Stress causes acid reflux by changing how your gut moves and how your muscles behave. Stress can turn up how strongly you feel acid in your food pipe (esophagus). Acute stress did not always raise measured acid, but it often made heartburn feel worse. That points to stress changing pain sensing, not just acid level.
Table of Contents
ToggleWhen you feel stressed, your body flips into a “fight or flight” state. Your brain signals your gut through nerves and stress hormones. Stress can cause acid reflux, but it may not mean you suddenly “make tons of acid.” It can mean your system becomes easier to trigger and harder to calm.
Can Anxiety Cause Acid Reflux
Many people notice reflux during worry, panic, or long, anxious weeks. The link is not just “in your head.” Anxiety can change body signals, muscle function, and symptom awareness. Anxiety causes acid reflux more often by changing how your body reacts to normal acid and pressure.
How Anxiety Affects Stomach Acid Production
When anxiety hits, your nervous system shifts blood flow and attention away from digestion. Your body uses the stress pathways called the HPA axis and SAM axis (your hormone and adrenaline systems).
In some people, stomach acid-related symptoms rise during anxiety. However, a key driver can be “increased perception.” That means your brain reads the same gut signal as more painful.
Anxiety does not always increase acid production. Results vary by person and by study method. Even so, stress-caused acid reflux can still happen through sensitivity changes alone.
Anxiety-Related Muscle Tension And LES Dysfunction
Your lower esophageal sphincter, or LES (the “valve” between the food pipe and stomach), should stay closed. If it relaxes at the wrong time, reflux gets easier.
Anxiety can change breathing and muscle tension. Tight belly muscles and shallow chest breathing can raise pressure in your abdomen. More pressure can push stomach contents upward, especially after meals.
There is also a behavior that rises in stress: frequent air swallowing and “supragastric belching” (air moving in and out of the food pipe). This can stretch the area and trigger reflux events soon after.
Why Reflux Symptoms Worsen During Panic Or Worry
Panic pushes your body into high alert. Your brain scans your chest and throat for danger. That can make normal sensations feel scary and intense.
Stress has also been shown to increase sensitivity to acid in the esophagus in GERD-related conditions. In other words, the same acid exposure can hurt more during stress.
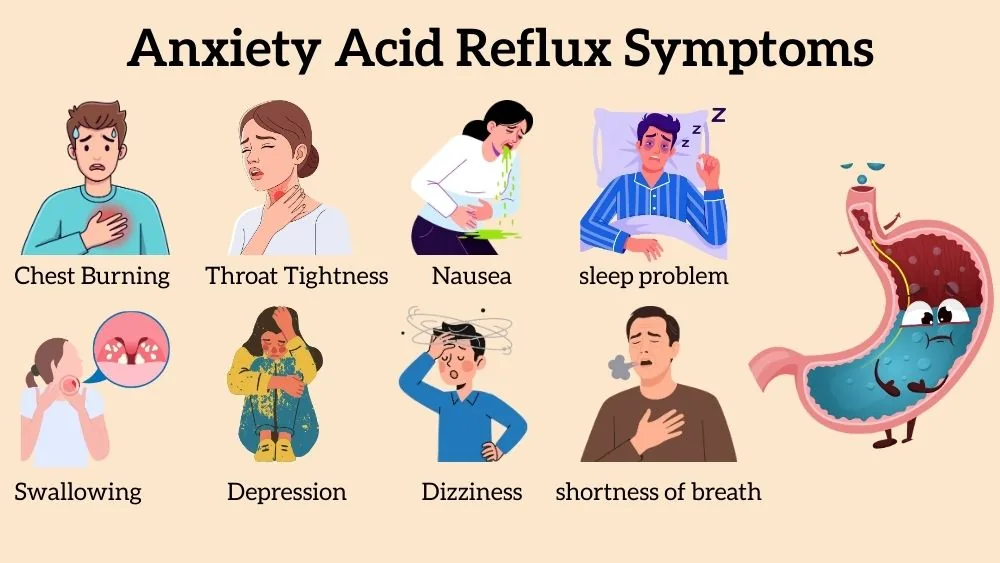
Anxiety Acid Reflux Symptoms
Stress-linked reflux symptoms can look like classic heartburn. They can also feel “throat-heavy,” “chest-tight,” or “hard to swallow.” Some of this comes from acid irritation. Some comes from stress-driven muscle tension and sensitivity.
Chest Burning And Throat Tightness
You may feel burning behind your breastbone. You may feel it after eating or when lying down. Those are common GERD patterns.
Stress can add throat tightness. It can make you notice every swallow. It can make the burn feel sharper. If chest pain feels new, heavy, or comes with sweating, get urgent care. Do not guess.
Still, on many ordinary days, stress causes acid reflux explains why symptoms spike without a big diet change.
Globus Sensation And Difficulty Swallowing
Globus sensation means you feel a lump in your throat. You may keep clearing your throat. You may feel like swallowing takes effort. Lump in the throat and trouble swallowing are possible reflux-related symptoms.
Stress can tighten throat muscles. Reflux can irritate the throat lining. Together, you can feel stuck, even when food passes fine. This is one reason stress-caused acid reflux often shows up as throat discomfort, not just heartburn.
Nausea, Bloating, And Sour Taste During Stress
Stress can shift gut movement. For some people, it slows stomach emptying. When food sits longer, you can feel full, bloated, or nauseated.
A sour or bitter taste can happen when stomach contents move upward. “Backwash of sour liquid” is a classic reflux sign. When your week feels tense, stress-caused acid reflux can show up as bloating plus throat taste, not just heartburn.
GERD Flare Ups Due To Stress
If you already have GERD , stress can make it feel louder and more frequent. People often describe sudden flares during exams, job stress, grief, or conflict. GERD flare-ups due to stress relate strongly to symptom severity, even when acid measurements do not always change.
Why Stress Triggers Sudden GERD Flare-Ups
Stress changes your routine fast. You may eat faster. You may snack late. You may drink more caffeine. You may lie down soon after dinner. These patterns can raise reflux risk.
But there is also a less obvious reason. Acute stress can “turn up the volume” on your esophagus. A stressor can make you feel stronger heartburn from the same acid exposure. So GERD flare-ups due to stress can be a mix of habits and sensitivity.
Stress Hormones And Delayed Gastric Emptying
Gastric emptying means how fast your stomach sends food into the small intestine. When emptying slows, the stomach stays fuller longer. Pressure rises, and reflux becomes easier.
Human and animal research shows certain stressors can delay gastric emptying and change gut movement after meals. Not every type of stress slows emptying in every person. Your body’s response depends on stress type, duration, and your baseline gut function.
Even so, this is a strong pathway for why stress-caused acid reflux can worsen after stressful days.
Acute Vs Chronic Stress Impact On GERD
Acute stress is short-term and often causes short symptom spikes.
Chronic stress lasts weeks or months. It can disturb sleep, raise muscle tension, and keep the stress system activated. Over time, that can push you toward more frequent symptoms and more sensitivity. This is why stress-caused acid reflux can feel occasional for one person and daily for another.
How Stress Worsens Acid Reflux
Stress can shift digestion, raise sensitivity, and change behaviors that trigger reflux. This is why stress-caused acid reflux can feel so consistent in your life.
Cortisol Effects On Digestion And Acid Secretion
Cortisol is a stress hormone and helps you stay alert. It also changes digestion timing. Under stress, your body can send less blood to the stomach. That can shift how your stomach contracts after meals. It can also change how fast your stomach empties.
Stress does not always increase acid exposure in the esophagus. Yet it can still raise symptoms. That happens because stress can increase esophageal sensitivity (your food pipe feels pain faster). Doctors describe this pattern in reflux hypersensitivity (acid feels stronger than expected).
Stress-Related Changes In Gut Motility
Motility means movement. It is how your gut pushes food forward. Stress can slow down your stomach in some people. It can also cause more bloating. When the stomach stays full, pressure rises. That pressure can push stomach contents up.
Stress can also increase belching patterns. One type is supragastric belching (air pulls into the food pipe, then pushes out). That extra air can trigger reflux episodes. Breathing training can reduce belching and reflux symptoms in certain patients.
Poor Sleep, Stress Eating, And Reflux Cycles
Sleep loss makes stress worse. Stress makes sleep worse. Then reflux joins the loop. Late meals matter too. When you eat close to bedtime, you lie down with a fuller stomach. Acid can move upward more easily.
Avoiding late meals and raising the head of your bed when night symptoms hit are recommended. These steps lower acid exposure during sleep.
Stress nudges you into habits that trigger reflux. Then, reflux ruins sleep, and the next day feels harder. In real life, stress causes acid reflux often lives inside this cycle.
Emotional Stress And GERD
Emotional stress includes grief, anger, conflict, and burnout. These feelings can hit your gut fast. You may notice heartburn after arguments. You may notice throat symptoms during sadness.
For many people, stress-caused acid reflux feels strongest during emotional overload.
Relationship Between Emotional Distress And Heartburn
When you feel distressed, your breathing often changes. You may take short breaths. You may hold your belly tight. That raises belly pressure. It can push reflux upward.
Emotional stress can also turn up pain signals. In reflux hypersensitivity, symptom severity can rise even when tests show limited acid.
So you can feel heartburn that seems “too big” for the meal you ate. This can make stress-caused acid reflux feel confusing, but it has a real body basis.
Depression, Anxiety Disorders, And GERD Overlap
Anxiety and depression often appear alongside reflux. The overlap can happen for several reasons. Poor sleep can worsen both. Some people eat differently during a low mood, while others become less active. These shifts can increase reflux risk.
Also, brain–gut disorders like functional heartburn can mimic GERD. Functional heartburn means you feel burning, but acid tests look normal. It is linked to sensitivity and stress pathways. If you keep thinking anxiety causes acid reflux , this overlap explains why the pattern feels common.
Brain–Gut Axis Role In Chronic Reflux
Your brain and gut connect through nerves and hormones. Stress can keep that system “on.” Over time, your esophagus may react more strongly to small triggers.
Doctors now describe reflux hypersensitivity as a condition where reflux events cause symptoms even when acid exposure stays normal. That is a brain–gut axis issue, not “weakness.” This helps explain why stress-caused acid reflux can continue, even after your schedule calms down.
How To Reduce Stress-Related Acid Reflux
You need a two-part plan. You calm the stress system. You reduce reflux triggers. When you do both, stress-caused acid reflux often becomes less frequent.
Stress Management Techniques That Reduce Reflux
Start with simple routines you can repeat. Take short walks after meals if you can. Light movement helps digestion and reduces stress tension.
Keep meals steady. Skipping meals can backfire. It can lead to large late meals. Large meals increase stomach pressure. That pressure feeds reflux.
If your symptoms spike during hard weeks, label it clearly. GERD flare-ups due to stress often improve when your daily rhythm becomes predictable again.
Mindfulness, Breathing, And Relaxation Strategies
Breathing training has real research behind it. Diaphragmatic breathing means belly breathing. It trains your breathing muscle under the lungs. In a study, post-meal diaphragmatic breathing reduced post-meal reflux events compared with quiet sitting.
Not every study shows big changes in acid exposure. Some show symptom improvement more than acid changes.
Sit upright and put one hand on your belly. Breathe in through your nose. Let your belly rise. Breathe out slowly. Keep shoulders relaxed. Do this after meals for a few minutes.
This can help when stress worsens acid reflux through tension and air swallowing.
Lifestyle Habits That Calm Both Mind And Stomach
Night reflux needs special care. Experts suggest head-of-bed elevation for nighttime symptoms. Sleeping on your left side may also reduce nighttime reflux in some people.
Eat earlier when possible. Avoid lying down soon after eating. Tailor food triggers to your body. Some people react to mint, chocolate, fatty meals, or acidic foods. You do not need a strict list. You need a personal pattern.
If you calm your evenings, stress-caused acid reflux often becomes easier to manage.
When Stress Is Not The Only Cause Of Acid Reflux
Stress matters. But it is not the only reason reflux happens. Some people have true GERD with tissue injury. Some have a hiatal hernia (part of the stomach moves upward). Some have esophagitis (an inflamed food pipe).
Warning Signs Of Underlying GERD Or Esophagitis
Get medical help right away if you have chest pain with shortness of breath or pain that spreads to the jaw or arm.
Also take “alarm symptoms” seriously. These include trouble swallowing that worsens, vomiting blood, black stools, or unplanned weight loss. These signs need evaluation.
If symptoms happen often, they can lead to complications like Barrett’s esophagus (cell changes in the food pipe). That is why repeated reflux deserves attention.
When To Consider Medical Treatment
If you use over-the-counter heartburn medicine more than twice a week, it is time to talk with a clinician. Doctors usually prescribe acid-lowering medicines when symptoms are frequent or when there is inflammation. Dosage varies by age and condition. Some people also need testing, like an endoscopy (a camera exam), based on symptoms and risk.
Combining Stress Control With Reflux Therapy
When symptoms come from both reflux and sensitivity, you often need both approaches. Reflux care reduces acid exposure. Stress care reduces sensitivity and habit triggers.
Behavioral therapies can help some people with functional heartburn and reflux hypersensitivity. This combined plan fits the reality that GERD flare-ups due to stress can happen even when you “eat perfectly.”
FAQs
Can Stress Alone Cause Acid Reflux Without GERD?
Yes. Stress-caused acid reflux can happen even without long-term GERD. Stress can raise esophageal sensitivity and belly pressure. Symptoms often follow stressful events, then ease when your nervous system settles.
How Do I Know If My Reflux Is Anxiety-Related?
Look at timing and body clues. If symptoms spike during worry, racing thoughts, or panic sensations, anxiety-caused acid reflux may fit. You may also notice throat tightness and frequent air swallowing during stress.
Can Stress Cause Acid Reflux Every Day?
It can. If stress stays high, sleep and eating habits often change. That can keep symptoms going. In that pattern, stress causes acid reflux to become daily through tension, late meals, and stronger symptom sensitivity.
Does Treating Anxiety Reduce GERD Symptoms?
Often, yes. Lower anxiety can reduce muscle tension, air swallowing, and symptom focus. It also improves sleep. For many people, stress worsens acid reflux less when anxiety treatment and reflux care work together.
Can Emotional Stress Cause Throat Burning?
Yes. Emotional stress can tighten throat muscles and increase sensitivity. Reflux can also reach the throat and irritate it. If throat-burning tracks with hard emotions, stress-caused acid reflux may explain the pattern.
Are Stress-Induced Reflux Symptoms Dangerous?
Most are not dangerous right away. But frequent reflux can inflame the food pipe over time. If symptoms persist, get evaluated. Stress-caused acid reflux can still lead you to real GERD that needs treatment.
What’s The Fastest Way To Calm Stress-Related Heartburn?
Sit upright, loosen tight clothing, and breathe slowly. Diaphragmatic breathing may reduce post-meal reflux events for some people. If symptoms repeat, treat GERD flare-ups due to stress with both habit and stress control.
Can Therapy Help Acid Reflux Caused By Stress?
Yes. For reflux hypersensitivity and functional heartburn, therapy methods like CBT can help some people by changing stress response and symptom focus. This supports why stress-caused acid reflux can improve with mind–gut care.
About The Author

This article is medically reviewed by Dr. Nivedita Pandey, Senior Gastroenterologist and Hepatologist, ensuring accurate and reliable health information.
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist specializing in pre and post-liver transplant care, as well as managing chronic gastrointestinal disorders. Known for her compassionate and patient-centered approach, Dr. Pandey is dedicated to delivering the highest quality of care to each patient.
→ Book a consultation to discover which remedies suit your needs best.
About Author | Instagram | Linkedin