Achalasia is a rare disorder where the lower esophageal sphincter, the valve between your esophagus and stomach, stays tight when it should relax. This makes swallowing slow, painful, or inconsistent, and food can collect in the esophagus.
Table of Contents
ToggleThe problem happens because the nerve cells that control this valve stop working. Since the nerve loss cannot be reversed, care focuses on improving the passage of food and preventing long-term harm.
Current achalasia treatment options range from medicines and Botox for short-term relief to pneumatic dilation, laparoscopic Heller myotomy, and POEM surgery for achalasia for longer-lasting results.
Each method lowers the tight muscle differently, and the best option depends on the achalasia type, symptom severity, and your overall health.
Best Treatment for Achalasia
The best treatment for achalasia depend on the manometry subtype, your age, health, and local expertise. Common durable choices include pneumatic dilation, laparoscopic Heller myotomy, and POEM. Short-term options include medications and Botox. Major society guidelines recommend matching therapy to the achalasia type and the patient.
What to expect when choosing treatment
You and your doctor weigh relief of swallowing, risk of reflux, recovery time, and long-term success. If you want less invasive care, you may try achalasia non-surgical treatment first. If you want a durable fix, you may choose an operation. Centers with experience achieve better results.
How Treatment Goals Differ by Achalasia Type
High-resolution manometry divides achalasia into types I, II, and III. Each has different goals.
- Type I: Improve emptying of a weak, floppy esophagus.
- Type II: Restore flow and reduce pressure. This type responds best to most treatments.
- Type III: Stop spasm in the esophagus body. Long myotomy often works best.
You need manometry to guide the plan. Type II has the highest success with most approaches.
Key Factors That Decide the Best Treatment
Decisions come from test results and your situation:
- Manometry subtype.
- Appearance on barium swallow (size, shape).
- Endoscopy findings and risk of other disease.
- Your age and fitness for surgery.
- Preference about reflux after treatment.
- Local availability of POEM or experienced surgeons.
If you have a very dilated or sigmoid esophagus, surgery by a specialist may be better than non-surgical approaches.
Long-Term Effectiveness of Major Options
- Pneumatic dilation gives good long-term symptom relief for many people. It may need repeat sessions.
- Laparoscopic Heller myotomy is durable. Surgeons often add fundoplication to lower reflux risk.
- POEM shows high short-term and mid-term success. It may raise reflux risk more than Heller myotomy.
All choices can help. You must plan a follow-up to catch the return of symptoms or reflux. Matching therapy to subtype improves outcomes.
Achalasia Cardia Treatment
What Achalasia Cardia Means Clinically
“Achalasia cardia” means the lower esophagus and sphincter fail to relax. You feel food stick, regurgitate, or lose weight. Tests show weak or absent contractions and a tight lower sphincter. Doctors use manometry, barium swallow, and endoscopy to confirm the diagnosis and rule out other causes.
Diagnostic Tests Before Selecting Treatment
Before you decide, clinicians use three main tests:
- High-resolution manometry. It gives the type.
- Timed barium swallow. It shows emptying and esophagus shape.
- Upper endoscopy. It rules out cancer and clears retained food.
These tests guide whether achalasia cardia treatment should be dilation, myotomy, or POEM. Evidence supports manometry as the key test.
Early-Stage Versus Advanced Achalasia Management
If your esophagus is early-stage, you may respond well to less invasive options. If it is advanced and very dilated, surgery is often needed. End-stage, distorted esophagus may require complex repair or specialist referral. Discuss risks and benefits with a team experienced in achalasia care.
Achalasia Non-Surgical Treatment
Non-surgical care can be a first step or a choice when surgery is risky.
Medications: Nitrates and Calcium Channel Blockers
Doctors usually prescribe nitrates or calcium channel blockers to relax the lower sphincter a little. These drugs give mild, short-lived relief. Side effects include low blood pressure and headache. They are for short-term use or for patients who cannot have procedures.
Botox Injection: Short-Term Relief
Botulinum toxin injected into the sphincter relaxes muscle for months. Benefits wear off with time. Repeated injections lose effectiveness and may cause local scarring. Botox is a reasonable option if you are frail or need a temporary fix before a more durable therapy.
Who Should Choose Non-Surgical Options
Non-surgical therapy suits you if you are elderly, have serious medical problems, or need quick symptom relief. Many people prefer durable options when possible. If you choose achalasia non-surgical treatment , plan follow-up and know that more definitive therapy may be needed later.
Achalasia Surgery Options
Surgery offers long-term relief for many people. The main surgical choices are pneumatic dilation, laparoscopic Heller myotomy, and POEM.
Pneumatic Dilation: Benefits and Risks
Pneumatic dilation stretches the sphincter with a balloon. You usually go home the same day. Benefits include strong symptom relief for many people. Risks include esophageal perforation in a small percentage. Repeat dilations may be needed. Graded pneumatic dilation is an effective choice for many patients.
Heller Myotomy: How It Works and Success Rate
Laparoscopic Heller myotomy cuts the tight muscle at the sphincter. Surgeons commonly add a partial fundoplication to reduce reflux. The operation gives durable relief and is well studied. Recovery requires short hospitalization and gradual diet progression. Outcomes are good when done at experienced centers.
When Surgery Is Preferred Over Non-Surgical Treatment
Surgery is preferred when you want a lasting result, when dilation fails, or when the esophagus shows advanced change. Your team will review test results and explain risks. Choose a center with experience in achalasia surgery options to improve outcomes.
POEM Surgery for Achalasia
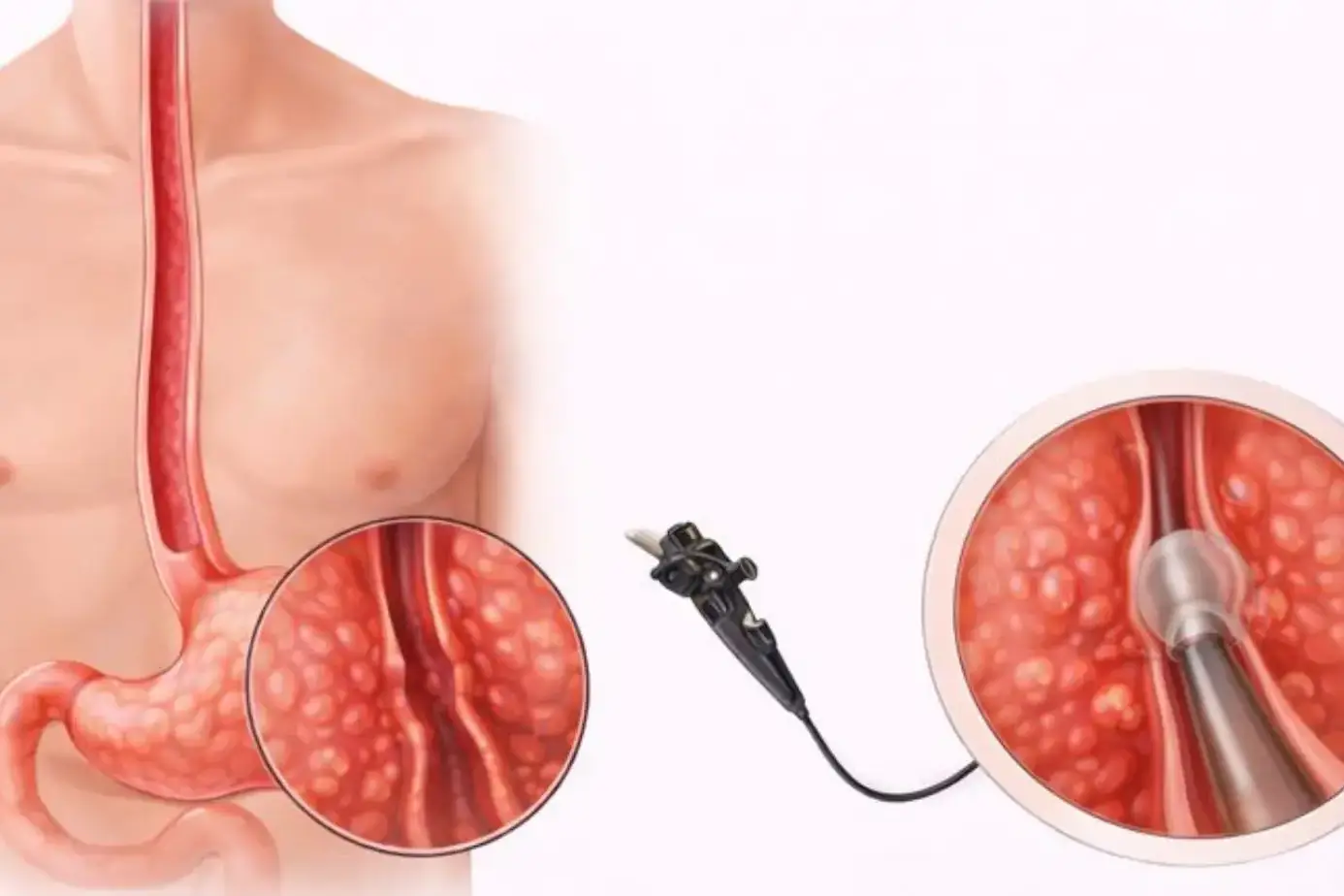
How POEM Works (Endoscopic Myotomy)
POEM stands for peroral endoscopic myotomy. You receive general anesthesia. A flexible endoscope goes through your mouth into the esophagus. The doctor makes a short tunnel inside the esophagus wall.
They cut the muscle causing the blockage. The tunnel is closed with clips. POEM removes the tight band that stops food from passing. POEM often needs a short hospital stay and quick recovery.
Why POEM Is Ideal for Type III Achalasia
Type III achalasia has spasm in the esophagus body. POEM allows a long myotomy along the esophagus. That length helps release spasm and reduce chest pain. Studies show better outcomes for Type III with POEM than with other options. If you have spasm, POEM may give superior symptom relief.
Risks and Post-Procedure Reflux Concerns
POEM often relieves swallowing. You also face higher reflux risk than after Heller myotomy with fundoplication. Many patients need proton pump inhibitors after POEM. Discuss reflux risk and the need for long-term acid control before choosing POEM. Early higher reflux rates after POEM. Long-term reflux data are still growing.
Post-Treatment Care & Lifestyle
Diet Changes After Treatment
After dilation, myotomy, or POEM, you start with liquids. Move to soft foods in days to weeks. Chew food well. Eat small portions. Avoid tough, dry, or crumbly foods until healing is complete. Centers commonly give a staged diet plan and dietitian support. Many patients gradually return to normal foods. Follow your center’s written diet instructions closely.
Managing Reflux Symptoms
If you develop reflux, your doctor usually prescribes a proton pump inhibitor. Elevate your bed head. Avoid late meals. If reflux persists, get testing and an endoscopy. Long-term reflux can injure the esophagus. Treat reflux early to prevent damage. POEM patients need closer reflux surveillance.
Follow-Up Tests and Long-Term Monitoring
You need a follow-up to watch for symptoms and reflux. Your team may use timed barium swallow, manometry, endoscopy, and pH testing if symptoms return. Routine surveillance for cancer is controversial. Major guidelines do not recommend universal endoscopic screening. Targeted surveillance is essential if achalasia is long-standing. Discuss a customized follow-up plan with your team.
FAQs
What Is the Most Effective Long-Term Treatment?
Effectiveness depends on your achalasia type. POEM, Heller myotomy, and pneumatic dilation all work. POEM and Heller offer high-durable relief in many studies. Choose by subtype and reflux risk.
Can Achalasia Return After Treatment?
Yes. Symptoms can recur after any therapy. Dilation may require repeats. Myotomy and POEM reduce recurrence risk, but return can occur. Keep regular follow-up and report new symptoms.
Is Achalasia Curable or Only Manageable?
Achalasia is chronic. Treatments improve swallowing and quality of life. They do not restore the original nerve cells. You receive symptom control rather than a cure.
How Soon Will Swallowing Improve?
Many patients notice improved swallowing within days to weeks after POEM or myotomy. Balloon dilation may work quickly. Botox acts fast but only temporarily. Recovery varies by person.
Is POEM Better Than Heller Myotomy?
POEM often equals or exceeds Heller for symptom relief. POEM has shorter recovery. POEM has higher early reflux rates. Choice depends on reflux tolerance and surgical expertise.
What Are the Risks of Pneumatic Dilation?
Pneumatic dilation risks include chest pain and possible esophageal perforation. Perforation is uncommon. Repeat dilations may be necessary for lasting relief. Centers monitor closely for complications.
Can Achalasia Increase Cancer Risk?
Achalasia raises long-term risk of esophageal cancer mildly. The absolute risk is low. Guidelines do not recommend routine endoscopic surveillance for all patients. Consider targeted screening if the disease lasts many years. Evidence on cancer risk is limited and evolving.
Can Achalasia Be Treated Without Surgery?
Yes. You can try medicines, Botox, or pneumatic dilation. These non-surgical options give short-term to mid-term relief. If you can tolerate definitive therapy, discuss durable options.
Do I Need Lifelong Monitoring After Treatment?
Most people need periodic checks for symptoms, nutrition, and reflux. Testing occurs if symptoms return or if reflux is hard to control. Work with your team for a monitoring plan.
Does Achalasia Affect Life Expectancy?
With diagnosis and treatment, most patients live normal lives. Untreated, severe disease can lead to weight loss and complications. Early care improves outcomes.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin