Overview
Gallbladder disease is more common than many realize. It refers to a group of problems affecting the gallbladder, the bile ducts, and their function in digestion. Although the gallbladder is small, its impact on health can be large. Problems start when bile flow gets disrupted, leading to pain, inflammation, and serious complications.
Table of Contents
ToggleUnderstanding gallbladder diseases and symptoms is important because many people ignore early warning signs until an emergency occurs.
What Is Gallbladder Disease?
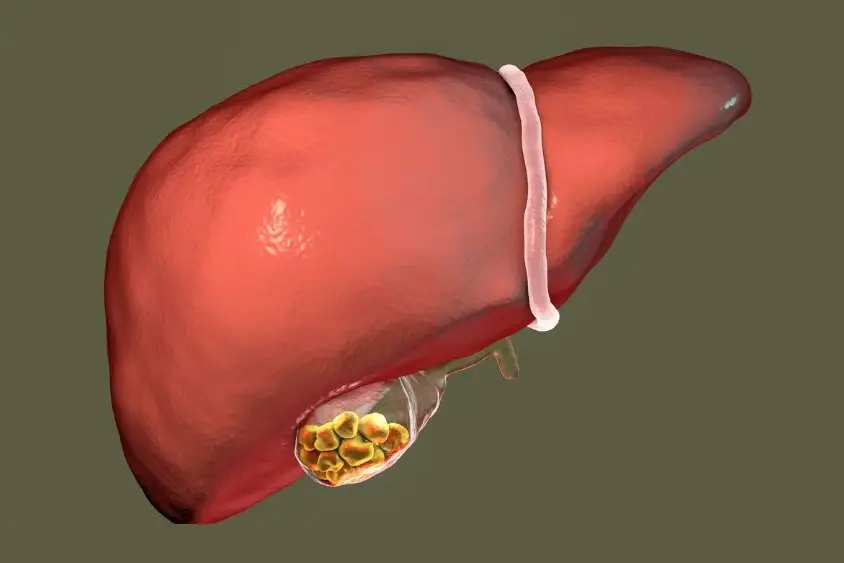
Gallbladder disease describes conditions that impair the normal role of the gallbladder. The gallbladder stores bile made by the liver, then releases it into the small intestine to help digest fat. When this process fails, symptoms appear.
Conditions under gallbladder disease include gallstones, cholecystitis, polyps, perforation, infection, and rarely gallbladder cancer. Since gallbladder problems progress differently in each person, no two cases look exactly alike.
What Conditions Affect The Gallbladder?
The gallbladder can develop stones, inflammation, blockages, infection, or abnormal growths. The most common condition is gallstones, but not every stone causes symptoms. Acute cholecystitis occurs when a stone blocks the bile duct, leading to swelling and pain.
Chronic cholecystitis happens after repeated attacks, making the gallbladder stiff and scarred. Gallbladder polyps are usually benign but large ones raise cancer risk. Rarely, gallbladder cancer develops, often discovered late.
How Common Is Gallbladder Disease?
Gallstones are extremely common worldwide. In some countries, more than 15 percent of adults have them. Many live symptom-free, but a portion will face signs of gallbladder disease like sharp pain or fever. Removal of the gallbladder is one of the most frequently performed abdominal surgeries.
Who Does Gallbladder Disease Affect?
Gallbladder disease affects all ages but is more common in adults. Women between 30 and 60 are at higher risk. People with obesity, diabetes, or rapid weight changes are also vulnerable.
Genetics play a role, with family history increasing risk. Some ethnic groups, such as Native Americans, show higher rates due to genetic predisposition.
What Are The 5 Fs Of Gallbladder Disease?
Doctors often teach medical students to remember the 5 Fs: female, fat, fertile, forty, and fair. These describe risk patterns seen in practice.
For example, women in their 40s with excess weight and hormonal influences often present with gallstones. However, men and young people also develop gallbladder disease.
How Does Gallbladder Disease Affect My Body?
When bile cannot pass normally, the digestive system struggles. Patients may report bloating, indigestion, and abdominal pain after eating fatty meals. Some experience fatty food intolerance that leads to discomfort and nausea and vomiting.
If bile backs up into the liver, it causes yellowing of the skin and eyes. The liver and gallbladder connection is strong, so damage to one affects the other.
What Are The Complications Of Gallbladder Disease?
Untreated gallbladder disease leads to serious complications.
Cholangitis
This is a dangerous infection of the bile ducts. It causes fever, chills, jaundice, and abdominal pain. It needs emergency treatment.
Cirrhosis
When bile flow is blocked for years, it scars the liver. This can cause permanent liver damage and increase the risk of cancer.
Pancreatitis
A gallstone can lodge in the duct that drains the pancreas. This triggers pancreatitis, which causes severe abdominal pain and sometimes life-threatening illness.
These complications of gallbladder disease show why early diagnosis and treatment are critical.
Symptoms And Causes

What Are The Signs And Symptoms Of Gallbladder Disease?
The most common gallbladder disease symptoms include right upper belly pain, pain after eating fatty meals, bloating, nausea, vomiting, and fever. People often mistake these for digestive upset, which delays treatment.
Biliary Colic
Pain that comes in waves, usually after a heavy meal. It may last from 30 minutes to several hours.
Acute Cholecystitis
Intense pain with fever, chills, and tenderness over the gallbladder. Needs immediate care.
Chronic Cholecystitis
Repeated attacks leading to scarring, constant mild discomfort, and poor digestion.
Other signs of gallbladder disease are diarrhea, light-colored stools, and dark urine.
What Causes Gallbladder Disease?
The most frequent causes of gallbladder disease are gallstones and bile flow obstruction. Gallstones form when bile has too much cholesterol or bilirubin. Other causes include infection, tumors, injury, or reduced gallbladder function.
Patients with metabolic syndrome, obesity, or a high-fat diet face increased risk. In rare cases, acalculous cholecystitis appears without stones, often in critically ill patients.
Diagnosis And Tests
How Is Gallbladder Disease Diagnosed?
Doctors start with medical history. They ask about pain, food triggers, and family history. They check for fever, jaundice, and tenderness in the right upper abdomen. Blood tests look for liver function changes and infection. Imaging confirms the diagnosis.
What Tests Are Used To Diagnose Gallbladder Disease?
The most used test is ultrasound (gallbladder ultrasound). It shows stones, swelling, or fluid. A CT scan may reveal complications like perforation. An MRI (gallbladder MRI) provides detailed bile duct images.
A HIDA scan (cholescintigraphy) checks gallbladder function. Doctors use ERCP (Endoscopic retrograde cholangiopancreatography) to diagnose and treat blockages. These imaging tests (ultrasound, CT scan, MRI) guide treatment decisions.
Management And Treatment

How Is Gallbladder Disease Treated?
Treatment depends on severity. Mild cases may improve with rest, fluids, and diet changes. Acute infection requires hospitalization, IV fluids, antibiotics, and pain relievers (ibuprofen, Aleve, Motrin). Endoscopy can remove duct stones. Surgery is the main gallbladder disease treatment.
Surgery / gallbladder removal is called cholecystectomy. Most are done laparoscopically, using small cuts and cameras. Recovery is faster than open surgery. Patients can live without the gallbladder because bile flows directly from the liver to the intestine. After surgery, most can eat normally but some may have temporary loose stools.
For high-risk patients who cannot undergo surgery, doctors may place a tube to drain the gallbladder or dissolve stones with medication. These are less common.
Outlook / Prognosis
What Can I Expect If I Have Gallbladder Disease?
With timely treatment, most people recover fully. Those with surgery usually return to normal life within weeks. Without treatment, the risk of repeated attacks, infection, and complications rises.
Rarely, untreated disease leads to perforated gallbladder or severe liver damage. For people diagnosed with polyps or cancer, outcomes depend on stage and treatment timing.
Prevention
How Can I Reduce My Risk Of Gallbladder Disease?
Prevention focuses on lifestyle. Maintain a healthy weight. Avoid rapid weight loss plans. Eat balanced meals rich in fiber, vegetables, and lean proteins. Limit fried and high-fat foods that worsen digestive issues related to gallbladder.
Exercise regularly to support bile flow. People with diabetes should manage blood sugar carefully. Regular checkups help spot problems early.
The Bottom Line
Gallbladder disease is common yet often ignored until pain strikes. By knowing the early warning signs and understanding the different conditions that affect the gallbladder, people can seek help before complications arise. Advances in gallbladder disease treatment mean that most cases resolve well.
The key is not to dismiss gallbladder disease symptoms as minor digestive upset. Early action protects both gallbladder and liver health.
FAQs
Q: What is the most common cause of gallbladder disease
The most common cause is gallstones which block bile flow, leading to pain, infection, and inflammation. This is why imaging and treatment are vital.
Q: Can gallbladder problems cause digestive symptoms
Yes, gallbladder problems often cause bloating, indigestion, nausea, and fatty food intolerance. These digestive symptoms are warning signs of serious disease needing medical care.
Q: How do doctors confirm gallbladder disease
Doctors use ultrasound first, then may use CT scan, MRI, HIDA scan, or ERCP. These tests identify stones, infections, blockages, and gallbladder function problems.
Q: What treatment is needed for acute gallbladder infection
Acute cholecystitis needs hospitalization, fluids, antibiotics, and sometimes urgent surgery. Delay in treatment raises the risk of complications such as perforated gallbladder or severe infection.
Q: Can gallbladder disease cause yellow skin and eyes
Yes, bile backup causes jaundice, where skin and eyes turn yellow. This sign means bile ducts are blocked and urgent medical evaluation is required.
Q: Is surgery always needed for gallbladder disease
Not always. Some mild cases improve with medication and diet changes, but recurrent pain or complications usually need gallbladder removal for lasting cure.
Q: What is the outlook after gallbladder removal
Most people live normal lives after gallbladder removal. Digestion adapts within weeks, though some may experience mild diarrhea or fatty food sensitivity for a short time.
Q: Can gallbladder disease increase cancer risk
Yes, long-term inflammation and large polyps may raise the risk of gallbladder cancer. Regular checkups help detect polyps and growths early to guide timely treatment.
Q: What are stool changes with gallbladder problems
Pale stools, greasy stools, or diarrhea can occur. These happen when bile flow is blocked. Dark urine often appears with the same condition, pointing to obstruction.
Q: How do I lower my chance of gallbladder problems
Eat a balanced diet, maintain a healthy weight, avoid fast dieting, and exercise regularly. These steps help lower gallstone risk and protect gallbladder health.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.