Alcohol and liver damage signs show up when your liver can’t handle the workload anymore. Your liver processes about 90% of every drop of alcohol you consume.
Table of Contents
ToggleKey Takeaways
- Alcohol and liver damage signs develop when repeated drinking injures liver cells and disrupts normal function
- Early signs include fatigue, loss of appetite, nausea, and mild abdominal discomfort
- Advanced damage causes jaundice, swelling, bleeding problems, and confusion
- Some early changes reverse when drinking stops
You may ignore the early warnings, like feeling tired, losing your appetite, and a dull ache below your ribs. By the time symptoms become impossible to ignore, real damage has already happened.
Your liver keeps working even when 70% of it is damaged. This silence tricks you into thinking everything’s fine. It’s not.
How Alcohol Damages the Liver
Your liver breaks down alcohol into acetaldehyde (a toxic chemical that attacks your cells directly). Acetaldehyde damages DNA and stops cells from repairing themselves properly.
Acetaldehyde triggers inflammation. Your body sends white blood cells to fix the problem. These cells release chemicals that hurt healthy tissue while trying to clean up the damage. The more you drink, the more inflammation builds up, leading to chronic inflammation.
Fat accumulation starts next. Alcohol messes with how your liver processes fats. Instead of burning fat for energy, your liver stores it. Cells swell with fat droplets. Blood flow slows down. Oxygen delivery drops.
Every time you drink alcohol, scar tissue forms where healthy cells used to be. Scars don’t filter toxins or produce proteins; they just sit there, blocking blood flow and reducing function.
Your liver regenerates constantly, replacing old cells with new ones. But regeneration requires time without new damage. Keep drinking, and your liver can’t keep pace with destruction. Alcohol and liver damage signs appear when compensation fails.
The amount of alcohol matters, but so does the pattern. Binge drinking (five or more drinks in one session) causes more damage than spreading drinks across a week. Daily drinking, even moderate amounts, prevents healing.
| Women develop liver damage faster than men at lower alcohol levels. Two drinks per day for a woman equals three or four for a man in terms of liver stress. |
Early Signs of Liver Damage From Alcohol
Signs of liver damage from alcohol start when you feel tired more often.
- Appetite drops without an obvious reason. Foods you loved taste bland or unappealing.
- Morning nausea becomes common. You wake up queasy, especially after drinking the night before. Some people vomit occasionally.
A dull ache appears in your right upper abdomen, below your ribs. It’s not sharp or stabbing; just a persistent discomfort. The pain comes and goes. After heavy drinking, it worsens. When you stop drinking for a few days, it fades.
- Weight loss happens without trying.
- Blood tests catch problems before you feel sick. Normal AST is below 40 units per liter. Alcoholic liver damage pushes it above 50, sometimes above 100.
These early signs of liver damage from alcohol get ignored because everyone feels tired sometimes, and lots of things cause nausea. That abdominal ache could be anything. You wait until symptoms become severe before seeing a doctor. By then, significant damage exists.
Your liver has massive reserve capacity. You can lose 70% of function before severe symptoms appear. This reserve lets early damage hide. Your liver struggles silently, compensating as much as possible, until compensation fails completely.
Symptoms of Alcohol-Induced Liver Damage
Symptoms of alcohol induced liver damage intensify as destruction progresses.
- Jaundice turns your skin and eyes yellow. The yellowing starts in your eyes, then spreads to your skin. Bilirubin levels above 2.5 mg/dL cause visible yellowing.
- Your skin itches intensely. Not surface itching from dry skin; the itch comes from inside your tissues. Some people scratch until they bleed.
- Bruises appear from minor bumps. A slight knock against a table leaves a purple mark that takes weeks to fade.
- Small red spots with radiating blood vessels appear on your chest, face, and arms.
- Your abdomen swells with fluid. This condition is called ascites (ah-SITE-eez). Your stomach looks pregnant. Breathing becomes difficult.
- Mental fog sets in. You forget conversations. Simple tasks feel overwhelming. Concentration disappears.
- Sleep patterns flip. You’re awake at night, exhausted during the day.
Alcohol Liver Damage Abdominal Pain
Alcohol liver damage abdominal pain is in your right upper abdomen, just below your ribs on the right side. Your liver has no pain nerves inside it. The pain comes from the capsule surrounding your liver (a thin membrane that stretches when your liver swells).
The pain feels dull and constant, like a deep ache. It’s different from sharp gallstone pain or burning stomach ulcer pain. Pressing on the area increases discomfort. The pain doesn’t move around or radiate to other spots.
Inflammation causes swelling. The capsule stretches, triggering pain receptors in the membrane.
Alcohol liver damage abdominal pain worsens after drinking . Alcohol causes immediate inflammation, increasing swelling temporarily. Heavy drinking sessions cause more pain than light drinking. The pain might fade after a few days of abstinence, then return with more drinking.
Stages of Alcohol-Related Liver Disease
Stages of alcohol related liver disease progress through three phases, each representing deeper damage. The transition between stages depends on how much you drink, how long you’ve been drinking, and genetic factors that vary person to person.
Alcoholic Fatty Liver
Fat fills liver cells like grease clogging a drain. Your liver looks enlarged and yellowish instead of dark reddish-brown. This happens in about 90% of people who drink heavily for just a few weeks. Most people feel nothing wrong. Blood tests show mildly elevated enzymes; maybe AST at 60 or ALT at 80 when normal is below 40.
Imaging tests like ultrasounds reveal bright spots where fat has accumulated. This stage is completely reversed. Stop drinking for four to six weeks, and the fat disappears. Your liver cells shrink back to normal size. Function restores fully. But start drinking again, and fat reaccumulates within days.
Alcoholic Hepatitis
Inflammation attacks liver cells directly. Hepatitis means liver inflammation (your liver is under assault). Liver cells die faster than they can regenerate. Alcohol and liver damage signs become noticeable here.
Blood work shows dramatic enzyme elevations. AST might hit 200 or 300. Bilirubin rises above 3 mg/dL. White blood cell counts jump. You feel sick; fatigue intensifies, nausea worsens, pain sharpens. Some people develop fever. Jaundice appears in moderate to severe cases.
Alcoholic Cirrhosis
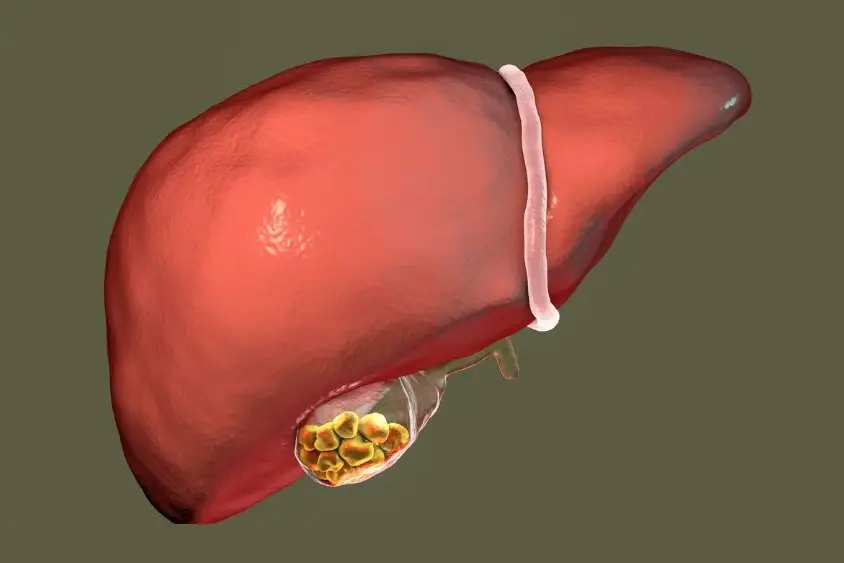
Scar tissue replaces healthy liver tissue permanently. Your liver shrinks, hardens, and develops a nodular, bumpy surface instead of being smooth.
Cirrhosis doesn’t reverse. Scars are permanent. You can stop drinking and prevent new scars from forming, but existing scars stay forever. About 10-20% of heavy drinkers develop cirrhosis after 10-20 years of sustained drinking.
Complications multiply fast. Swollen, fragile veins in your esophagus and stomach, causing massive internal bleeding. Vomiting blood or passing black, tarry stools means a variceal bleed.
Liver cancer risk jumps. Cirrhotic livers develop hepatocellular carcinoma at rates 15 times higher than healthy livers. Survival drops sharply. Five-year survival with compensated cirrhosis (still functioning somewhat) is about 50%. With decompensated cirrhosis (failing), survival drops below 30%. Continued drinking cuts survival to under 20% at five years.
Reversible Signs of Alcohol Liver Damage
Reversible signs of alcohol liver damage include fatty liver changes, elevated liver enzymes, fatigue, appetite loss, and mild abdominal discomfort. If you catch damage in the fatty liver stage, complete healing happens within weeks.
Enzyme levels drop toward normal after abstinence. AST and ALT decline within two to four weeks. GGT, which rises with alcohol use, takes six to eight weeks to normalize.
Fat disappears from liver cells. Imaging studies show this clearly. Cell membranes repair. DNA damage gets fixed. Inflammation resolves as white blood cells stop attacking tissue.
Energy returns gradually. The first week feels rough; fatigue persists, sometimes worsens as your body adjusts. By week three or four, energy improves noticeably. Appetite comes back. Food tastes good again. The dull abdominal ache fades.
Signs That Indicate Severe or Advanced Damage
Persistent jaundice that lasts weeks signals liver failure. If your skin and eyes stay yellow despite stopping alcohol, your liver isn’t recovering. Bilirubin levels above 5 mg/dL indicate serious dysfunction. Above 10 mg/dL means impending failure.
- Vomiting blood (bright red or coffee-ground texture) means ruptured veins in your esophagus. This is life-threatening.
- Black, tarry stools indicate bleeding somewhere in your digestive tract. This also requires immediate medical attention.
- Confusion, drowsiness, slurred speech, or personality changes suggest hepatic encephalopathy. Without treatment, this progresses to stupor, then coma. Mortality reaches 40-50% once coma develops.
- Rapid abdominal swelling over days means massive ascites. Your belly might expand several inches, and breathing becomes labored. You may accumulate 10-15 liters of fluid.
- Kidney failure follows severe liver failure. Urine output drops. Waste products accumulate. This combination (liver and kidney failure) has extremely poor survival rates.
Can Alcohol-Related Liver Damage Be Reversed?
Early fatty liver reverses completely. Stop drinking, and fat clears out within four to eight weeks. Full function returns.
Alcoholic hepatitis partially reverses. You might lose 20-30% of capacity permanently, but 70% functioning liver is enough for normal life.
Cirrhosis doesn’t reverse. Scar tissue is permanent. The damage is structural. Alcohol and liver damage signs might improve but scars remain. Your liver will never be 100% again.
Stopping alcohol at any stage prevents further damage. That’s the critical point. Even with cirrhosis, abstinence extends survival significantly. Five-year survival with cirrhosis and continued drinking: 20-30%. With abstinence: 50-60%. That’s years of additional life.
When to See a Doctor
See a doctor if you’ve been drinking heavily for years and notice persistent fatigue, loss of appetite, nausea, or abdominal discomfort lasting more than two weeks. These symptoms deserve evaluation even if they seem minor.
Get checked immediately if jaundice appears. Yellow skin or eyes never happens for harmless reasons.
Abdominal swelling needs medical attention within days. Even small amounts of ascites suggest advanced disease. Your doctor can drain fluid to ease breathing and investigate causes. Diuretics help prevent reaccumulation.
Any bleeding requires emergency care. Vomiting blood, bloody stools, or excessive bruising from minor bumps can kill within hours without treatment.
Confusion, memory problems, or difficulty concentrating warrant urgent assessment. Treatment includes lactulose to reduce ammonia and antibiotics to alter gut bacteria. Early intervention prevents coma.
Annual checkups with blood work catch problems before symptoms appear. Liver enzyme tests (AST, ALT, GGT, and bilirubin) reveal damage early. If you drink regularly, get tested yearly. Elevated enzymes trigger further investigation with ultrasound or FibroScan to assess scarring.
FAQs – Alcohol and Liver Damage Signs
What are the first signs of liver damage from alcohol?
Fatigue that doesn’t improve with rest, loss of appetite, mild nausea, and occasional dull pain below your right ribs are the earliest alcohol and liver damage . These symptoms appear subtle and get mistaken for other problems, which delays diagnosis until damage worsens significantly.
Does alcohol always cause liver pain?
No. Early fatty liver produces no pain at all. Pain appears only when your liver swells enough to stretch the surrounding capsule. You may develop advanced alcohol and liver damage signs, including cirrhosis, without ever experiencing pain, making early detection harder.
Can alcohol-related liver damage be reversed?
Fatty liver reverses completely within weeks of stopping alcohol. Alcoholic hepatitis partially reverses over months. Cirrhosis never reverses because scar tissue is permanent, but abstinence prevents further scarring and extends survival by 20-30 years compared to continued drinking.
Is jaundice an early sign of alcohol liver damage?
No. Jaundice appears after moderate to severe damage has occurred. Early alcohol and liver damage signs like fatigue and appetite loss appear first. Yellow eyes indicate bilirubin levels above 2.5 mg/dL, meaning your liver has lost significant filtering capacity already.
Can moderate drinking still damage the liver?
Yes. Women develop signs of liver damage from alcohol from just two drinks daily due to body composition and hormone differences. Genetic factors, medications, obesity, and viral hepatitis increase damage risk even with moderate consumption. No amount is completely risk-free.
How long does it take for alcohol to damage the liver?
Fatty liver develops within two to four weeks of heavy drinking. Alcoholic hepatitis takes months to years. Cirrhosis typically requires 10-20 years of sustained heavy drinking, though genetics and drinking patterns cause faster progression in 15-20% of heavy drinkers.
Does stopping alcohol improve liver health?
Yes, dramatically. Stopping alcohol allows fat to clear, inflammation to resolve, and enzyme levels to normalize. Even with cirrhosis, abstinence prevents new scarring and improves five-year survival from 30% to 60%. Reversible signs of alcohol liver damage disappear within weeks to months.
Is alcohol liver damage life-threatening?
Advanced stages of alcohol related liver disease like cirrhosis cause life-threatening complications: variceal bleeding, liver cancer, kidney failure, and hepatic encephalopathy. Early fatty liver isn’t immediately dangerous but progresses to deadly stages without intervention. Cirrhosis kills 50% within five years.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.