Welcome to our comprehensive guide on bile duct dysfunction. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for this condition. Bile duct dysfunction, also known as biliary obstruction, occurs when the bile ducts are blocked, leading to various complications. It is important to understand the causes and care for this condition to manage it effectively.
Table of Contents
ToggleIf you or a loved one is experiencing symptoms like abdominal pain, nausea, jaundice, or changes in stool color, it is crucial to seek medical attention. Bile duct dysfunction can be caused by factors such as gallstones, inflammation, trauma, tumors, infections, and liver damage. Prompt diagnosis and appropriate care are essential to prevent complications and promote overall well-being.
Throughout this article, we will delve deeper into the causes of biliary obstruction and the risk factors associated with it. We will also discuss the symptoms, diagnosis methods, and the various treatment options available. Additionally, we will provide insights into preventing bile duct dysfunction and minimizing its impact on your health.
By understanding the causes, seeking early medical intervention, and adopting preventive measures, you can effectively manage bile duct dysfunction and ensure better long-term health. Follow our guide to gain valuable insights into this condition and take control of your health journey.
What is Biliary Obstruction?
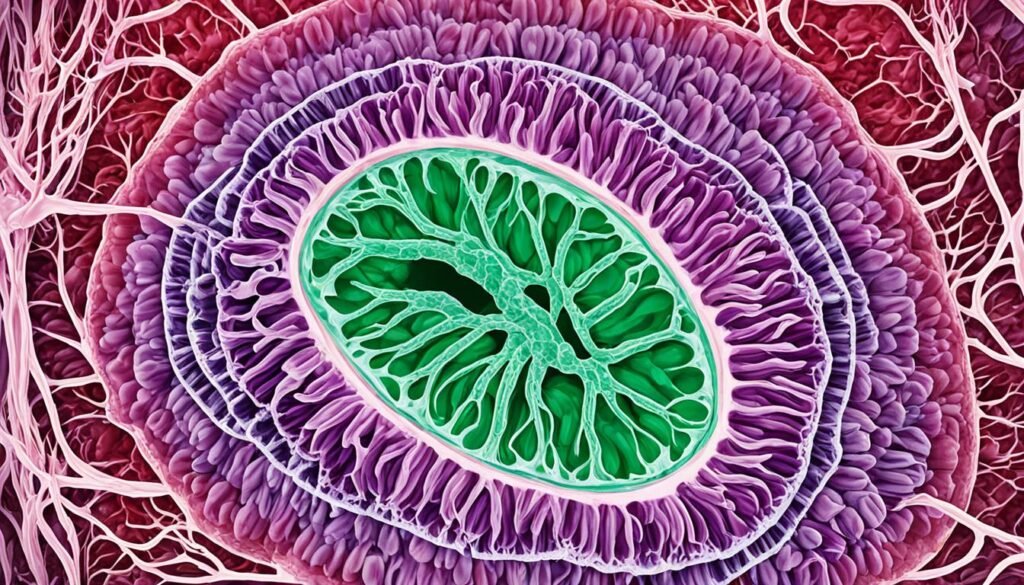
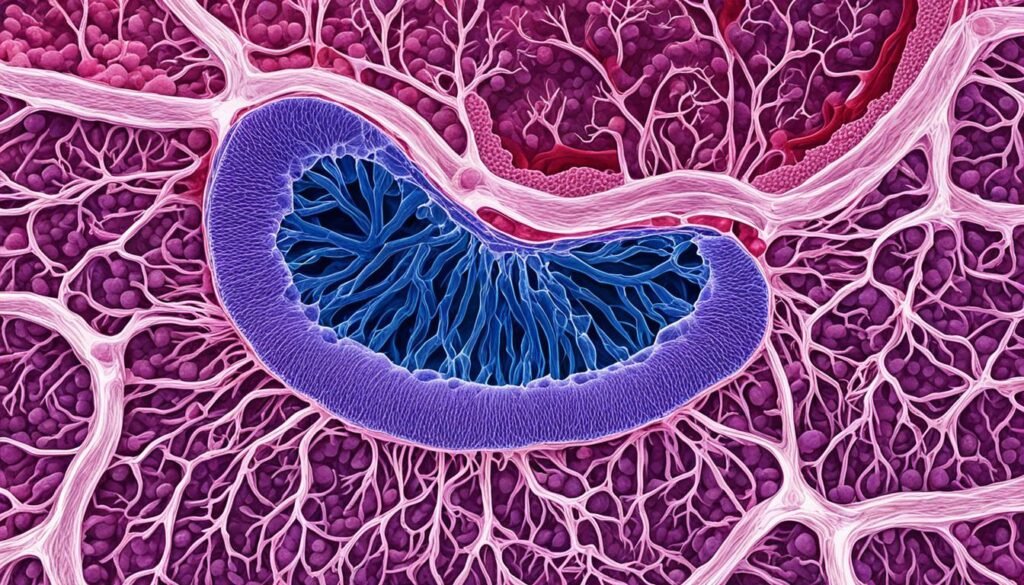
Biliary obstruction occurs when the bile ducts, which are responsible for carrying bile from the liver and gallbladder to the duodenum, become blocked. Bile is a vital fluid produced by the liver that aids in the digestion of fats.
This blockage can occur in either the intrahepatic ducts within the liver or the extrahepatic ducts that run towards the small intestine. If left untreated, bile duct obstruction can lead to severe complications, including liver diseases.
Biliary obstruction can be a result of various factors such as gallstones, inflammation, trauma, tumors, infections, and liver damage. Understanding the causes and identifying the symptoms of biliary obstruction is essential for accurate diagnosis and prompt treatment.
Causes of Biliary Obstruction
Biliary obstruction, the blockage of the bile ducts, can occur due to various causes. Identifying the underlying reason is essential for effective treatment and management of this condition. Some common causes of biliary obstruction include:
- Gallstones: The formation of hardened deposits in the gallbladder or bile ducts.
- Inflammation of the bile ducts: Swelling and irritation of the tubes that carry bile.
- Trauma: Physical injury to the bile ducts or surrounding organs.
- Tumors: Abnormal growths in the liver, gallbladder, pancreas, or bile ducts.
- Infections: Bacterial or parasitic infections that affect the bile ducts.
- Cysts: Fluid-filled sacs that develop within or near the bile ducts.
- Enlarged lymph nodes: Abnormal swelling of lymph nodes that can compress the bile ducts.
- Pancreatitis: Inflammation of the pancreas that can lead to bile duct obstruction.
- Gallbladder or liver surgery: Previous surgical procedures in the area can cause scarring or blockage.
- Cirrhosis: Severe liver damage resulting in the disruption of normal bile flow.
- Choledochal cysts: Congenital abnormalities that affect the bile ducts.
Some of these causes may have genetic connections, while others may be acquired through lifestyle or medical conditions. Understanding the underlying cause of biliary obstruction is crucial for appropriate treatment and preventing further complications.
Major Causes of Biliary Obstruction
| Cause | Description |
|---|---|
| Gallstones | Hardened deposits in the gallbladder or bile ducts. |
| Inflammation of the bile ducts | Swelling and irritation of the tubes that carry bile. |
| Trauma | Physical injury to the bile ducts or surrounding organs. |
| Tumors | Abnormal growths in the liver, gallbladder, pancreas, or bile ducts. |
| Infections | Bacterial or parasitic infections affecting the bile ducts. |
| Cysts | Fluid-filled sacs within or near the bile ducts. |
| Enlarged lymph nodes | Abnormal swelling of lymph nodes compressing the bile ducts. |
| Pancreatitis | Inflammation of the pancreas leading to bile duct obstruction. |
| Gallbladder or liver surgery | Previous surgical procedures causing scarring or blockage. |
| Cirrhosis | Severe liver damage disrupting normal bile flow. |
| Choledochal cysts | Congenital abnormalities affecting the bile ducts. |
Risk Factors for Biliary Obstruction
Several risk factors can increase the likelihood of developing biliary obstruction. It is important to be aware of these risk factors and seek medical attention if symptoms or complications arise.
Gallstones
A history of gallstones can significantly increase the risk of developing biliary obstruction. Gallstones can block the bile ducts, leading to obstruction and related complications.
Caroli Disease
Caroli disease, a rare disorder that causes the enlargement of bile ducts, is another risk factor for biliary obstruction. This condition can impair the flow of bile and lead to blockages.
Chronic Pancreatitis and Pancreatic Cancer
Chronic pancreatitis, a long-term inflammation of the pancreas, and pancreatic cancer are associated with an increased risk of biliary obstruction. These conditions can affect the normal functioning of the pancreas and bile ducts.
Abdominal Injury
Abdominal injuries, such as those caused by accidents or trauma, can damage the bile ducts and contribute to biliary obstruction.
Obesity and Rapid Weight Loss
Obesity and rapid weight loss can increase the risk of biliary obstruction. Excess weight and sudden changes in weight can affect the bile flow and contribute to the development of blockages.
Red Blood Cell Disorders
Red blood cell disorders, like sickle cell anemia, can lead to the accumulation of bilirubin and increase the risk of biliary obstruction.
Genetics
Certain genetic factors can predispose individuals to developing biliary obstruction. Genetic variations can affect the structure and function of the bile ducts, increasing the vulnerability to obstruction.
Risk Factors for Biliary Obstruction
| Risk Factors |
|---|
| Gallstones |
| Caroli Disease |
| Chronic Pancreatitis |
| Pancreatic Cancer |
| Abdominal Injury |
| Obesity |
| Rapid Weight Loss |
| Red Blood Cell Disorders |
| Genetics |
Symptoms and Diagnosis of Biliary Obstruction
If you are experiencing any of the following symptoms, it may be a sign of biliary obstruction:
- Light-colored stools
- Dark urine
- Jaundice (yellowing of the skin and eyes)
- Abdominal pain in the upper right side
- Nausea
- Vomiting
- Weight loss
- Itching
These symptoms can vary in severity and may be accompanied by other discomforts. If you are experiencing any of these symptoms, it is important to seek medical attention for a proper diagnosis.
Diagnosing Biliary Obstruction
To diagnose biliary obstruction, your healthcare provider will perform a thorough physical examination and may recommend the following tests:
- Blood tests: These tests help check your liver function and bilirubin levels, which can indicate the presence of biliary obstruction.
- Imaging tests: Your healthcare provider may order ultrasound, CT scan, MRI, MRCP, or ERCP to visualize your bile ducts and assess any blockages or abnormalities.
These diagnostic tests play a crucial role in identifying the presence and cause of biliary obstruction, enabling your healthcare provider to develop an appropriate treatment plan.
| Diagnostic Tests | Description |
|---|---|
| Blood tests | Measure liver function and bilirubin levels |
| Ultrasound | Use sound waves to create images of your bile ducts |
| CT scan | Combine X-rays to produce detailed cross-sectional images |
| MRI | Use powerful magnets and radio waves to generate images |
| MRCP | Magnetic resonance cholangiopancreatography to visualize bile ducts |
| ERCP | Endoscopic retrograde cholangiopancreatography to view and treat blockages |
If diagnosed with biliary obstruction, understanding the cause of the blockage is essential for effective treatment. Your healthcare provider will develop a personalized treatment plan based on the underlying cause and severity of your condition.
Treatment Options for Biliary Obstruction
When it comes to treating biliary obstruction, the main objective is to address the underlying cause of the blockage and relieve it promptly to prevent complications. The choice of treatment depends on various factors, including the specific cause of the obstruction.
Here are some common treatment options for biliary obstruction:
- Cholecystectomy: In cases where gallstones are the underlying cause, the surgical removal of the gallbladder, known as cholecystectomy, may be recommended. This procedure eliminates the source of the obstruction and prevents its recurrence.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): ERCP is a minimally invasive procedure that combines endoscopy and fluoroscopy to diagnose and treat bile duct disorders. It can be used to remove stones causing the obstruction or place a stent to keep the duct open.
- Surgical Removal or Treatment of Tumors: In cases where tumors are causing the biliary obstruction, surgical removal or other targeted treatments may be necessary. The specific approach depends on the location, size, and stage of the tumor.
- Medication for Infections or Parasites: If the obstruction is caused by infections or parasites, the appropriate medication will be prescribed to address the underlying infection and eliminate the parasites.
- Other Therapeutic Interventions: Depending on the underlying cause and severity of the obstruction, additional therapeutic interventions such as bile duct dilation, biliary stenting, or percutaneous transhepatic cholangiography may be required to restore the normal flow of bile.
Prompt treatment is crucial to prevent complications associated with biliary obstruction, such as infections, sepsis, and the development of chronic liver diseases. By addressing the underlying cause of the obstruction, these treatment options aim to alleviate symptoms, restore normal bile flow, and improve overall health and quality of life.

Complications of Biliary Obstruction
If left untreated, biliary obstruction can lead to serious complications that can significantly impact your health and quality of life. Early detection and appropriate treatment are essential in order to prevent these complications and ensure better outcomes.
- Infections: Biliary obstruction can increase the risk of developing infections in the bile ducts, liver, or surrounding areas. These infections can be challenging to treat and may require antibiotics or drainage procedures.
- Sepsis: In severe cases, biliary obstruction can lead to sepsis, a life-threatening condition where the body’s response to infection causes widespread inflammation. Immediate medical attention is crucial to prevent sepsis and its complications.
- Chronic Liver Diseases: Prolonged biliary obstruction can contribute to the development of chronic liver diseases such as biliary cirrhosis. This condition causes liver damage, scarring, and impaired liver function, leading to long-term complications.
- Jaundice: Biliary obstruction can cause a buildup of bilirubin in the bloodstream, resulting in jaundice. Jaundice is characterized by yellowing of the skin, eyes, and mucous membranes and can indicate a serious underlying issue.
Seeking early medical intervention and appropriate treatment for biliary obstruction is crucial in order to prevent these complications and maintain good health. Complying with the prescribed treatment plan and closely monitoring your symptoms can help minimize the impact of biliary obstruction on your overall well-being.

Prevention of Biliary Obstruction
While certain causes of biliary obstruction may not be preventable, making certain lifestyle changes can reduce the risk. By adopting a healthy diet and managing your weight, you can take proactive steps to prevent biliary obstruction. Here are some key prevention strategies:
- Increased Fiber Intake: Incorporate fiber-rich foods into your diet, such as whole grains, fruits, vegetables, and legumes. Fiber helps regulate digestion and prevents the formation of gallstones, which can lead to biliary obstruction.
- Reduced Cholesterol Consumption: Limit your intake of cholesterol-rich foods, such as red meat, high-fat dairy products, and fried foods. High cholesterol levels can contribute to the development of gallstones and biliary obstruction.
- Controlled Fat and Sugar Intake: Opt for healthier fats, such as those found in nuts, seeds, and oily fish, while avoiding saturated fats and trans fats. Additionally, limit your consumption of refined sugars and sugary beverages, which can increase the risk of obesity and related complications.
- Maintaining a Healthy Weight: Aim for a healthy body weight through a balanced diet and regular exercise. Being overweight or obese increases the chances of developing gallstones and biliary obstruction.
- Management of Chronic Conditions: If you have conditions such as gallstones, chronic pancreatitis, or pancreatic cancer, it is important to work with your healthcare professional to manage these conditions effectively. Proper management can help reduce the risk of biliary obstruction.
By adopting these preventive measures and making healthy choices, you can significantly reduce the likelihood of developing biliary obstruction. Taking care of your diet, weight, and overall health plays a crucial role in preventing this condition.
Conclusion
Bile duct dysfunction, also known as biliary obstruction, is a condition that can have significant implications if left untreated. It can be caused by various factors such as gallstones, inflammation, trauma, tumors, and liver damage. However, there is hope for individuals facing this condition, as prompt diagnosis, appropriate treatment, and lifestyle modifications can make a substantial difference in managing bile duct dysfunction and preventing complications.
By working closely with healthcare professionals, you can receive the necessary guidance and support to effectively manage bile duct dysfunction. Treatment options may include surgical interventions, medication, and therapeutic procedures like endoscopic retrograde cholangiopancreatography (ERCP). It is essential to address the underlying cause of the obstruction and relieve the blockage to restore the proper function of the bile ducts.
While not all causes of biliary obstruction can be prevented, taking proactive steps in maintaining good overall health can significantly reduce the risk. This includes making dietary changes, such as increasing fiber intake and limiting the consumption of cholesterol, saturated fats, trans fats, and refined sugars. Additionally, managing chronic conditions like gallstones, chronic pancreatitis, and pancreatic cancer is paramount in preventing biliary obstruction.
By prioritizing your health and seeking timely medical attention for any symptoms or risk factors associated with biliary obstruction, you can take control of your well-being. With proper care and management, individuals can lead healthy lives while minimizing the impact of bile duct dysfunction and its potential complications on their overall health and quality of life.
FAQ
What is biliary obstruction?
Biliary obstruction refers to a blockage in the bile ducts, which are tubes that carry bile from the liver and gallbladder to the duodenum. Bile is a fluid produced by the liver to aid in the digestion of fats. The obstruction can occur in the intrahepatic ducts within the liver or the extrahepatic ducts that run towards the small intestine.
What are the causes of biliary obstruction?
Biliary obstruction can be caused by various factors, including gallstones, inflammation of the bile ducts, trauma, biliary strictures, cysts, parasites, enlarged lymph nodes, pancreatitis, gallbladder or liver surgery, tumors in the liver, gallbladder, pancreas, or bile ducts, infections, cirrhosis, severe liver damage, and choledochal cysts.
What are the risk factors for biliary obstruction?
Several risk factors can increase the likelihood of developing biliary obstruction, including a history of gallstones, Caroli disease, chronic pancreatitis, pancreatic cancer, abdominal injury, obesity, rapid weight loss, red blood cell disorders like sickle cell anemia, and certain genetic predispositions.
What are the symptoms and how is biliary obstruction diagnosed?
The symptoms of biliary obstruction can vary but commonly include light-colored stools, dark urine, jaundice, abdominal pain in the upper right side, nausea, vomiting, weight loss, and itching. Diagnosing biliary obstruction requires a thorough physical examination, blood tests to check for liver function and bilirubin levels, and imaging tests like ultrasound, CT scan, MRI, MRCP, and ERCP.
What are the treatment options for biliary obstruction?
The goal of treatment for biliary obstruction is to address the underlying cause and relieve the blockage. Treatment options may include cholecystectomy, endoscopic retrograde cholangiopancreatography (ERCP) to remove stones or place a stent, surgical removal or treatment of tumors, medication to treat infections or parasites, and other therapeutic interventions as necessary.
What are the complications of biliary obstruction?
If left untreated, biliary obstruction can lead to life-threatening complications, including infections, sepsis, chronic liver diseases such as biliary cirrhosis, and the buildup of bilirubin in the bloodstream causing jaundice.
Can biliary obstruction be prevented?
While certain causes of biliary obstruction may not be preventable, making certain lifestyle changes can reduce the risk. Increasing fiber intake, reducing the consumption of cholesterol, saturated fats, trans fats, and refined sugars, maintaining a healthy weight, and managing chronic conditions like gallstones, chronic pancreatitis, and pancreatic cancer can contribute to preventing biliary obstruction.
Source Links


