Hemochromatosis is an iron overload disorder. It’s caused by a genetic mutation. This mutation affects how the body controls iron absorption. As a result, excess iron can build up in key organs such as the liver, heart, and pancreas. This excess iron can lead to serious health issues. The article will discuss the possible connection between hemochromatosis and high blood pressure. It’ll also cover the condition in detail, mentioning its effects, diagnosis, and how it is managed.
Table of Contents
ToggleUnderstanding Hemochromatosis
Hemochromatosis is a genetic disorder that makes the body absorb too much iron. It stores this extra iron in vital organs. If not treated, this can lead to serious health problems.
What is Hemochromatosis?
This condition makes it hard for the body to control iron absorption. It leads to too much iron in tissues and organs. This can harm the liver, heart, and pancreas, causing health issues.
Types of Hemochromatosis
The most common type is from mutations in the HFE gene. There are also juvenile, neonatal, and secondary types. They result from specific anemias or liver problems.
Genetic Causes and Risk Factors
Hemochromatosis genetics are key in causing the disorder. Having altered HFE genes from both parents is a top risk for hereditary hemochromatosis. Factors like sex and ethnicity affect how likely you are to get the disorder.
People of Northern European descent, especially those with Celtic roots, are at higher risk. Men often show symptoms earlier than women, who lose some iron through menstruation.
The Impact of Iron Overload
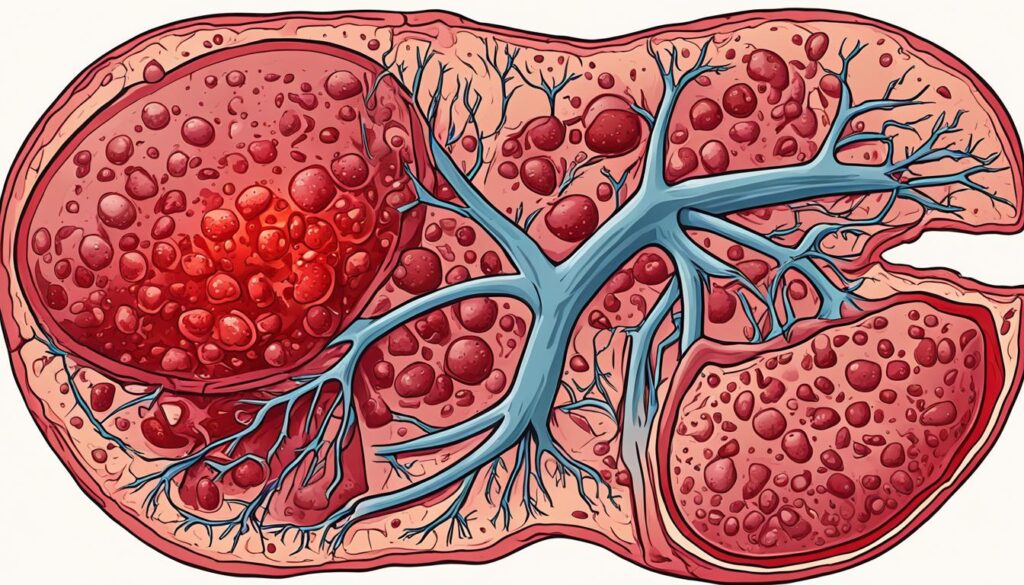
How Iron Overload Affects Organs
Having too much iron, a condition called hemochromatosis, stores in organs like the liver. This can harm them and even make them stop working. It might lead to diseases that last a long time, such as cirrhosis, diabetes, and heart failure.
These problems happen because the body’s usual iron-handling system, managed by the liver hormone hepcidin, doesn’t work right. In hemochromatosis, hepcidin can’t do its job. This lets the body soak up and store more iron than it should.
Liver Damage and Cirrhosis
Hemochromatosis hits the liver hard. Too much iron there can start liver fibrosis, which is scarring. Over time, this can turn into cirrhosis. Cirrhosis means the liver is badly scarred and can’t work well.
Cirrhosis raises the chance of getting liver cancer. It’s important for those with hemochromatosis to regularly check their liver health. They should also manage their iron levels. Doing so can help avoid serious liver problems.
Hemochromatosis and Cardiovascular Health
Hemochromatosis is a common iron overload disorder. It impacts the heart’s ability to pump blood right. This can lead to congestive heart failure. In this condition, the heart can’t pump blood well, causing fluid in the lungs and organs.
Iron Overload and Heart Failure
People with hemochromatosis face a higher risk of heart failure. This happens because too much iron harms the heart muscles. The heart can’t pump properly, causing problems like arrhythmias.
Arrhythmias and Conduction Abnormalities
Hemochromatosis may also cause arrhythmias. These are irregular heartbeats. They range from atrial fibrillation to ventricular tachycardia. Such heart issues can lead to stroke and sudden cardiac death.
Research aims to understand hereditary hemochromatosis better. It uses tools like echocardiography and magnetic resonance imaging. The goal is to detect and treat the disease early.
Can Hemochromatosis Cause High Blood Pressure?
The Link Between Iron Overload and Hypertension
New research has shown a possible link between hemochromatosis and high blood pressure. Hemochromatosis is when your body has too much iron. Studies prove that high iron levels and high blood pressure may be connected. This means having too much iron could lead to high blood pressure.
Potential Mechanisms Involved
Oxidative stress is a key player in this link. Iron causes our bodies to produce harmful molecules. These can damage our blood vessels, making them work less well. This, in turn, can lead to high blood pressure. Inflammation could also be making things worse. When our bodies react to too much iron, it might raise our blood pressure too. And if the iron collects in our blood vessels, they may not work as they should, adding to the problem.
Even though we’re still figuring out how hemochromatosis is related to high blood pressure, we know enough to take action. If you have hemochromatosis, managing your iron levels could help keep your heart and blood pressure healthy.
Diagnosis and Screening
Diagnosing hemochromatosis correctly is key to managing it well and preventing issues. Luckily, there are many good ways to find out if someone has this gene disorder. These tests include genetic tests and thorough blood tests.
Genetic Testing for Hemochromatosis
Genetic testing is the best way to diagnose hereditary hemochromatosis. It looks at the HFE gene to see if there are any mutations, like C282Y and H63D, linked to the disease. This test tells if someone has inherited hemochromatosis, the most usual type. Knowing this helps pick the right treatment and tracks how the disease is doing.
Blood Tests and Imaging
Besides genetic tests, doctors can also do blood tests to see if iron levels are too high, showing signs of hemochromatosis. High serum ferritin levels, usually over 200 ng/mL for women and 300 ng/mL for men, point to hemochromatosis with good odds. If blood shows high serum ferritin along with increased transferrin saturation, the diagnosis accuracy rises to 93%.
Doctors may use imaging tests like MRIs or CT scans to check iron levels in the body, especially the liver. These scans are safe and give important clues for diagnosis and tracking the disease over time.
Treatment Options
If you have hemochromatosis, your doctor will likely suggest two main treatments. These are therapeutic phlebotomy and iron chelation therapy. The goal is to lower your high iron levels. This will help prevent serious health issues that come with how to treat hemochromatosis.
Therapeutic Phlebotomy
The most usual treatment is therapeutic phlebotomy. It means regularly taking blood out to reduce iron levels. It’s like donating blood. Doctors do this often, maybe every week or month, depending on your blood tests and how severe your condition is.
Iron Chelation Therapy
Sometimes, iron chelation therapy is used. This might be when the other method isn’t an option. It uses special drugs to help the body get rid of extra iron. This helps protect your organs and tissues from the harm of too much iron.
Preventing Complications
It’s crucial to find hemochromatosis early. This helps avoid big health problems like liver disease and heart issues. With fast treatment, the chances of these dangers go way down.
Early Detection and Treatment
Getting checked for hemochromatosis is key. Tests for iron levels and genes can catch it early. After a diagnosis, doctors help set up a plan, often involving therapies to lower iron in the body.
Lifestyle Modifications
Changing how you live can also make a big difference. This means less iron in your food, not taking iron pills, and staying at a good weight. These steps help manage the disease and keep you healthy.
Ongoing Research
Scientists are always looking into new ways to treat hemochromatosis. They are checking out if hepcidin-based medicines can help. These new treatments are working to fix why too much iron builds up in the body. This is a big problem in hemochromatosis.
Exploring New Treatment Approaches
One key area of study is using hepcidin. This is a liver hormone that’s very important for iron balance. Experts are looking into making medicines based on hepcidin. These might help the body control iron better. This could lessen the bad effects of too much iron in hemochromatosis.
Understanding the Mechanisms
Researchers are also trying to understand why too much iron causes health problems in hemochromatosis. They are specifically looking at how it affects the heart and blood pressure. By studying these effects, experts want to find new ways to treat the disorder. Their goal is to make managing hemochromatosis easier.
Living with Hemochromatosis
People with hemochromatosis may find it hard to deal with its effects. This includes how it impacts the body, emotions, and social life. Yet, having the right ways to cope and support makes a big difference. You can learn to live well despite this genetic disorder.
Coping Strategies and Support
It helps to talk to doctors and be part of support groups. Participating in activities that lower stress is also good. Support from friends and family, as well as counseling, is key in handling how you feel about the condition.
Building a strong support system is critical. This network should include loved ones and health professionals. They can provide helpful advice and understanding as you manage your condition every day.
Monitoring and Managing Symptoms
Keeping an eye on your iron levels is crucial. This means following the treatment you are given. Lifestyle changes are also important. They help you deal with hemochromatosis symptoms better and lower the risk of other health issues.
Eating less food high in iron can support your treatment. It’s important to keep a healthy weight and stay active. Not drinking alcohol and staying away from smoking also help. These steps lead to a better life with hemochromatosis.
Conclusion
Hemochromatosis is a genetic disorder that makes your body keep too much iron. This can lead to serious health issues, like causing high blood pressure. Science is still learning about how too much iron might make blood pressure go up. But, it seems to link with ways your body handles stress, fights off infections, and keeps your blood vessels healthy.
If you have hemochromatosis, working with your doctor is key to keeping you safe. They will help find it early and start treatment fast. They’ll also guide you on how to lower the risk of problems, such as high blood pressure. By doing what your doctor says and changing how you live where needed, you can do a lot to protect your heart and stay healthy. It’s all about being well-informed and actively taking care of yourself.
Dealing with hemochromatosis might be tough sometimes. But, you’re not alone. With good support and being ready to act, this health issue won’t stop you from enjoying life. Each person’s experience with hemochromatosis is different. By being watchful and working hand in hand with your healthcare team, you can keep moving forward confidently.
FAQ
What is hemochromatosis?
What are the types of hemochromatosis?
What are the risk factors for developing hemochromatosis?
How does iron overload affect the body?
How does hemochromatosis affect the heart?
Can hemochromatosis cause high blood pressure?
How is hemochromatosis diagnosed?
How is hemochromatosis treated?
How can complications from hemochromatosis be prevented?
What are some of the ongoing research areas for hemochromatosis?
Source Links
- https://www.mayoclinic.org/diseases-conditions/hemochromatosis/symptoms-causes/syc-20351443
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8716004/
- https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/haemochromatosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5996563/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10368456/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10499463/
- https://www.medicalnewstoday.com/articles/166455
- https://academic.oup.com/ajh/article/25/4/492/2743111


