Diffuse hepatic steatosis refers to widespread fat accumulation across the liver rather than isolated patches. This fat buildup interferes with how your liver controls blood sugar, processes fats, and clears toxins from the body.
Table of Contents
ToggleUnlike sudden liver illnesses, this condition develops slowly and often remains silent while metabolic damage continues. It commonly links to insulin resistance, excess calorie intake, hormonal imbalance, and long-term dietary patterns rather than a single trigger.
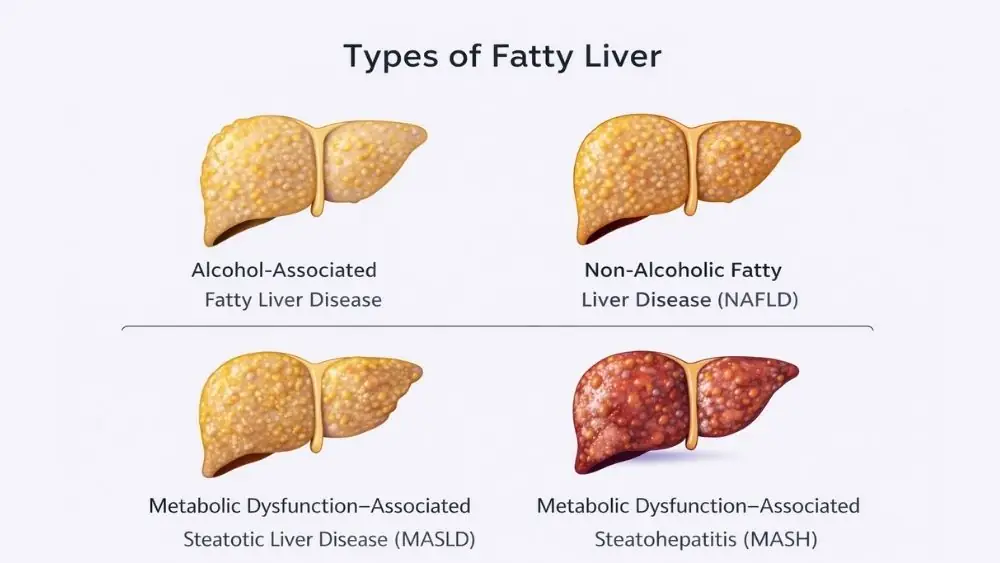
Types Of Fatty Liver Disease
Fatty liver disorders differ based on what drives fat buildup and whether liver cells show damage. Some forms involve only fat storage, while others include inflammation and scarring, which raises long-term risk. Correct classification affects monitoring and treatment decisions.
Alcohol-Associated Fatty Liver Disease
Alcohol-associated fatty liver develops when alcohol changes how your liver handles fat. Alcohol increases fat production inside liver cells and slows fat breakdown. Even before pain or abnormal blood tests appear, diffuse hepatic steatosis can already be present. The liver often improves within weeks after alcohol intake stops. Continued drinking increases the chance of inflammation and scarring.
Non-Alcoholic Fatty Liver Disease (NAFLD)
This form appears without heavy alcohol use. It is common in people with obesity, diabetes, or high cholesterol. NAFLD often starts silently. Imaging may reveal diffuse hepatic steatosis even when liver enzymes stay normal. This explains why many people remain unaware of liver fat for years.
Metabolic Dysfunction–Associated Steatotic Liver Disease (MASLD)
MASLD is a newer term that highlights metabolic stress as the main driver. Blood sugar problems, abnormal cholesterol, and belly fat work together. In MASLD, diffuse hepatic steatosis reflects ongoing metabolic strain rather than a single cause.
Metabolic Dysfunction–Associated Steatohepatitis (MASH)
MASH develops when fat triggers liver cell injury and inflammation. This stage is more serious. Scar tissue may begin to form. Diffuse hepatic steatosis combined with inflammation increases the risk of long-term liver damage.
What Causes Hepatic Steatosis
Fat accumulates in the liver when fat delivery or production exceeds the liver’s ability to burn or export it. Metabolic stress, dietary sugars, alcohol metabolism, and hormonal imbalance often interact rather than act alone. These factors explain why hepatic steatosis appears even in people without obvious symptoms.
Insulin Resistance and Metabolic Syndrome
Insulin resistance prevents sugar from entering muscle cells. The liver then converts extra sugar into fat. This fat stays trapped in liver tissue. Over time, insulin resistance sustains diffuse hepatic steatosis even without excess calories.
Obesity and Central Fat Accumulation
Fat around your waist releases fatty acids directly into the liver. This direct flow overwhelms normal fat processing. People with normal body weight but high belly fat can still develop diffuse hepatic steatosis .
Excess Alcohol Consumption
Alcohol alters liver chemistry. It promotes fat storage while blocking fat removal. Regular intake, even at moderate levels, can maintain diffuse hepatic steatosis and delay recovery.
Poor Diet and High Fructose Intake
Sugary drinks and processed foods supply fructose. The liver converts fructose into fat faster than other sugars. This process feeds diffuse hepatic steatosis , especially when fiber intake stays low.
Medications and Toxin Exposure
Certain drugs stress liver metabolism. Long-term exposure may trigger fat accumulation. This mechanism explains why diffuse hepatic steatosis sometimes appears in people without obesity or alcohol use.
Genetic and Hormonal Factors
Some genes affect fat handling and insulin sensitivity. Thyroid disorders and hormonal changes also influence liver fat storage. Genetics can make diffuse hepatic steatosis harder to reverse.
Symptoms Of Hepatic Steatosis
Liver fat rarely causes sharp or sudden symptoms because the liver lacks pain nerves. Subtle signs usually reflect reduced energy handling or liver enlargement rather than direct injury. Symptoms often appear only after fat disrupts normal liver function.
Early-Stage Symptoms
Early stages often lack clear warning signs. Routine blood tests or imaging often reveal diffuse hepatic steatosis before symptoms begin.
Fatigue and Low Energy
Fatty liver interferes with energy balance. You may feel tired despite normal sleep. This fatigue often improves once liver fat decreases.
Right Upper Abdominal Discomfort
A mild pressure or ache under your right ribs may appear. This discomfort reflects liver swelling linked to diffuse hepatic steatosis .
Liver Enlargement (Hepatomegaly)
Fat accumulation can enlarge the liver. Doctors may detect this during a physical exam or imaging.
Symptoms of Advanced Liver Involvement
As damage progresses, symptoms become clearer. Swelling, yellowing of skin, and easy bruising may appear. These signs suggest diffuse hepatic steatosis has advanced beyond simple fat storage.
How Is Hepatic Steatosis Diagnosed
Diagnosis relies on detecting fat content, not just liver injury. Imaging reveals fat distribution, while blood tests assess metabolic strain and inflammation risk. Combining methods gives a clearer picture than relying on a single test.
Blood Tests and Liver Enzymes
ALT and AST may rise, but normal results do not rule out fat buildup. Many people with diffuse hepatic steatosis show normal enzyme levels.
Ultrasound Findings
Ultrasound often shows a brighter liver compared to the kidney. This brightness reflects fat within liver tissue and commonly detects diffuse hepatic steatosis .
CT Scan and MRI Imaging
CT and MRI measure liver fat more precisely. MRI can estimate fat percentage, which helps track improvement or progression of diffuse hepatic steatosis .
FibroScan and Elastography
These tools measure liver stiffness. Increased stiffness suggests scar tissue. FibroScan helps separate simple fat buildup from early fibrosis.
Liver Biopsy: When It Is Needed
Biopsy is not routine. Doctors reserve it for unclear cases or suspected advanced disease. It confirms inflammation and scarring when imaging cannot.
Hepatic Steatosis Treatment
Treatment focuses on correcting the processes that drive fat storage rather than targeting fat alone. Reducing insulin resistance, limiting fat input, and restoring fat export are key goals. Medical therapy supports lifestyle change but does not replace it.
Weight Loss and Lifestyle Modification
Sustained weight loss directly reduces liver fat content. Losing even 5 percent of body weight lowers fat inside liver cells, while greater loss can reduce inflammation. Rapid weight loss is not advised, as it may stress the liver. Consistent habits improve insulin sensitivity, which helps reverse diffuse hepatic steatosis over time.
Dietary Changes for Fatty Liver
Your liver responds quickly to food quality. Diets low in added sugars and refined carbohydrates reduce fat production in the liver. Fiber slows sugar absorption and supports gut health, which affects liver inflammation. These changes form a core part of treatment for hepatic steatosis and support long-term control.
Physical Activity and Exercise
Exercise improves how your muscles use sugar and fat. This reduces fat delivery to the liver. Both aerobic activity and resistance training lower liver fat even without major weight loss. Regular movement helps stabilize diffuse hepatic steatosis and improves blood lipid levels.
Alcohol Cessation
Alcohol directly worsens liver fat accumulation. Complete avoidance allows liver cells to recover and restore normal fat handling. Continued alcohol intake, even in small amounts, can delay improvement in diffuse hepatic steatosis .
Management of Diabetes and Dyslipidemia
High blood sugar and abnormal cholesterol accelerate liver fat buildup. Doctors usually adjust medications to improve metabolic control. Better glucose and lipid control lowers cardiovascular risk, which is closely linked to diffuse hepatic steatosis .
Medications and Emerging Therapies
No medication cures fatty liver for all patients. Some diabetes drugs reduce liver fat and inflammation. Vitamin-based therapies show mixed results. New agents target insulin resistance and inflammation, but evidence remains limited and evolving.
Complications of Untreated Diffuse Hepatic Steatosis
Liver cells can clear fat when metabolic pressure eases. Reversal depends on how long fat has been present and whether inflammation or scarring has started. Early stages respond far better than advanced disease.
Progression to Steatohepatitis
Fat can irritate liver cells, triggering inflammation. This stage involves cell injury, not just fat storage. Persistent inflammation increases the chance of scarring and worsens liver function.
Liver Fibrosis
Fibrosis means scar tissue replaces healthy liver cells. Blood flow through the liver becomes restricted. Fibrosis develops slowly but may become permanent if diffuse hepatic steatosis remains untreated.
Cirrhosis Risk
Cirrhosis represents extensive scarring and structural damage. The liver struggles to perform essential tasks like toxin removal and protein production. This stage increases the risk of liver failure and cancer.
Cardiovascular Disease Risk
People with fatty liver face higher heart attack and stroke risk. Abnormal cholesterol, insulin resistance, and inflammation link diffuse hepatic steatosis to heart disease more strongly than liver failure.
Can Diffuse Hepatic Steatosis Be Reversed?
Liver cells can clear fat when metabolic pressure eases. Reversal depends on how long fat has been present and whether inflammation or scarring has started. Early stages respond far better than advanced disease.
Reversibility in Early Stages
When fat accumulation occurs without inflammation or scarring, liver cells can clear excess fat. Lifestyle correction often restores normal liver structure and function within months.
Timeline for Liver Fat Reduction
Liver fat levels can decrease within weeks of dietary change and exercise. Blood tests may normalize within three to six months. Imaging improvements often follow continued lifestyle adherence.
Factors Affecting Recovery
Age, genetics, metabolic control, and alcohol use influence recovery speed. Persistent insulin resistance or continued sugar intake can slow improvement in diffuse hepatic steatosis .
Prevention of Diffuse Hepatic Steatosis
Preventing liver fat requires long-term control of sugar handling and fat storage rather than short dietary fixes. Daily habits influence liver metabolism more than occasional detox efforts. Small, consistent changes reduce lifetime risk.
Healthy Weight Maintenance
Avoiding gradual weight gain prevents fat from reaching the liver. Waist size offers a better risk indicator than body weight alone.
Balanced Diet and Sugar Control
Limiting sugary beverages and processed foods lowers liver fat production. Whole foods support steady energy use and reduce insulin spikes linked to diffuse hepatic steatosis .
Limiting Alcohol Intake
Alcohol limits the liver’s ability to burn fat. Keeping intake minimal or avoiding alcohol altogether protects liver health.
Regular Health Screening
Routine blood tests and imaging identify fatty liver before symptoms appear. Early detection allows intervention before complications develop.
When to See a Doctor
Medical evaluation is needed when liver fat appears repeatedly or metabolic markers worsen. Delay allows silent progression that may not cause pain until damage becomes advanced.
Persistently Elevated Liver Enzymes
Repeated abnormal liver tests need assessment, even without symptoms. Enzyme trends offer clues about liver stress.
Imaging Showing Diffuse Fatty Liver
Imaging findings require follow-up to assess fibrosis risk. Monitoring helps guide diagnoses of hepatic steatosis and management plans.
Symptoms Suggesting Liver Damage
Swelling, jaundice, confusion, or bleeding tendencies suggest advanced liver involvement and need urgent care.
FAQs
Is diffuse hepatic steatosis serious?
Diffuse hepatic steatosis can remain mild for years, but it becomes serious when inflammation or scarring develops. Early detection and lifestyle correction greatly reduce the risk of long-term liver damage.
Can diffuse fatty liver turn into cirrhosis?
Yes, prolonged diffuse hepatic steatosis can progress to inflammation and fibrosis, which may eventually lead to cirrhosis if underlying metabolic or alcohol-related factors remain uncontrolled.
Is hepatic steatosis always related to alcohol?
No. Many cases occur without alcohol use. Metabolic dysfunction, obesity, and insulin resistance explain most non-alcohol-related causes of hepatic steatosis .
How long does it take to reverse fatty liver?
Improvement often begins within weeks of lifestyle change. Complete reversal of diffuse hepatic steatosis may take several months depending on weight loss, diet, and metabolic control.
How is diffuse hepatic steatosis diagnosed?
Doctors rely on imaging, blood tests, and sometimes elastography. These diagnoses of hepatic steatosis help determine severity and risk of progression.
Which blood tests are abnormal in hepatic steatosis?
ALT, AST, triglycerides, and fasting glucose may rise. However, normal results do not exclude diffuse hepatic steatosis , especially in early stages.
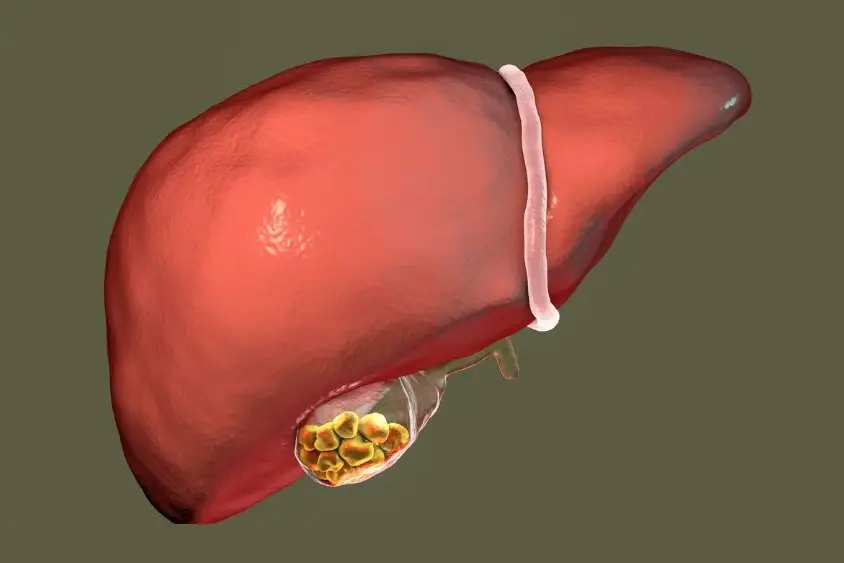
What does fatty liver look like on ultrasound or CT scan?
The liver appears brighter or less dense than surrounding tissues. This visual change reflects fat infiltration seen in types of fatty liver disease .
Is FibroScan useful in diffuse hepatic steatosis?
Yes. FibroScan estimates liver stiffness and fat content. It helps distinguish simple fat buildup from early fibrosis in diffuse hepatic steatosis .
Can diffuse hepatic steatosis progress to steatohepatitis?
Yes. Without control of metabolic risk factors, diffuse hepatic steatosis can advance to inflammatory stages, increasing the risk of fibrosis and cirrhosis.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.