What is gut microbiota?
Microbiota is the community of trillions of bacteria, fungi, and other microbes that live in your digestive tract. These tiny organisms are not just passive passengers, they actively help your body in multiple ways.
Table of Contents
ToggleThe gut microbiota breaks down food into nutrients, supports your immune system, and produces compounds like short-chain fatty acids that keep your gut lining healthy. It surprisingly contributes to the regulation of hormones and metabolic processes.
When the gut microbiome is in equilibrium, it assists the body in maintaining consistent energy levels, regular menstrual cycles, and stable emotional states. But in Polycystic Ovary Syndrome (PCOS), this balance often shifts, a condition known as Gut dysbiosis in PCOS.
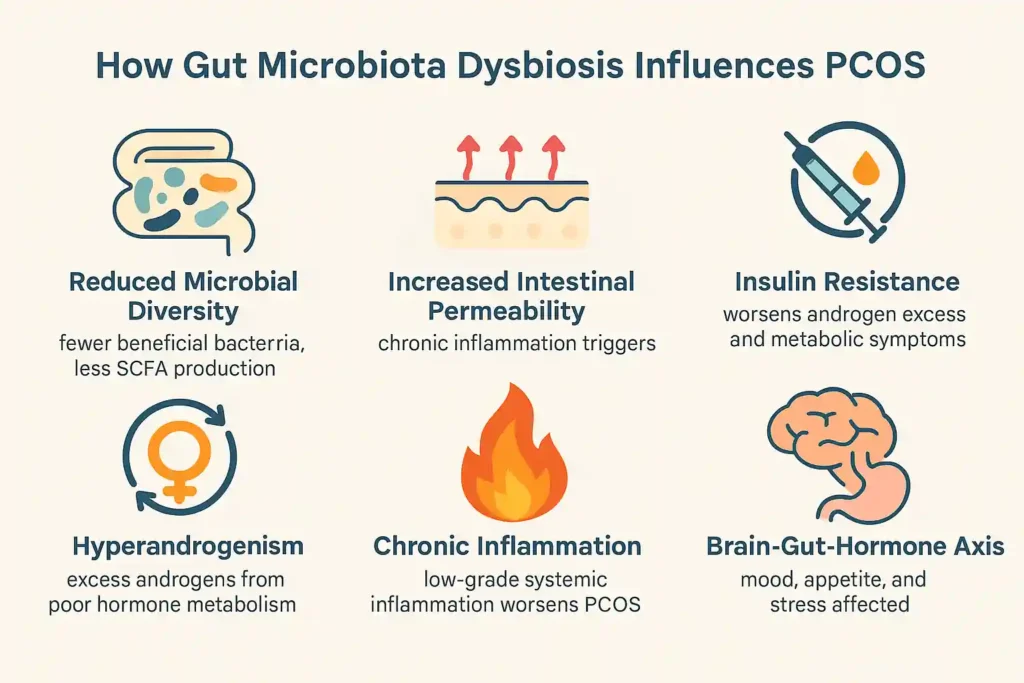
This imbalance can weaken your gut barrier, increase intestinal permeability, and cause chronic inflammation. Over time, it affects estrogen metabolism, fuels androgen excess, and worsens insulin resistance, all key features of what is PCOS.
Scientists describe this connection as the Microbiota-PCOS axis. It means your gut microbes and reproductive hormones are in constant communication. When your gut is unhealthy, the whole system suffers, deepening the cycle of pcos and gut microbiome disruption.
Changes of gut microbiota composition in PCOS
Women with Polycystic Ovary Syndrome often show a different gut bacteria makeup compared to women without PCOS. Studies suggest that gut dysbiosis in PCOS means fewer good bacteria and more harmful ones.
Common changes include:
- Lower diversity of gut bacteria.
- A reduction in beneficial microbes that generate short-chain fatty acids (SCFAs), which are essential for gut health.
- More bacteria are linked to intestinal permeability, which can trigger inflammation.
This imbalance is not just a gut problem, it’s tied to hormone changes, insulin resistance, and weight gain. In fact, many women with PCOS also have signs of metabolic syndrome.
Gut microbiota and the pathological mechanism of PCOS

The link between PCOS and gut microbiota is part of what experts call the Microbiota-PCOS axis. This means changes in the gut microbiome can trigger or worsen the main problems in PCOS: hormone imbalance, high androgens, and irregular ovulation.
Poor gut health can:
- Disrupt estrogen metabolism, leading to irregular cycles.
- Promote androgen excess, which causes acne, hair growth, and scalp hair loss.
- Increase inflammation and oxidative stress, making symptoms worse.
Scientists believe that fixing the gut imbalance could help manage the root causes of PCOS, not just the symptoms.
Gut microbiota and insulin resistance
Insulin resistance, when your body struggles to use insulin properly is common in PCOS. Poor gut health makes this worse. Harmful gut bacteria can release toxins that enter the bloodstream, cause gut inflammation in PCOS, and interfere with insulin signaling.
This sets off a chain reaction: high insulin levels boost androgen excess, which then worsens PCOS symptoms. Improving the gut microbiome PCOS connection may lower insulin resistance and help with weight control.
Gut microbiota and hyperandrogenism
High androgen levels are a hallmark of what is PCOS. The gut plays a surprising role here. When the gut microbiota is unbalanced, the liver can’t process hormones properly. This allows more active androgens to circulate.
An unbalanced gut may also affect the gut-brain-hormone axis, influencing hormone production directly. Restoring gut balance could therefore help reduce excess hair growth, acne, and menstrual issues caused by pcos and gut microbiota interaction.
Gut microbiota and chronic inflammation
Many women with PCOS have low-grade chronic inflammation. Gut imbalance often increases intestinal permeability, allowing harmful particles to leak into the bloodstream. This triggers the immune system and worsens inflammation.
Inflammation fuels PCOS metabolic mechanisms and can worsen oxidative stress PCOS gut microbiome issues, leading to even more hormone disruption.
Brain-gut axis and PCOS
The brain-gut-hormone axis is like a communication highway between your brain, gut, and hormones. In PCOS, this link can be disturbed. Stress and anxiety can alter gut bacteria. In turn, unhealthy gut bacteria can affect mood and appetite.
This is why PCOS isn’t just about ovaries, it’s a full-body condition where mental health and gut health are closely connected.
Treatment of PCOS based on gut microbiome
Researchers are now looking at PCOS microbiota interventions that target the gut directly. These may not be “quick fixes,” but they aim to correct the root imbalance.
Fecal microbiota transplantation
Fecal microbiota transplantation (FMT) involves transferring healthy gut bacteria from a donor to the patient. Early studies suggest it may help restore healthy bacteria in pcos and gut microbiome cases, improve insulin sensitivity, and lower inflammation.
Herbal medicine
Some herbs, like berberine and licorice root, have been studied for their ability to support microbiome modulation. They may improve gut diversity and reduce oxidative stress PCOS gut microbiome issues.
Probiotics and prebiotics
Prebiotics and probiotics can feed and add beneficial bacteria to the gut. Certain probiotic strains have shown promise in improving insulin sensitivity, lowering inflammation, and balancing hormones in gut microbiome and PCOS patients.
Other drugs
Some diabetes medications, like metformin, also seem to improve gut bacteria diversity. This could explain part of their benefit in PCOS and insulin resistance cases.
The Bottom Line
PCOS and gut microbiota are more connected than most people realize. Gut imbalance can influence hormones, weight, metabolism, and inflammation. Addressing the gut microbiome PCOS link may be one of the most powerful ways to manage symptoms and improve health long term.
Frequently asked questions
What is the connection between gut microbiota and PCOS?
An unhealthy gut microbiota affects hormones, metabolism, and inflammation. This imbalance known as the Microbiota-PCOS axis can make Polycystic Ovary Syndrome symptoms worse and harder to manage long term.
How does gut dysbiosis contribute to PCOS symptoms?
Gut dysbiosis in PCOS triggers inflammation, disrupts estrogen metabolism, worsens insulin resistance, and fuels androgen excess, all of which drive irregular cycles, weight gain, acne, and other PCOS-related symptoms.
Can improving gut health help manage PCOS?
Yes. Balancing the gut microbiome pcos link through diet, prebiotics and probiotics, and lifestyle changes can improve hormones, lower inflammation, and support better metabolic health in pcos and gut microbiota cases.
Can gut issues cause PCOS?
While gut problems alone don’t cause PCOS, poor gut microbiota and pcos balance can worsen hormone issues, increase oxidative stress PCOS gut microbiome, and contribute to Metabolic syndrome PCOS gut symptoms.
Why did I suddenly develop PCOS?
PCOS metabolic mechanisms involve genetics, environment, and lifestyle. Gut imbalance, stress, weight gain, and diet shifts can interact with these factors, making pcos symptoms appear suddenly or worsen over time.
Does gut health affect hormone balance in PCOS?
Absolutely. A healthy gut microbiome and PCOS connection supports estrogen metabolism, keeps androgens in check, and reduces gut inflammation in PCOS, which can improve menstrual regularity and fertility outcomes.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin