Bile reflux happens when bile flows backward into your stomach and food pipe. Bile is a yellow-green digestive liquid made by your liver. It normally helps break down fats in the small intestine. When the flow goes the wrong way, bile irritates delicate tissue. Bile reflux often causes deep burning pain, bitter vomiting, and long-term damage if ignored. Many people suffer for years because the condition gets misread.
Table of Contents
ToggleCauses of Bile Reflux
Bile reflux develops when the normal one-way movement of bile breaks down. Structural damage, nerve problems, or surgical changes allow bile to push backward into the stomach. Over time, repeated exposure injures the stomach lining and disrupts digestion.
Gallbladder Surgery
Gallbladder removal changes bile timing and control. Bile no longer gets stored. It drips into the intestine all day. This steady flow raises pressure. Bile then moves backward into the stomach. Many people develop bile reflux months after surgery. Symptoms often worsen after fatty meals.
Stomach Surgery
Stomach surgery can damage protective valves. These valves keep bile moving forward. Operations for ulcers or tumors often weaken them. Once damaged, bile flows freely into the stomach. This backward flow raises the risk of chronic bile reflux .
Peptic Ulcers
Peptic ulcers are open sores in the stomach or intestine. Swelling from ulcers can block the pyloric valve. This valve controls food exit. When blocked, bile builds up. Pressure pushes bile upward. This process triggers bile reflux symptoms.
Pyloric Valve Dysfunction
The pyloric valve sits between the stomach and the small intestine. It opens and closes during digestion. Injury, surgery, or long-term inflammation can weaken it. A weak valve cannot stop bile backflow. Valve failure is a major cause among people with severe bile reflux .
Motility Disorders
Motility means movement. The stomach must empty on time. Nerve damage slows this movement. Diabetes and nerve disorders often cause this delay. Slow emptying lets bile stay longer. Pressure increases. Bile then flows backward. This mechanism explains many stubborn bile reflux cases.
Chronic Gastritis
Chronic gastritis means long-term stomach lining. Bile irritates the lining further. The lining loses its protective mucus layer. This damage makes the bile injury worse. Gastritis and bile reflux often exist together and feed each other.
Bile Flow Abnormalities
Some bodies produce excess bile. Others fail to control release timing. Both raise reflux risk. These patterns often appear after surgery. Abnormal bile flow explains why some people develop bile reflux without acid problems.
Symptoms of Bile Reflux
The symptoms of bile reflux often feel stronger and more persistent than acid reflux. They usually do not improve with common antacids. Many symptoms worsen at night or after fatty meals because bile flow increases during digestion.
Upper Abdominal Pain
Pain sits in the upper stomach. It feels sharp, burning, or gnawing. Eating often triggers it. Pain may last for hours. This pain pattern strongly suggests bile reflux .
Burning Sensation in the Chest or Stomach
This burn feels deep and raw. Antacids rarely help. The burn may spread upward. Many mistake this for acid reflux. The difference matters because bile reflux needs different treatment.
Bitter or Yellow-Green Vomiting
Bile tastes bitter and harsh. Vomit may look yellow or green. This sign is very specific. It strongly points to bile reflux , not simple indigestion.
Nausea
Nausea often lasts all day. It worsens after meals. You may avoid food. Long-term nausea leads to weakness. This symptom is common in advanced bile reflux .
Chronic Cough or Hoarseness
Bile irritates the throat. This causes cough and voice changes. Symptoms worsen when lying flat. Many people visit lung doctors first. The real cause often remains bile reflux .
Unintentional Weight Loss
Pain reduces eating. Poor digestion limits nutrient use. Weight drops without effort. This weight loss signals ongoing damage from bile reflux .
Difficulty Sleeping Due to Symptoms
Symptoms worsen at night. Lying flat helps bile travel upward. Take sleep breaks often. Poor sleep worsens healing. Night symptoms are common with bile reflux .
Diagnosis of Bile Reflux
Diagnosing bile reflux requires tests that detect non-acid reflux. Standard acid tests may appear normal. Doctors rely on visual findings, bile movement tracking, and tissue changes to confirm bile-related injury.
Medical History and Symptom Review
Doctors ask about surgery history. They ask about vomiting color and pain timing. Bitter taste matters. Night symptoms matter. These clues help separate bile reflux from acid problems.
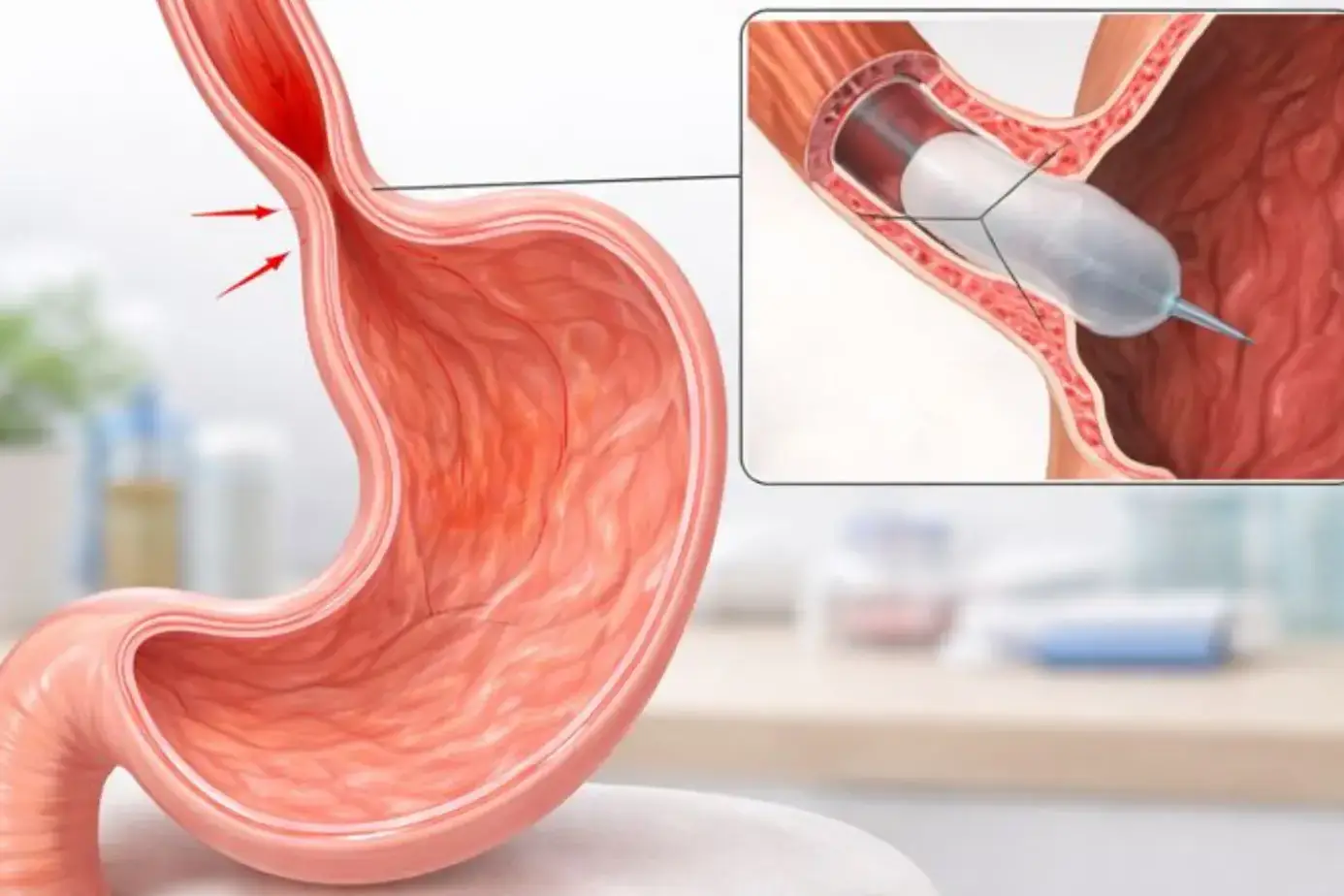
Upper Endoscopy
An endoscopy uses a thin camera tube. It enters through the mouth. Doctors look for bile pooling. They also check tissue redness and swelling. Visible bile strongly supports bile reflux .
Esophageal Impedance Monitoring
This test tracks liquid movement in the food pipe. It detects non-acid reflux. Acid tests alone can miss bile. This method helps confirm stubborn bile reflux cases.
HIDA Scan
A HIDA scan tracks bile movement from the liver. It shows abnormal flow patterns. Doctors use it when a surgical history exists. It helps confirm backward bile movement linked to bile reflux .
Gastric Biopsy Findings
Doctors may take tissue samples. Bile damage shows specific cell changes. These changes differ from acid injury. Biopsy results help confirm long-term bile reflux exposure.
Bile Reflux Treatments
Treatment plans often combine medication, diet control, and monitoring. Severe or resistant cases may need surgical correction.
Medications to Reduce Bile Irritation
Doctors often prescribe bile-binding medicines. These drugs bind to bile inside the stomach and intestine. Bound bile causes less irritation. This approach does not stop bile flow, but it lowers tissue damage. Doctors usually adjust the dose based on response and side effects.
Medications That Improve Gastric Emptying
Some medicines help the stomach empty faster. Faster emptying reduces pressure buildup. Less pressure means less backward bile flow. These drugs help most when nerve-related motility issues exist. Response varies by age and overall health.
Acid-Suppressing Therapy
Acid blockers alone do not treat bile reflux , but they help when acid reflux also exists. Acid makes bile damage worse. Lowering acid reduces combined injury. Doctors often use these drugs as supportive treatment, not as the main solution.
Surgical Treatment Options
Surgery becomes an option when medicine fails. The most common method reroutes bile away from the stomach. This surgery reduces bile exposure long-term. Doctors reserve surgery for severe cases due to risks and recovery time.
Managing Underlying Conditions
Treating ulcers, gastritis, and nerve disorders reduces symptoms. Blood sugar control helps nerve-related motility problems. Addressing root issues improves long-term outcomes and lowers flare-ups.
Foods to Avoid With Bile Reflux
Food choices directly affect bile release and stomach pressure. Knowing foods to avoid with bile reflux helps reduce daily symptoms. Avoiding triggers often lowers medication needs and improves comfort.
High-Fat and Fried Foods
Fat increases bile release. Fried foods slow digestion. Both raise backflow risk. Even healthy fats can trigger symptoms when eaten in large amounts.
Spicy Foods
Spices irritate the stomach lining. A damaged lining reacts faster to bile. This irritation worsens the burning and pain. Mild seasoning works better.
Chocolate and Caffeinated Drinks
Chocolate relaxes stomach valves. Caffeine increases stomach pressure. Both make reflux easier. These items often trigger night symptoms.
Alcohol
Alcohol damages the stomach’s protective layer. It also increases bile flow. Even small amounts can worsen bile reflux symptoms.
Citrus and Acidic Foods
Acidic foods irritate already-inflamed tissue. Citrus fruits and tomato-based foods often cause pain. Limiting intake reduces flare-ups.
Carbonated Beverages
Gas increases stomach pressure. Pressure pushes bile upward. Carbonated drinks often worsen bloating and reflux.
Lifestyle Changes for Bile Reflux
Simple changes like meal timing, posture, and sleep position reduce symptom frequency. Consistent habits support healing and improve long-term control.
Eating Smaller, Frequent Meals
Large meals stretch the stomach. Stretching raises pressure. Smaller meals reduce bile backflow risk. Eating every three hours helps digestion.
Avoiding Lying Down After Meals
Gravity helps digestion move forward. Lying flat allows bile to travel upward. Staying upright for at least three hours helps prevent reflux.
Weight Management
Extra weight increases abdominal pressure. This pressure pushes bile upward. Even modest weight loss can reduce symptom frequency.
Elevating the Head During Sleep
Raising the head of the bed limits nighttime reflux. Pillows alone often fail. Bed elevation uses gravity to protect the throat.
Smoking Cessation
Smoking weakens stomach defenses. It also slows healing. Quitting improves response to treatment and reduces irritation.
Bile Reflux Complications
The complications of bile reflux develop gradually with ongoing exposure. Damage may affect the stomach, food pipe, and nutrient absorption. Early treatment lowers the risk of permanent tissue changes.
Chronic Gastritis
Bile causes ongoing stomach lining. The lining thickens and scars over time. Pain becomes constant and harder to treat.
Esophagitis
Bile burns the food pipe lining. Swelling and sores form. Swallowing may hurt. Untreated damage can spread.
Barrett’s Esophagus
Repeated injury changes cell structure. These changes increase cancer risk. Doctors monitor this condition closely with regular exams.
Increased Risk of Esophageal Cancer
Long-term bile exposure damages DNA. Cancer risk rises with duration and severity. Early treatment lowers this risk.
Nutritional Deficiencies
Poor digestion limits nutrient absorption. Fat-soluble vitamins drop first. Weakness, bone issues, and fatigue may follow.
Prevention of Bile Reflux
Diet awareness, weight control, and follow-up care reduce long-term damage. People with prior surgery benefit most from regular monitoring.
Managing Digestive Disorders Early
Treat ulcers and gastritis promptly. Early treatment protects stomach valves. Delayed care increases long-term damage.
Dietary Modifications
Balanced meals reduce bile stress. Lower fat intake helps control bile release. Fiber supports smoother digestion.
Avoiding Trigger Foods
Tracking food reactions helps identify triggers. Removing problem foods reduces flare-ups. Personal triggers vary widely.
Long-Term Medical Follow-Up
Regular checkups diagnose damage early. Doctors adjust treatment as needed. Monitoring prevents silent progression.
FAQs
Is bile reflux dangerous?
Bile reflux can cause serious damage if untreated. Long-term exposure injures the stomach and food pipe, increases cancer risk, and leads to nutritional problems that affect overall health.
Can bile reflux be cured permanently?
Some people achieve long-term relief with surgery or strict management. Others control symptoms with medication and lifestyle changes. Results depend on cause, severity, and early diagnosis.
How is bile reflux different from GERD?
GERD involves stomach acid. Bile reflux involves bile. Acid blockers often fail alone. Diagnosis and treatment differ because bile damages tissue in a different way.
Does bile reflux cause vomiting?
Yes, vomiting can occur. Vomit often looks yellow or green and tastes bitter. This sign helps doctors separate bile reflux from other digestive disorders.
What foods make bile reflux worse?
High-fat foods, fried items, alcohol, chocolate, caffeine, and spicy foods worsen symptoms. Avoiding these reduces bile release and stomach pressure.
Can bile reflux damage the esophagus?
Yes, bile can severely damage the esophagus. Ongoing exposure causes inflammation, scarring, and cell changes that raise long-term cancer risk.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin