Suppose you frequently experience heartburn, regurgitation of stomach contents, difficulty swallowing food, or chest pain. In that case, you may be experiencing symptoms of Barrett’s Esophagus.
Table of Contents
ToggleBarrett’s Esophagus is a condition in which acid reflux damages the lining of the Esophagus, leading to changes in the cells and an increased risk of esophageal cancer. These symptoms are often similar to gastroesophageal reflux disease (GERD). It’s essential to seek medical attention if you have these symptoms, especially if they persist for over five years.
Understanding the symptoms of Barrett’s Esophagus is the first step toward diagnosis and effective treatment. This article will delve deeper into the causes, diagnosis, treatment options, and prevention strategies for this condition. By understanding the condition better, you can take proactive steps to manage your health and well-being.
What Causes Barrett’s Esophagus?
The exact cause of Barrett’s Esophagus is not known, but it is commonly associated with long-standing GERD. When the lower esophageal sphincter (LES) fails to function properly, stomach acid and chemicals can flow back into the Esophagus, damaging the lining and triggering the development of Barrett’s Esophagus.
Several factors can increase the risk of developing Barrett’s Esophagus:
- A family history of the condition
- Being male
- Being white
- Having chronic heartburn and acid reflux
- Smoking
- Being overweight
The image above highlights the risk factors associated with Barrett’s esophagus.
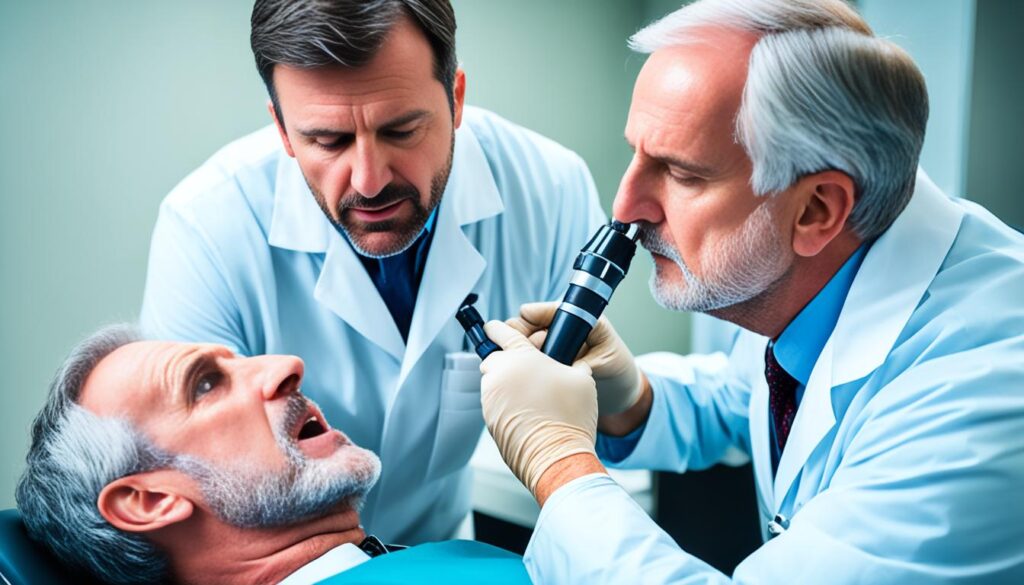
Diagnosing Barrett’s Esophagus
Diagnosing Barrett’s Esophagus requires specific procedures and examinations to assess the condition accurately. The process generally involves an upper endoscopy and biopsy, enabling doctors to examine the esophageal lining and detect any abnormalities or changes. This ensures a precise diagnosis and provides valuable insights into the presence of Barrett’s Esophagus or any precancerous cells, known as dysplasia.
During an upper endoscopy, a flexible tube called an endoscope equipped with a camera is gently inserted into the Esophagus. This technique allows the doctor to carefully examine the esophageal lining for any signs of damage or unusual cell growth. If suspicious areas are identified, a biopsy may be performed. This involves the extraction of a small tissue sample for further analysis in a laboratory, which confirms the presence of Barrett’s Esophagus or identifies any dysplasia.
Additionally, doctors may use a technique known as chromoendoscopy to enhance the detection of abnormal areas in the Esophagus. This procedure involves applying special stains to the esophageal lining, making identifying any changes indicative of Barrett’s Esophagus or precancerous cells easier. Chromoendoscopy can provide a more precise evaluation of the affected areas, helping guide the treatment plan.
Regular checkups and endoscopies are crucial for monitoring the condition and ensuring early detection of any changes in the esophageal lining. This proactive approach allows doctors to intervene promptly and prevent the progression of Barrett’s Esophagus or the development of esophageal cancer. Discuss with your healthcare provider the recommended frequency for checkups and follow-up endoscopies based on your specific condition.
| Diagnosing Barrett’s Esophagus | Procedure |
|---|---|
| Upper Endoscopy | Examination of the esophageal lining using a flexible tube with a camera (endoscope). |
| Biopsy | Extraction of a tissue sample from suspicious areas for laboratory analysis. |
| Chromoendoscopy | Application of specialized stains to enhance the detection of abnormal areas in the esophagus. |
| Regular Checkups | Ongoing monitoring of the condition and early detection of changes. |
Treating Barrett’s Esophagus
The main goal of treating Barrett’s Esophagus is to prevent or slow the condition’s progression. Treatment strategies involve a combination of lifestyle changes and medications to help control acid reflux and reduce the risk of complications. Here are some critical approaches to treating Barrett’s Esophagus:
Lifestyle Changes:
- Avoid trigger foods and beverages that can exacerbate acid reflux.
- Maintain a healthy weight through regular exercise and a balanced diet.
- Quit smoking, as it can worsen symptoms and increase the risk of complications.
- Elevate the head of the bed while sleeping to prevent acid reflux during the night.
- Eat smaller, more frequent meals to reduce the pressure on the lower esophageal sphincter.
- Avoid lying down immediately after meals to allow for proper digestion.
Medications:
Medications can be prescribed to control acid reflux and reduce inflammation. Some common medications for treating Barrett’s Esophagus include:
| Medication | Function |
|---|---|
| Proton Pump Inhibitors (PPIs) | Reduce acid production in the stomach. |
| Antacids | Neutralize stomach acid to provide immediate relief. |
| Histamine 2 (H2) Blockers | Decrease the production of stomach acid. |
| Promotility Agents | Improve the movement of food through the digestive tract. |
Aggressive Treatments:
More intensive treatments may be necessary in low-grade or high-grade dysplasia. The choice of treatment depends on the severity and extent of the condition. Some options include:
- Radiofrequency Ablation: Destroys abnormal cells using heat energy.
- Endoscopic Mucosal Resection: Removes precancerous or early cancerous lesions.
- Endoscopic Spray Cryotherapy: Freezes abnormal cells to eliminate them.
- Surgery: Removes a portion of the Esophagus in more advanced cases.
Regular endoscopies and surveillance are essential for monitoring the progression of Barrett’s Esophagus and detecting any precancerous or cancerous changes. These screenings help ensure early intervention and improve treatment outcomes.

Complications of Barrett’s Esophagus
Barrett’s Esophagus can lead to various complications, including an increased risk of developing esophageal cancer. It is important to note, however, that not everyone with Barrett’s Esophagus will develop cancer.
Regular checkups and surveillance endoscopies are crucial in detecting any precancerous or cancerous changes early. By identifying these changes early on, medical interventions can be implemented to improve the chances of successful treatment.
Other complications that may arise from Barrett’s Esophagus include:
- Difficulty swallowing (dysphagia): The narrowing of the Esophagus due to a damaged lining can make swallowing food or liquids difficult.
- Bleeding: The fragile tissue in the Esophagus may result in bleeding, which can be characterized by blood in the vomit or black, tarry stools.
- Narrowing of the Esophagus (strictures): Repeated injury to the Esophagus can cause scar tissues to develop, leading to narrowing. This can result in difficulty swallowing and discomfort.
Regular monitoring and management of Barrett’s Esophagus are crucial to minimize the complications associated with the condition and improve overall quality of life.
Frequently Asked Questions
- What is the main complication of Barrett’s Esophagus?
- How are precancerous or cancerous changes detected?
- What is dysphagia?
- How can bleeding be recognized?
- What causes the narrowing of the Esophagus in Barrett’s Esophagus?
Barret’s Esophagus and GERD
Barrett’s Esophagus is often associated with gastroesophageal reflux disease (GERD). In fact, long-standing GERD is one of the main risk factors for the development of Barrett’s Esophagus. It is important to manage GERD effectively through lifestyle modifications, dietary changes, and medications to reduce the risk of developing Barrett’s Esophagus and its complications. Treating and controlling GERD can help prevent the progression of Barrett’s Esophagus and reduce the risk of esophageal cancer.
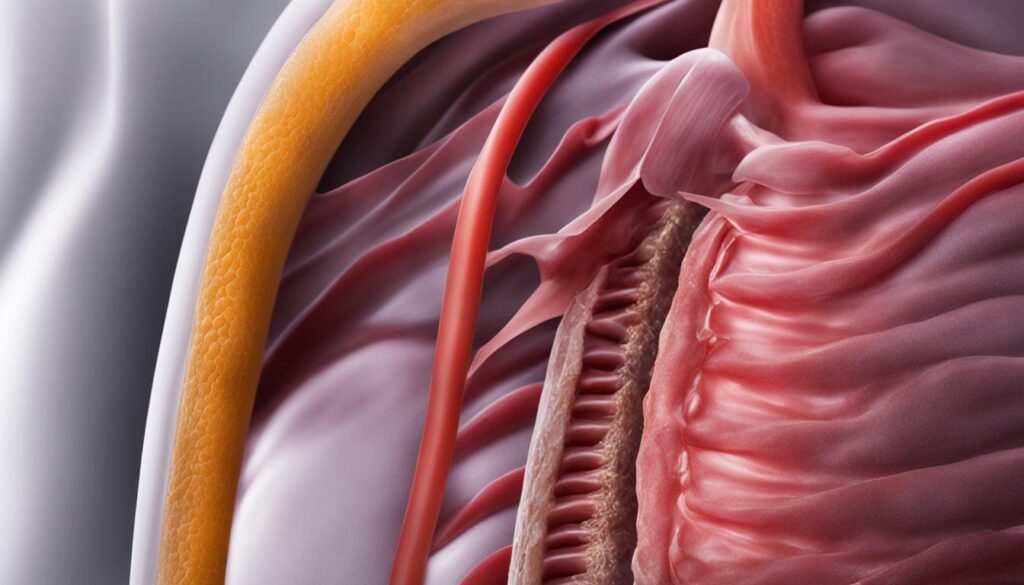
GERD, also known as acid reflux, occurs when stomach acid flows back into the Esophagus, causing symptoms such as heartburn, regurgitation, and chest pain. When left untreated, GERD can damage the lining of the Esophagus over time, leading to the development of Barrett’s Esophagus.
To manage GERD effectively, here are some lifestyle changes that can help:
- Avoid trigger foods and beverages: Certain foods and drinks, such as spicy foods, citrus fruits, and carbonated drinks, can trigger or worsen GERD symptoms. It is important to identify and avoid these triggers to reduce acid reflux.
- Maintain a healthy weight: Excess weight can put pressure on the stomach, leading to a higher risk of acid reflux. Losing weight, if necessary, can help alleviate GERD symptoms.
- Quit smoking: Smoking weakens the lower esophageal sphincter, allowing stomach acid to flow back into the Esophagus. Quitting smoking can improve GERD symptoms and overall health.
- Elevate the head of the bed: Raising the head of the bed by using a wedge pillow or elevating the mattress can help prevent stomach acid from flowing back into the Esophagus while sleeping.
- Eat smaller, more frequent meals: Large meals can increase pressure on the stomach, leading to acid reflux. Eating smaller, more frequent meals can reduce the likelihood of reflux episodes.
- Avoid lying down immediately after meals: Waiting at least two to three hours after eating before lying down can help prevent acid reflux.
In addition to lifestyle changes, medications such as proton pump inhibitors (PPIs), antacids, and H2 blockers may be prescribed to control acid reflux and reduce the risk of developing Barrett’s Esophagus.
By effectively managing GERD, you can alleviate the uncomfortable symptoms and lower the risk of developing Barrett’s Esophagus and its potential complications. Regular monitoring and communication with your healthcare provider are crucial for maintaining optimal digestive health.
Screening and Surveillance of Barrett’s Esophagus
Regular screening and surveillance are essential for individuals at high risk of Barrett’s Esophagus. Suppose you have a long-standing history of GERD or a family history of the condition. In that case, it is essential to prioritize screening to detect any abnormalities early.
Screening for Barrett’s Esophagus usually involves endoscopies and biopsies. During an endoscopy, a flexible tube with a camera is inserted into your Esophagus to examine the lining. If any abnormalities are found, a biopsy may be performed to confirm the presence of Barrett’s Esophagus and check for any precancerous or cancerous changes.
The frequency of surveillance endoscopies depends on your condition’s severity and the presence of dysplasia. Your healthcare provider will determine the appropriate interval for follow-up screenings. Close monitoring through surveillance is crucial for detecting any changes that require treatment.
| Screening and Surveillance Recommendations | |
|---|---|
| High-risk individuals: | Regular screenings using endoscopy and biopsy |
| Endoscopy: | A flexible tube with a camera is inserted into the esophagus |
| Biopsy: | Tissue samples are collected to confirm Barrett’s esophagus and check for changes |
| Surveillance frequency: | Determined by the severity of your condition and the presence of dysplasia |
Regular screening and surveillance play a vital role in managing Barrett’s Esophagus. By detecting and treating abnormalities early, you can reduce the risk of complications and ensure the best possible outcomes for your health.
Lifestyle Changes for Barrett’s Esophagus
Making specific lifestyle changes can help manage symptoms and reduce the risk of complications associated with Barrett’s Esophagus. By incorporating the following habits into your daily routine, you can promote healing and prevent the progression of the condition:
- Avoid trigger foods and beverages: Certain foods and drinks can trigger acid reflux, worsening the symptoms of Barrett’s Esophagus. Spicy, fatty, and acidic foods, as well as caffeine and alcohol, should be limited or avoided.
- Maintain a healthy weight: Excess weight can put pressure on the stomach, leading to increased reflux and irritation of the Esophagus. Maintaining a healthy weight through regular exercise and a balanced diet can reduce the strain on your digestive system.
- Quit smoking: Smoking is a known risk factor for Barrett’s Esophagus and can worsen reflux symptoms. Quitting smoking benefits your overall health and helps protect the lining of your Esophagus.
- Elevate the head of the bed while sleeping: Raising the head of your bed by using a wedge-shaped pillow or elevating the mattress can help prevent the backflow of stomach acid into the Esophagus, reducing nighttime symptoms.
- Eat smaller, more frequent meals: Large meals can put additional pressure on the stomach, increasing the likelihood of acid reflux. Opt for smaller, more frequent meals to minimize discomfort and manage symptoms effectively.
- Avoid lying down immediately after meals: Give your body time to digest food properly by avoiding lying down immediately after meals. Standing or sitting upright for at least 2-3 hours after eating can help prevent acid reflux and minimize irritation in the Esophagus.
By incorporating these lifestyle changes, you can actively manage Barrett’s Esophagus and promote your overall well-being.
Support and Resources for Barrett’s Esophagus
Living with Barrett’s Esophagus can be challenging, but you don’t have to face it alone. Resources are available to provide you with the support and information you need to navigate this condition.
Support Groups and Online Communities
Joining a support group or online community can connect you with others who understand what you’re going through. These communities provide a safe space to share experiences, ask questions, and receive emotional support from people who can relate. Here are some recommended support groups and online communities for Barrett’s Esophagus:
- Barrett’s Esophagus Support Group: A community of individuals with Barrett’s Esophagus sharing their stories, tips, and advice.
- Reddit Barrett’s Esophagus Forum is an online forum where you can exchange information and support with others who have the condition.
- Facebook Barrett’s Esophagus Support Group: A closed Facebook group where you can connect with people going through similar experiences.
Educational Materials
Educational materials can help you better understand Barrett’s Esophagus and its management. These resources provide valuable information, tips, and guidance on coping with the diagnosis and managing the symptoms. Here are some recommended educational materials:
- “Living with Barrett’s Esophagus: A Comprehensive Guide”: A book written by leading experts in the field, offering in-depth information on Barrett’s Esophagus and its treatment options.
- Brochures and pamphlets: Available at gastroenterology clinics and healthcare facilities, these materials provide concise information on the condition and its management.
- Online resources: Websites like the American College of Gastroenterology and the Mayo Clinic offer comprehensive information on Barrett’s Esophagus, including treatment options and lifestyle recommendations.
Working with Healthcare Professionals
Collaborating with healthcare professionals is crucial in managing and treating Barrett’s Esophagus. Gastroenterologists and nutritionists can offer personalized advice, develop a tailored treatment plan, and address any concerns or questions you may have. They will guide you through your journey and provide the necessary guidance and medical interventions to help you manage your condition effectively.
Remember, the support and resources available for Barrett’s Esophagus can make a significant difference in your journey. By reaching out to others, accessing educational materials, and working closely with healthcare professionals, you can receive the support and information needed to manage your condition and improve your quality of life effectively.
Prevention of Barrett’s Esophagus
While it may not be possible to completely prevent Barrett’s Esophagus, certain measures can reduce the risk. By managing GERD effectively and adopting a healthy lifestyle, you can minimize the chances of developing Barrett’s Esophagus and its potential complications.
Lifestyle Changes
Making lifestyle modifications can play a vital role in preventing Barrett’s Esophagus. Here are some steps you can take:
- Avoid trigger foods and beverages that can exacerbate acid reflux.
- Maintain a healthy weight through regular exercise and a balanced diet.
- Quit smoking to reduce the risk of acid reflux and damage to the esophageal lining.
- Avoid excessive alcohol consumption, as it can contribute to acid reflux.
- Elevate the head of your bed while sleeping to prevent stomach acid from flowing back into the Esophagus.
- Eat smaller, more frequent meals to reduce the pressure on the lower esophageal sphincter.
- Avoid lying down immediately after meals to allow time for digestion.
Medical Intervention
Seeking medical attention for persistent reflux symptoms is essential for preventing the development of Barrett’s Esophagus. Effective management of GERD through medications and other interventions can significantly reduce the risk. If you experience symptoms such as frequent heartburn, regurgitation of stomach contents, difficulty swallowing, or chest pain, consult a healthcare professional for evaluation and appropriate treatment.
| Prevention Measures | Description |
|---|---|
| Lifestyle Changes | Adopting healthy habits such as avoiding trigger foods, maintaining a healthy weight, quitting smoking, and elevating the head of the bed can help reduce the risk of Barrett’s esophagus. |
| Medical Intervention | Seeking medical attention for persistent reflux symptoms and effectively managing GERD through medications and other interventions can help prevent the development of Barrett’s esophagus. |
Conclusion
Barrett’s Esophagus is a condition that affects the lining of the Esophagus, increasing the risk of esophageal cancer. This condition is often associated with long-standing gastroesophageal reflux disease (GERD). Regular checkups, endoscopies, and surveillance are crucial to monitor the condition and identify any abnormalities.
Managing Barrett’s Esophagus involves lifestyle changes, medications, and potentially more aggressive treatments. By making necessary lifestyle modifications and taking prescribed medications, you can effectively minimize the symptoms and reduce the risk of complications. If needed, your doctor may recommend more advanced treatments.
Understanding the symptoms, causes, diagnosis, and treatment options for Barrett’s Esophagus empowers you to proactively manage the condition and safeguard your overall health and well-being. Remember to follow your healthcare provider’s recommendations, maintain a healthy lifestyle, and seek support from resources available to assist individuals living with Barrett’s Esophagus.
FAQ
What are the symptoms of Barrett’s Esophagus?
The symptoms of Barrett’s Esophagus are often similar to those of gastroesophageal reflux disease (GERD). They may include frequent heartburn, regurgitation of stomach contents, difficulty swallowing food, and chest pain. It is essential to seek medical attention if you experience these symptoms, especially if they persist for over five years.
What causes Barrett’s Esophagus?
The exact cause of Barrett’s Esophagus is not known, but it is commonly associated with long-standing GERD. When the lower esophageal sphincter (LES) fails to function properly, stomach acid and chemicals can flow back into the Esophagus, causing damage to the lining and triggering the development of Barrett’s Esophagus. Other risk factors include:
- A family history of the condition.
- Being male.
- Being white.
- Having chronic heartburn and acid reflux.
Smoking and being overweight can also increase the risk.
How is Barrett’s Esophagus diagnosed?
Barrett’s Esophagus is typically diagnosed through an upper endoscopy and biopsy. During this procedure, a doctor examines the lining of the Esophagus using a flexible tube with a camera (endoscope). If abnormalities are detected, a biopsy may be performed to confirm the presence of Barrett’s Esophagus and to check for any precancerous cells (dysplasia). Chromoendoscopy, which involves applying stains to the Esophagus, may also be used to identify abnormal areas. Regular checkups and endoscopies are recommended to monitor the condition.
How is Barrett’s Esophagus treated?
The main goal of treating Barrett’s Esophagus is to prevent or slow the condition’s progression. This can be achieved through lifestyle changes and medications to control acid reflux. These may include proton pump inhibitors (PPIs), antacids, histamine 2 (H2) blockers, and promotility agents. In low-grade or high-grade dysplasia cases, more aggressive treatments such as radiofrequency ablation, endoscopic mucosal resection, endoscopic spray cryotherapy, or surgery may be considered. Regular endoscopies and surveillance are essential to monitor the condition’s progression and detect any precancerous or cancerous changes.
What are the complications of Barrett’s Esophagus?
The main complication of Barrett’s Esophagus is an increased risk of developing esophageal cancer. However, it is essential to note that most people with Barrett’s Esophagus never develop cancer. Regular checkups and surveillance endoscopies are crucial for detecting precancerous or cancerous changes early when they are more treatable. Other complications of Barrett’s Esophagus may include difficulty swallowing (dysphagia), bleeding, and narrowing of the Esophagus (strictures).
How is Barrett’s Esophagus related to GERD?
Barrett’s Esophagus is often associated with gastroesophageal reflux disease (GERD). In fact, long-standing GERD is one of the main risk factors for the development of Barrett’s Esophagus. It is essential to manage GERD effectively through lifestyle modifications, dietary changes, and medications to reduce the risk of developing Barrett’s Esophagus and its complications. Treating and controlling GERD can help prevent the progression of Barrett’s Esophagus and reduce the risk of esophageal cancer.
How often should screening and surveillance be done for Barrett’s Esophagus?
Regular screening and surveillance are recommended for individuals at high risk of Barrett’s Esophagus, such as those with long-standing GERD or a family history of the condition. Screening may involve endoscopies and biopsies to check for the presence of Barrett’s Esophagus and any precancerous or cancerous changes. The frequency of surveillance endoscopies depends on the severity of the condition and the presence of dysplasia. Close monitoring is essential to detect and treat any abnormalities early.
What lifestyle changes can help manage Barrett’s Esophagus?
Making specific lifestyle changes can help manage symptoms and reduce the risk of complications associated with Barrett’s Esophagus. These may include avoiding trigger foods and beverages, maintaining a healthy weight, quitting smoking, elevating the head of the bed while sleeping, eating smaller, more frequent meals, and avoiding lying down immediately after meals. These changes can help reduce acid reflux and minimize the damage to the esophageal lining, promoting healing and preventing the progression of Barrett’s Esophagus.
What support and resources are available for Barrett’s Esophagus?
Living with Barrett’s Esophagus can be challenging, but there are resources available to support individuals with the condition. Support groups, online communities, and educational materials can provide valuable information, tips, and emotional support to cope with the diagnosis and manage symptoms. Working closely with healthcare professionals, including gastroenterologists and nutritionists, is essential to develop a personalized treatment plan and address any concerns or questions.
Can Barrett’s Esophagus be prevented?
While entirely preventing Barrett’s Esophagus may not be possible, specific measures can help reduce the risk. These include managing GERD effectively through lifestyle changes and medications, maintaining a healthy weight, avoiding smoking and excessive alcohol consumption, and seeking medical attention for persistent reflux symptoms. Early detection and treatment of GERD can help prevent the development of Barrett’s Esophagus and its potential complications.
Source Links


