Yes. You can live without a gallbladder because the liver keeps making bile even after the gallbladder is removed. The body shifts to a steady bile flow that still allows you to digest food.
Table of Contents
ToggleThe main changes happen with how you handle fats, how your bowel reacts in the early weeks, and how you adjust your meals during recovery. Some people need short-term diet changes, while others return to regular eating within weeks. Most people regain strong digestive comfort with time, and long-term health stays normal.
Life Without A Gallbladder
Bile Flow Changes When The Gallbladder Is Removed
When your gallbladder is gone, bile is no longer stored in a pouch. The liver sends bile directly into the bile ducts. Bile drains steadily into your small intestine. You lose the big bursts of bile that happen after fatty meals.
That steady flow still breaks down fats, but it works differently. Many people feel no major problem. Some feel loose stools after rich meals.
How The Liver Compensates For The Missing Gallbladder
Your liver keeps making bile at its normal rate. Over weeks, the bile ducts widen a little. This change gives the system more capacity. The ducts help moderate flow into the intestine.
The liver also adjusts how much bile it releases at different times. These changes help most people adapt within weeks to months. Research shows the body compensates well for the missing storage.
How Food Digestion Behaves Without Bile Storage
You will still digest proteins, carbs, and fats. Bile mixes with food in the small intestine to help break fat into absorbable pieces. Without a gallbladder, fat digestion is slower when you eat a large fatty meal.
You may feel bloated, gassy, or have loose stools after heavy meals. Smaller, lower-fat meals reduce this effect and ease symptoms. Most people regain normal digestion over time.
Common Early Digestive Adjustments
Right after surgery, you may notice:
- Mild diarrhea or loose stools.
- Bloating and gas.
- Mild indigestion after rich meals.
These symptoms usually start in days. They often improve in four to eight weeks. If diarrhea or severe pain lasts longer, see your doctor.
Long-Term Digestive Adaptation Timeline
Most people adapt in one to three months. Some adapt in a few weeks. A minority takes longer. A small group develops ongoing symptoms called post-cholecystectomy syndrome. Tests can find treatable causes.
If you keep having symptoms beyond three months, your doctor can run tests and suggest treatments. Modern studies show good long-term outcomes for most patients.
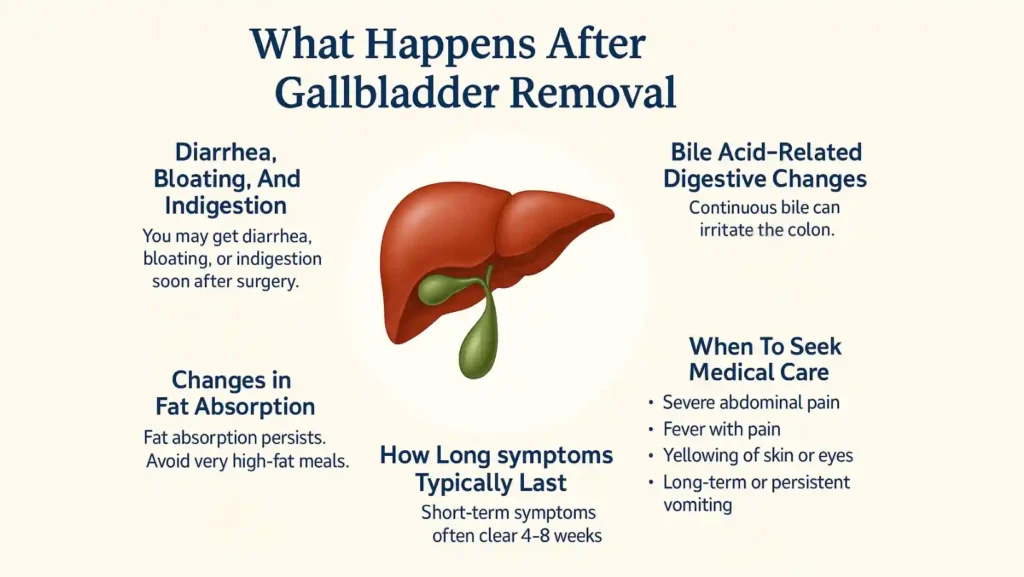
What Happens After Gallbladder Removal:
Diarrhea, Bloating, And Indigestion After Surgery
You may get diarrhea, bloating, or indigestion soon after surgery. These are common side effects of bile flow. Most cases are mild. You can manage symptoms with diet and fluids. If diarrhea is heavy or persistent, contact your care team. However, we advise follow-up for lasting or severe symptoms.
Bile Acid–Related Digestive Changes
Continuous bile in the intestine can irritate the colon. This irritation may cause watery stools. The problem may be bile acid malabsorption. Doctors sometimes use medicines that bind bile acids. These medicines reduce diarrhea when diet changes do not help. Your doctor will test and treat based on how severe your symptoms are.
How Long Post-Surgery Symptoms Typically Last
Short-term symptoms often clear in four to eight weeks. You may return to normal in three months. If symptoms continue longer, your doctor will check for other causes. Some people require medicine or further testing for bile duct issues or other problems. Most people do not need further surgery.
Changes In Fat Absorption After Cholecystectomy
Fat absorption continues after gallbladder removal. The change is usually minor. The steady bile flow still emulsifies fats. Very high-fat meals can overwhelm the system, causing loose stools.
If long-term fat malabsorption occurs, doctors check vitamin levels and may advise supplements. You should be able to keep normal nutrition without extra treatment.
When To Seek Medical Care Post-Surgery
See your doctor right away if you have:
- Severe abdominal pain.
- Fever with pain.
- Yellowing of skin or eyes.
- Dark urine or persistent vomiting.
These signs may mean a blocked bile duct, infection, or other serious issue. Early care prevents worse outcomes. If diarrhea causes weight loss or dehydration, seek help quickly.
Living Without a Gallbladder Diet
Why Low-Fat Meals Are Recommended Early On
Right after surgery, your body needs calm food. You should eat low-fat meals. Low-fat food reduces the need for a large bile surge. It cuts the risk of diarrhea and belly pain. You can live without a gallbladder ; know that a short low-fat period helps your body adapt. Start with small portions. Eat plain boiled rice, steamed vegetables, and lean chicken. Avoid greasy sauces and heavy creams.
Foods That Help Stabilize Digestion Post-Removal
Choose foods that are easy to digest. These items help you feel steady:
- Lean protein such as fish and skinless poultry.
- Cooked vegetables like carrots and zucchini.
- Plain fruits such as bananas and applesauce.
- Low-fat dairy or dairy alternatives.
- Whole grains in small amounts.
These choices support adaptation when you study life without a gallbladder . They make digestion smoother. They cut the chance of loose stools.
Foods That May Trigger Symptoms (Fatty, Fried, Processed)
High-fat foods often cause trouble. Avoid these at first: fried food, fatty cuts of meat, full-fat dairy, creamy desserts, and oily snacks. Processed fast food can trigger bloating and diarrhea. If you test a food and it causes pain, stop and wait a few days before trying again.
Meal-Spacing and Portion Guidelines
Eat smaller meals more often. Try five small meals a day instead of three large ones. This spacing keeps bile use mild and steady. Keep portions modest. A plate one-third full of lean protein, one-third vegetables, and one-third whole grains is a good start.
Long-Term Diet Adjustments for Digestive Comfort
After a few weeks, reintroduce healthy fats slowly. Try a teaspoon of olive oil or a small handful of nuts. Watch for symptoms. Keep a food diary. Over time, many people return to a normal, balanced diet. If you still have trouble, a registered dietitian can help design a living without a gallbladder diet tailored to you.
Gallbladder Removal Complications
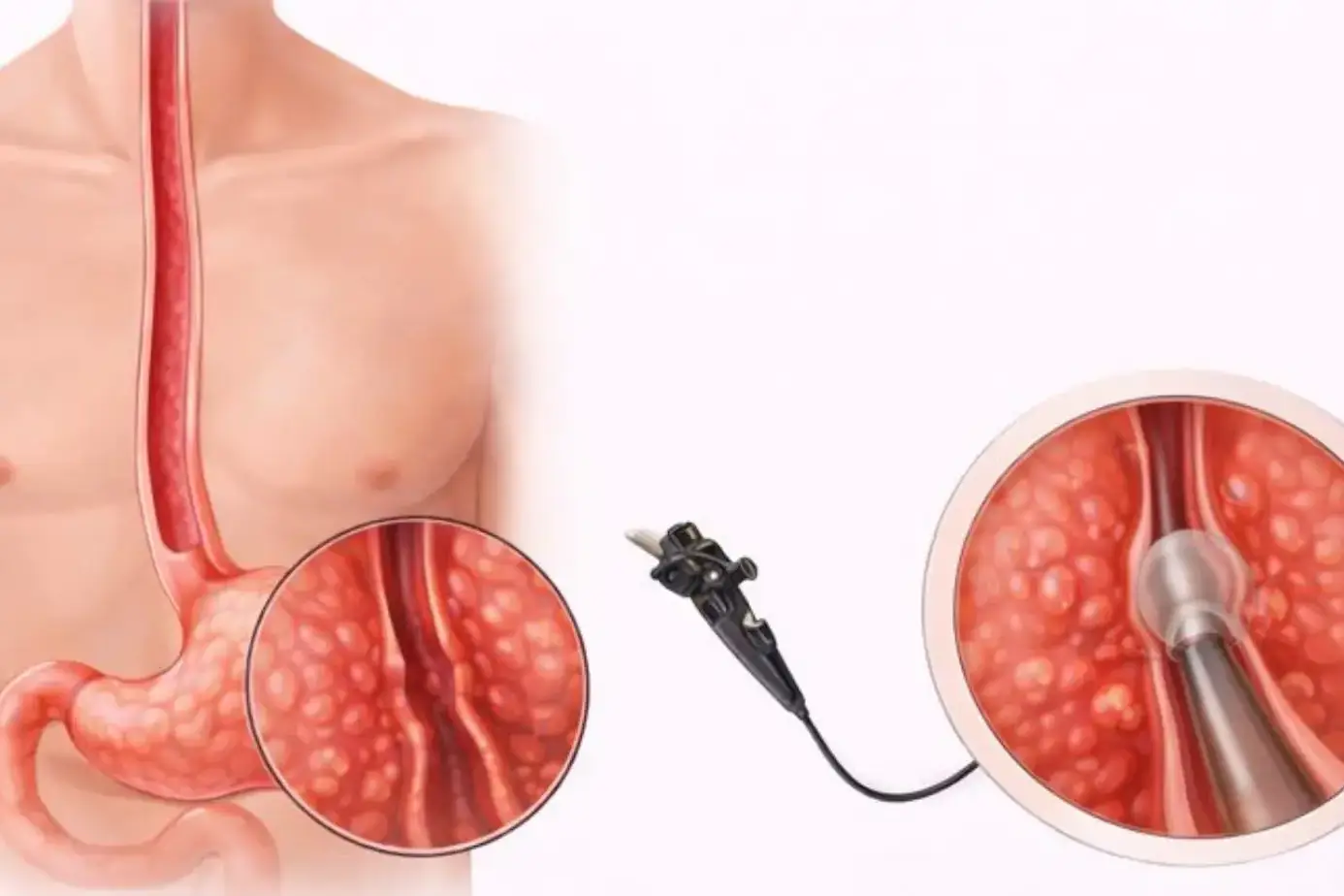
Bile Reflux After Gallbladder Removal
Bile reflux occurs when bile moves backward into the stomach. It can cause burning and nausea. If you notice persistent heartburn after meals, tell your doctor. Treatments include medicines that reduce bile and changes to what you eat. Early care helps prevent long-term irritation.
Post-Cholecystectomy Syndrome Symptoms
Post-cholecystectomy syndrome means ongoing symptoms after surgery. You may have pain, bloating, or nausea. You may also have irregular bowel movements. These signs can come from bile flow changes, small stones left behind, or other gut problems. Doctors run tests and treat the specific cause.
Persistent Diarrhea and Fat Malabsorption
Some people get chronic watery diarrhea. This can stem from bile acid reaching the colon. Doctors may use bile acid binders to slow the bowel. Severe fat malabsorption is rare. If your stools look greasy or you lose weight, get medical testing.
When Complications Require Medical Attention
Seek care if you have severe belly pain, fever, yellow eyes, or dark urine. These signs may mean bile duct blockage or infection. Also, act if you have sudden weight loss or very loose stools for weeks. Timely testing can find problems early.
Rare Surgical and Metabolic Complications
Rare problems include injury to the bile duct during surgery and infection at the incision. These events are uncommon. Surgeons and hospitals use safety steps to lower risk. If you have unusual symptoms, report them promptly.
How the Body Works Without a Gallbladder
Continuous Bile Release Instead of Storage and Release
The gallbladder stores bile and releases it at meals. After removal, the liver sends bile directly into the intestine. This flow is steady rather than pulsed. Your gut adapts to the steady supply. This change explains why you can still digest food and why you can live without a gallbladder. It is a realistic question with a positive answer for most people.
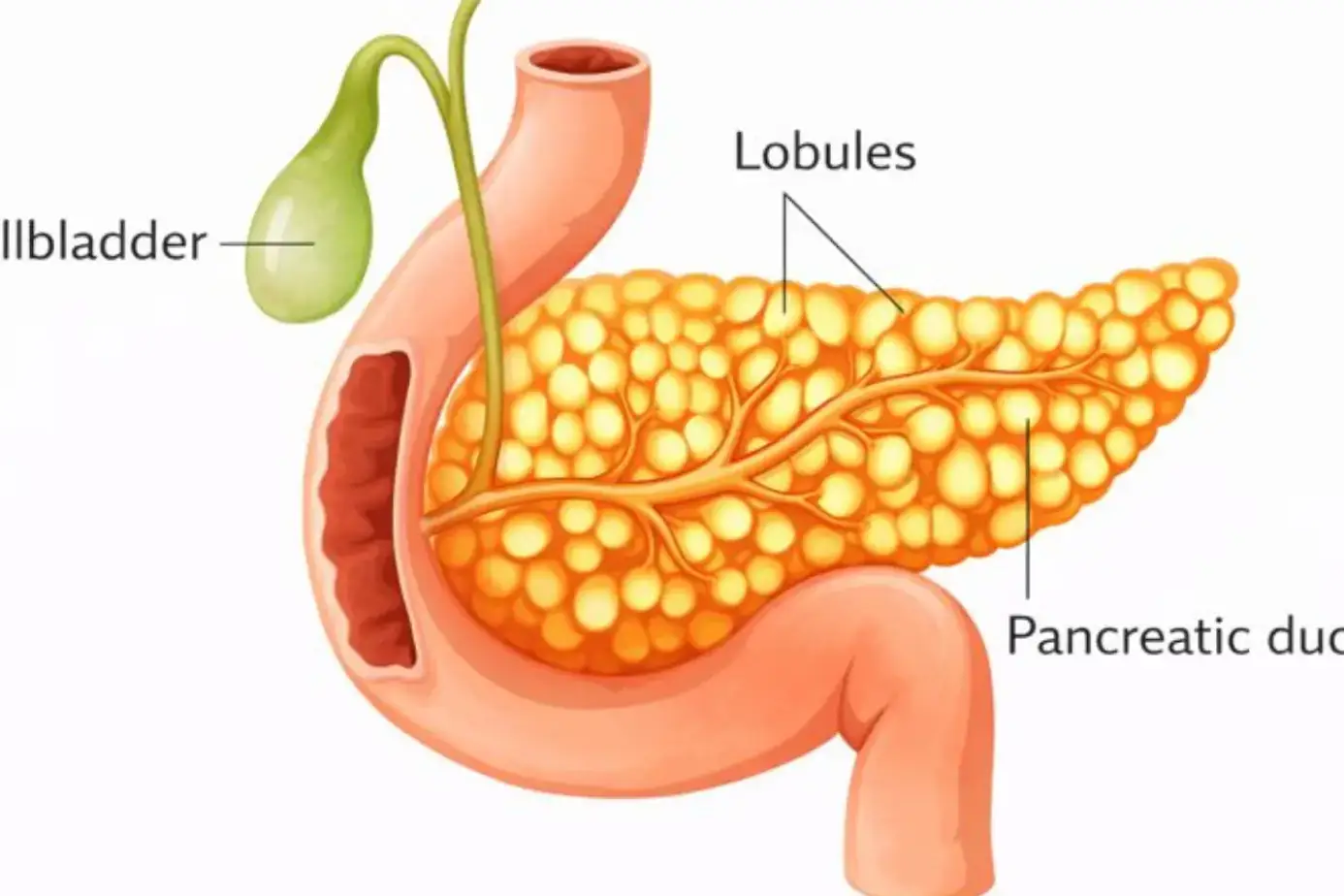
How Digestive Enzymes Support Fat Breakdown
Pancreatic enzymes and bile work together to digest fat. The pancreas releases enzymes when you eat. Bile helps break fat into small droplets. Together, they let your body absorb fat even without a gallbladder. If you keep meals smaller, enzymes and bile work better.
Changes in Nutrient Absorption
Most nutrients are absorbed normally without a gallbladder. A few people notice mild trouble with very fatty meals. If absorption falls, you may lose weight or feel tired. Tests can check vitamin and fat levels. Simple diet fixes or supplements solve most issues.
The Liver’s Compensatory Role
The liver increases bile flow, and the bile ducts may widen slightly. This change helps carry bile when there is no storage. Over weeks to months, this compensation reduces symptoms. Learning how the body works without a gallbladder helps you set the right diet and follow-up plan.
Long-Term Digestive Efficiency Without a Gallbladder
Long-term, many people return to normal eating. The body adapts. Digestive efficiency often matches pre-surgery levels. You may need to avoid very large fatty meals. With good habits, you can live well and stay active.
Surgery Overview: What Gallbladder Removal Involves
Laparoscopic vs Traditional Cholecystectomy
Laparoscopic cholecystectomy uses small cuts and a camera. It causes less pain and faster recovery. Open surgery uses a larger cut. Surgeons use open surgery only when needed. Most people have laparoscopic surgery. Ask your surgeon about the best option for you.
Typical Recovery Timeline
After laparoscopic surgery, you may leave the hospital the same day. You can walk the same day. Rest at home for a few days. Most return to normal work in one to two weeks. Open surgery needs a longer healing time. Follow the surgeon’s instructions on lifting and activity.
Pain Management After the Procedure
Doctors give pain medicines for short periods. You may use over-the-counter medicines after a few days. Avoid long-term opioid use. Gentle walking helps reduce pain and prevent blood clots. Report any increasing pain to your care team.
Returning to Normal Activities Safely
Start with slow walking and light chores. Do not lift heavy objects for a few weeks. Drive only when pain medicines do not slow your reactions. Your surgeon will clear you to resume sports or heavy work.
When to Seek Medical Help After Gallbladder Removal
Severe Pain or Persistent Digestive Issues
Seek urgent care for sharp, worsening pain. Also seek help for ongoing vomiting or inability to keep food down. These issues may show infection or blockage.
Jaundice or Signs of Bile Duct Problems
Yellow skin or yellow eyes require immediate testing. These signs may mean clogged bile ducts. Early treatment prevents liver damage.
Abnormal Stools or Inability to Digest Fat
If your stools are greasy, pale, or foul-smelling, or you lose weight, see a doctor. These signs suggest fat malabsorption.
Symptoms Indicating Complications
Fever, wound drainage, or swelling around the incision means infection. Contact your clinic right away. Quick care reduces the chance of worse problems.
Prevention & Long-Term Health Tips
Maintaining a Balanced Digestive-Friendly Diet
Keep a diet rich in vegetables, lean protein, and whole grains. Limit fried food and heavy sauces. Use small portions of healthy fats.
Hydration and Fiber Intake
Drink water often. Add fiber slowly to avoid gas. Soluble fiber can help stool consistency. High fiber also supports gut health.
Lifestyle Habits to Support Liver Health
Avoid heavy alcohol use. Keep a healthy weight. Exercise regularly. These habits protect your liver and digestion.
Supplements Some Patients Benefit From
A doctor may suggest bile acid binders for diarrhea. Probiotics can help gut balance. Take vitamins only if tests show a need.
FAQ
Is it harder to digest food without a gallbladder?
Yes, you may find fatty meals harder at first. With time, smaller low-fat meals let your digestion settle and work well again.
Does weight gain or weight loss happen after removal?
You may lose weight soon after surgery due to low appetite. Long term, weight changes depend on your diet and activity.
Can you live a normal life long term?
Yes. Most people return to normal life. Proper diet and follow-up care let you stay active and healthy.
Will removing the gallbladder affect your life expectancy?
No. Removing the gallbladder does not shorten life expectancy. It removes a source of pain and infection.
How long does it take for digestion to normalize without a gallbladder?
Most people normalize in two to four weeks. Some need a few months. Persistent issues need medical follow-up.
Can stress or anxiety worsen digestive issues after cholecystectomy?
Yes. Stress can increase gut sensitivity and worsen symptoms. Simple stress reduction helps digestive recovery.
Can pregnancy be affected by gallbladder removal?
No. If you recover well, pregnancy is usually safe. Plan timing with your obstetrician and surgeon.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.