memory loss and disorientation require medical review.
Can life expectancy improve with treatment?
Yes. Infection control, fluid management, and nutrition support improve end-stage liver disease life expectancy by reducing complications and hospital admissions.
Is pain common in end stage liver disease?
No. Pain usually comes from swelling or infection. Monitoring end-stage liver disease symptoms helps doctors identify causes and adjust treatment.
Should family members be involved in care planning?
Yes. Families help observe end-stage liver disease death timeline changes and support medication schedules, improving response to urgent symptoms.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.