Vanishing bile duct syndrome (VBDS) is a rare but serious outcome and complication of drug-induced liver injury. It is characterized by the progressive destruction and disappearance of the bile ducts in the liver, leading to cholestasis, which is the slowed or stopped flow of bile. VBDS typically occurs after a bout of severe cholestatic hepatitis and is marked by chronic cholestasis and histological loss of intrahepatic bile ducts.
Table of Contents
ToggleThe onset of VBDS usually happens 1 to 6 months after the initial liver injury. Common symptoms of VBDS include persistent pruritus, fatigue, jaundice, and dyslipidemia. Elevations in alkaline phosphatase, bilirubin, cholesterol, and bile acid levels are often seen in patients with VBDS.
Various drugs have been linked to VBDS, including amoxicillin/clavulanate, penicillins, fluoroquinolones, sulfonamides, antifungal agents, NSAIDs, and anticonvulsants. Other conditions that can mimic or cause VBDS include graft-vs-host disease, Hodgkin’s disease, sclerosing cholangitis, and primary biliary cholangitis.
Diagnosis of VBDS requires a liver biopsy to confirm the paucity of intrahepatic bile ducts. Management of VBDS focuses on alleviating symptoms, preventing further liver injury, and monitoring for disease progression. Treatment options include antihistamines for pruritus, bile acid resins to trap pruritogenics, corticosteroids (although their efficacy in VBDS is uncertain), ursodiol to ameliorate liver injury, and vitamin and mineral replacement. In severe cases, liver transplantation may be necessary.
What is Vanishing Bile Duct Syndrome?
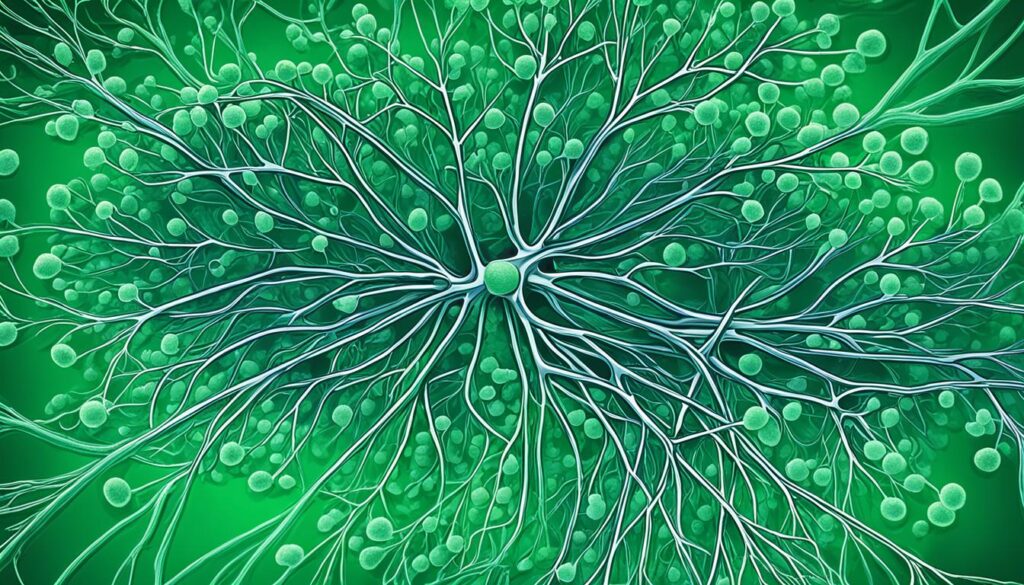
Vanishing bile duct syndrome (VBDS) is a condition characterized by the progressive destruction and disappearance of the bile ducts in the liver. The bile ducts play a crucial role in transporting bile from the liver and gallbladder to the small intestine to aid in the digestion of fats.
In VBDS, the bile ducts become injured and eventually die off, leading to cholestasis, which is the decreased or blocked flow of bile. This impaired bile flow can result in various complications and liver damage.
The exact mechanism behind VBDS is not fully understood, but it can be attributed to immune-mediated disorders, infections, cancers, and certain medications. It is important to note that VBDS is often associated with drug-induced liver injury, with antibiotics being the most commonly linked class of medications.
Common symptoms of VBDS may include itching, jaundice (yellowing of the skin and eyes), fatigue, stomach pain, loss of appetite, and weight loss. If left untreated, VBDS can lead to permanent liver damage and serious complications.
Diagnosing VBDS typically involves a liver biopsy to confirm ductopenia, which is characterized by a decrease in the number of bile ducts. This condition can significantly impact liver function and necessitates appropriate medical management.
In the next section, we will explore the causes and risk factors associated with Vanishing Bile Duct Syndrome.
Causes and Risk Factors of Vanishing Bile Duct Syndrome
Vanishing bile duct syndrome (VBDS) can occur as a result of various conditions that lead to liver injury. These include viral and non-viral hepatitis, infections, cirrhosis, tumors, ischemic conditions affecting the biliary tree, and autoimmune conditions.
Additionally, certain medications and toxins can damage the liver and contribute to the development of VBDS. Antibiotics such as penicillins, fluoroquinolones, and sulfonamides, as well as antifungal agents, NSAIDs, anticonvulsants, phenothiazines, tricyclic antidepressants, and certain seizure medications, have been associated with VBDS.
Furthermore, long-term heavy alcohol use is a significant risk factor for VBDS, as alcohol can cause liver injury. It’s important to avoid excessive alcohol consumption to reduce the risk of developing VBDS.
Exposure to viruses that cause hepatitis, such as hepatitis A and B, also increases the likelihood of developing VBDS. Proper vaccination against hepatitis A and B is recommended to help prevent viral hepatitis and its associated complications.
People who have undergone organ transplants are at risk of graft-vs-host disease, which can lead to the development of VBDS. It’s crucial to carefully manage the post-transplant condition and seek regular medical follow-up to monitor for any potential complications.
In order to minimize the risk of developing VBDS, it is advisable to avoid alcohol, toxic chemicals, and practice good hygiene. These preventive measures can promote liver health and reduce the likelihood of developing VBDS.
Symptoms and Diagnosis of Vanishing Bile Duct Syndrome
Symptoms of vanishing bile duct syndrome (VBDS) can vary depending on the underlying condition. Common symptoms include persistent itching, jaundice (yellowing of the skin), fatigue, stomach pain, loss of appetite, and weight loss. Some patients may be asymptomatic, and VBDS is initially identified based on laboratory abnormalities. Patients with chronic cholestasis may also experience skin xanthomas (fatty skin lesions), dyslipidemia (abnormal fat levels in the blood), and deficiencies in fat-soluble vitamins (A, D, E, and K).
Laboratory tests to diagnose VBDS include liver function tests, which typically show elevated levels of alkaline phosphatase, total bilirubin, and gamma-glutamyl transpeptidase. Imaging tests, such as MRIs, CT scans, or ultrasounds, may be done to evaluate the abdomen. However, the definitive diagnosis of VBDS requires a liver biopsy, which can confirm the paucity of intrahepatic bile ducts. A hepatologist will perform a physical exam, review medical history, and order these tests to diagnose VBDS.
| Common Symptoms of VBDS | Laboratory Abnormalities |
|---|---|
| Persistent itching | Elevated alkaline phosphatase levels |
| Jaundice (yellowing of the skin) | Elevated total bilirubin levels |
| Fatigue | Elevated gamma-glutamyl transpeptidase levels |
| Stomach pain | |
| Loss of appetite | |
| Weight loss |

Medications Associated with Vanishing Bile Duct Syndrome
Vanishing bile duct syndrome (VBDS) has been linked to various medications, particularly antibiotics. These medications have been reported to cause VBDS in some individuals. The exact mechanism by which these medications cause VBDS is not fully understood but is believed to involve immune-mediated processes and liver injury.
Some of the antibiotics frequently associated with VBDS include:
- Penicillins, such as amoxicillin and amoxicillin/clavulanate
- Fluoroquinolones, like ciprofloxacin and moxifloxacin
- Sulfonamide antibiotics, such as trimethoprim/sulfamethoxazole
In addition to antibiotics, other drug classes that have been implicated in causing VBDS include antifungal agents, NSAIDs, anticonvulsants (e.g., carbamazepine, lamotrigine), and certain antivirals (e.g., nevirapine).
It’s important to note that any severe acute cholestatic or mixed hepatitis may lead to VBDS, regardless of the specific medications involved.
Medications Associated with Vanishing Bile Duct Syndrome
| Medication Class | Examples |
|---|---|
| Antibiotics | Penicillins (amoxicillin, amoxicillin/clavulanate) Fluoroquinolones (ciprofloxacin, moxifloxacin) Sulfonamides (trimethoprim/sulfamethoxazole) |
| Antifungal Agents | Not applicable |
| NSAIDs | Not applicable |
| Anticonvulsants | Carbamazepine, lamotrigine |
| Antivirals | Nevirapine |
This table provides an overview of various medication classes associated with VBDS. It is important to consult with a healthcare professional for personalized information regarding the medications you are currently taking or considering.

Complications of Vanishing Bile Duct Syndrome
Vanishing bile duct syndrome (VBDS) can lead to serious complications that significantly impact your health and quality of life. Two main complications associated with VBDS are ductopenia and cholestasis.
Ductopenia
Ductopenia refers to the decrease in the number of bile ducts in your liver. As the bile ducts progressively disappear in VBDS, it can lead to a significant reduction in their number. This can impair the normal flow of bile, leading to further liver damage and complications.
Cholestasis
Cholestasis occurs when there is a decreased or blocked flow of bile. In VBDS, the destruction and loss of bile ducts can result in cholestasis. This can lead to a buildup of bile in the liver, causing liver injury and impairing its normal function.
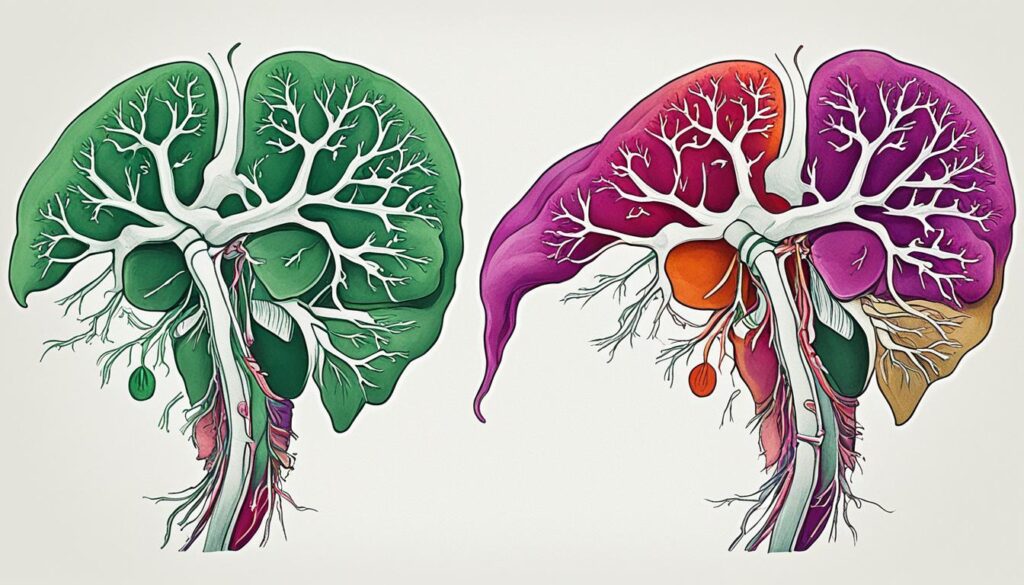
Both ductopenia and cholestasis associated with VBDS can have severe consequences for your liver. In some cases, the liver damage may progress to liver failure, a life-threatening condition where the liver is unable to perform its essential functions.
When VBDS reaches a critical stage, a liver transplantation may be necessary to save your life. Liver transplantation involves surgically replacing the damaged liver with a healthy liver from a donor. It is a complex procedure that requires careful evaluation and planning to ensure the best possible outcome.
It is crucial to diagnose and manage VBDS promptly and effectively to minimize the risk of these complications. Regular monitoring, proper symptom management, and adherence to treatment plans are essential in preserving liver function and improving your overall well-being.
Treatment and Management of Vanishing Bile Duct Syndrome
The treatment and management of vanishing bile duct syndrome (VBDS) depend on several factors, including the underlying condition causing the bile duct injury and the severity of the symptoms. The primary goal of treatment is to prevent further liver injury, alleviate symptoms, and improve overall quality of life.
In many cases, addressing and treating the underlying condition causing VBDS can lead to symptom resolution. For example, if VBDS is caused by a medication, discontinuing that medication may lead to improvement. However, this is not always possible or may not be enough to reverse VBDS completely.
Symptom management for VBDS includes the following strategies:
- Antihistamines for pruritus (itching): These medications can help relieve itching, a common symptom of VBDS. They work by blocking the histamine receptors in the body, reducing the sensation of itchiness.
- Bile acid resins to trap pruritogenics: These medications bind to bile acids in the intestines, preventing their reabsorption and reducing itchiness. They can help manage pruritus in people with VBDS.
- Ursodiol: This medication is commonly used in the treatment of VBDS to ameliorate liver injury. Ursodiol helps to improve the flow of bile and can have a protective effect on the liver.
- Corticosteroids: In severe cases of cholestasis and VBDS, corticosteroids may be used. However, it is important to note that their efficacy in VBDS is uncertain, and the decision to use corticosteroids is made on an individual basis.
In some cases, liver transplantation may be necessary to save the patient’s life. Liver transplantation can replace the damaged liver with a healthy one from a donor. It is considered in severe cases where VBDS has led to liver failure or other life-threatening complications.
Proper nutrition and vitamin and mineral replacement are also essential in managing VBDS. A balanced diet and appropriate supplementation can help support liver health and overall well-being.
Overall, the treatment and management of VBDS require a personalized approach based on the individual’s specific condition. Working closely with healthcare professionals, including hepatologists, can help ensure a comprehensive and effective treatment plan for VBDS.
Prognosis and Outlook for Vanishing Bile Duct Syndrome
The prognosis and outlook for vanishing bile duct syndrome (VBDS) can vary depending on the underlying cause, the severity of bile duct damage, and the effectiveness of treatment. For individuals with mild forms of VBDS, there is a possibility of gradual recovery over a few months to possibly years.
However, severe cases of VBDS can have long-lasting effects on a person’s health. Despite appropriate treatment, some individuals may eventually require a liver transplantation to survive. In such cases, a liver transplant can significantly improve the prognosis and quality of life.
It’s important to note that VBDS can cause lingering liver damage even after treatment. Therefore, long-term medical management is often necessary to maintain liver health and prevent complications.
To ensure the best possible prognosis for patients with VBDS, it is crucial to undergo close monitoring, properly manage symptoms, and strictly adhere to treatment plans. Regular follow-ups with healthcare providers and consistent self-care practices play a vital role in effectively managing VBDS and promoting recovery.
Remember that early detection, timely treatment, and proper management are key factors in achieving the best outcomes for individuals with vanishing bile duct syndrome.
Prevention of Vanishing Bile Duct Syndrome
To reduce your risk of developing vanishing bile duct syndrome (VBDS), there are several preventive measures you can take. By adopting these practices, you can promote liver health and decrease the likelihood of developing VBDS.
Vaccination
One of the key preventive measures against VBDS is vaccination. Make sure to receive the hepatitis A and hepatitis B vaccines, as these can help protect against viral hepatitis, which is a potential cause of VBDS. While vaccines for other forms of viral hepatitis are not currently available, getting vaccinated against hepatitis A and B can significantly reduce your risk of developing VBDS.
Alcohol Avoidance
Limiting or avoiding alcohol consumption is another important step in reducing the risk of liver damage and subsequently VBDS. Excessive alcohol consumption can lead to liver injury and cholestasis, increasing the chances of developing VBDS. By practicing moderation or abstaining from alcohol consumption altogether, you can protect your liver and minimize the risk of VBDS.
Toxin Avoidance
Avoiding exposure to toxic chemicals is crucial in preventing VBDS. Certain chemicals and toxins can damage the liver and contribute to the development of bile duct injury. Take precautions to limit your exposure to harmful substances in your environment, such as industrial chemicals, cleaning agents, and pesticides. Additionally, practicing good hygiene, including handwashing and maintaining a clean living environment, can further decrease the risk of developing VBDS.
| Preventive Measures | Description |
|---|---|
| Vaccination | Receive hepatitis A and B vaccines to protect against viral hepatitis and reduce the risk of developing VBDS. |
| Alcohol Avoidance | Limit or avoid alcohol consumption to prevent liver damage and decrease the chances of developing VBDS. |
| Toxin Avoidance | Avoid exposure to toxic chemicals and practice good hygiene to minimize the risk of developing VBDS. |
Living with Vanishing Bile Duct Syndrome
Living with vanishing bile duct syndrome (VBDS) can vary depending on the severity of the condition. For individuals with mild forms of VBDS, the prognosis may be more favorable, with gradual recovery over time. These individuals may experience fewer limitations and may not require invasive treatments such as a liver transplant.
However, individuals with severe VBDS may face ongoing challenges and the need for more intensive medical management. Ongoing monitoring, adherence to treatment plans, and regular follow-up with healthcare providers are vital for maintaining liver health and managing symptoms.
In some cases, a liver transplant may be necessary to improve the quality of life and prolong survival.
With proper care and support, individuals with VBDS can lead fulfilling lives and effectively manage their condition.
Daily Tips for Living with VBDS:
- Follow a healthy diet tailored to your liver condition, including a balance of nutrients and avoiding substances that may worsen symptoms or strain the liver.
- Take medications as prescribed and attend regular check-ups with your healthcare team to monitor your liver function and adjust treatment plans if needed.
- Engage in gentle exercise and physical activity that is suitable for your condition, aiming to maintain overall health and well-being.
- Manage stress levels through relaxation techniques, such as deep breathing exercises or mindfulness practices.
- Seek support from support groups or organizations that specialize in liver diseases to connect with others facing similar challenges and gain valuable insights.
By adopting these strategies and working closely with your healthcare team, you can navigate the challenges of VBDS and lead a fulfilling life.
Testimonials from Individuals Living with VBDS:
| Name | Location | Experience |
|---|---|---|
| Maria | New Delhi, India | While initially overwhelmed by my diagnosis of severe VBDS, I have learned to adapt and prioritize my health. With the guidance of my healthcare team, I have managed my symptoms through medication and regular monitoring. It has been challenging, but I am grateful for the support network I have found and the improvements I have seen in my quality of life. |
| Rajesh | Mumbai, India | Living with mild VBDS has allowed me to focus on self-care and make the necessary lifestyle adjustments. By maintaining a nutritious diet, taking prescribed medications, and staying physically active, I have experienced steady progress in managing my condition. Regular check-ups with my hepatologist and connecting with others in similar situations have been instrumental in my journey. |
| Priya | Bangalore, India | Severe VBDS presented significant challenges, requiring a liver transplant to regain my health. The surgery was life-changing, and with ongoing medical management, I have been able to enjoy an active life post-transplant. It is essential to stay disciplined with medications, attend follow-up appointments, and prioritize self-care to ensure the success and longevity of the transplant. |
Research and Innovation in Vanishing Bile Duct Syndrome
Research and innovation in the field of vanishing bile duct syndrome (VBDS) are focused on finding more effective treatments and potential breakthroughs. Scientists and medical professionals are exploring experimental approaches to treating VBDS, including the use of immunosuppression with calcineurin inhibitors or monoclonal antibodies.
Calcineurin inhibitors are medications that work by suppressing the immune system, reducing inflammation, and preventing further damage to the bile ducts. Monoclonal antibodies, on the other hand, are laboratory-made molecules that target specific immune cells or proteins involved in the development of VBDS.
These experimental approaches are currently being investigated in clinical trials to evaluate their safety and efficacy in managing VBDS. By modulating immune responses and reducing inflammation, these innovative therapies aim to alleviate symptoms, prevent disease progression, and improve outcomes for individuals with this rare and challenging condition.
Advancements in VBDS Research
The ongoing research efforts in the field of VBDS are focused on improving our understanding of the underlying mechanisms of the disease. Scientists are studying the immune responses involved in the destruction of bile ducts and identifying potential targets for intervention.
Advancements in technology and genetic research have also opened up new avenues for studying VBDS. Researchers are using sophisticated techniques to analyze the genetic factors that contribute to the development of the syndrome, with the aim of identifying potential biomarkers and personalized treatment approaches.
Clinical Trials
Clinical trials play a crucial role in VBDS research, as they help evaluate the safety and effectiveness of new treatments. These trials involve carefully designed studies that include patients with VBDS who are willing to participate in testing the experimental approaches.
During clinical trials, researchers closely monitor participants and collect data to assess the effects of the experimental treatments. The insights gained from these trials help guide the development of new therapies and improve the overall management of VBDS.
The Promise of Research and Innovation
The advancements in research and innovation bring hope to individuals living with VBDS. The identification of new treatment targets, along with the development of more effective therapies, holds the potential to significantly improve the quality of life for patients.
By continuing to invest in research and clinical trials, scientists and medical professionals aim to develop targeted treatments that can halt the progression of VBDS, restore normal bile duct function, and prevent complications associated with the condition.
As research progresses and new discoveries are made, individuals with VBDS can look forward to a future with improved treatment options and a better outlook for their liver health.
Ongoing Research in Vanishing Bile Duct Syndrome
| Research Area | Description |
|---|---|
| Immunosuppression with calcineurin inhibitors | Investigating the use of medications to suppress the immune system and reduce inflammation in VBDS |
| Monoclonal antibodies | Studying the effectiveness of laboratory-made molecules that target immune cells and proteins involved in VBDS |
| Genetic research | Exploring the genetic factors that contribute to the development of VBDS, with the aim of identifying potential biomarkers |
| Personalized treatment approaches | Investigating the potential for tailoring treatment plans based on individual genetic profiles and disease characteristics |
| Improved diagnostic techniques | Developing advanced imaging and laboratory tests to aid in early detection and accurate diagnosis of VBDS |
Conclusion
Vanishing bile duct syndrome (VBDS) is a rare but serious condition that can have significant implications for liver health. The progressive destruction and disappearance of the bile ducts in the liver can lead to cholestasis, liver damage, and potentially life-threatening complications. It can be caused by various factors, including medication use, liver injury, infections, and autoimmune conditions.
Diagnosis of VBDS requires a liver biopsy to confirm the paucity of intrahepatic bile ducts. Once diagnosed, treatment options focus on addressing the underlying cause, managing symptoms, preventing further liver injury, and monitoring for disease progression. While mild cases of VBDS may respond to conservative management approaches, such as discontinuing medications or treating underlying infections, severe cases may require more intensive interventions, including liver transplantation.
With proper management and ongoing medical care, individuals with VBDS can achieve improved liver health and maintain a good quality of life. Symptom management, such as using antihistamines for pruritus and bile acid resins to trap pruritogenics, can help alleviate discomfort. Additionally, medications like corticosteroids and ursodiol may be used to ameliorate liver injury. Ongoing research in the field aims to find more effective treatments and better understand the underlying mechanisms of VBDS, ultimately improving outcomes for patients.
By prioritizing liver health, seeking timely medical attention, and adhering to treatment plans, individuals with VBDS can optimize their overall well-being and lead fulfilling lives.
FAQ
What is vanishing bile duct syndrome (VBDS)?
VBDS is a rare condition characterized by the progressive destruction and disappearance of the bile ducts in the liver, leading to cholestasis, which is the slowed or stopped flow of bile.
What causes vanishing bile duct syndrome?
VBDS can be caused by various factors, including infections, autoimmune conditions, liver injury, and certain medications.
What are the symptoms of vanishing bile duct syndrome?
Common symptoms of VBDS include persistent itching, jaundice, fatigue, stomach pain, loss of appetite, and weight loss.
How is vanishing bile duct syndrome diagnosed?
Diagnosis of VBDS requires a liver biopsy to confirm the paucity of intrahepatic bile ducts.
Which medications are associated with vanishing bile duct syndrome?
Antibiotics, such as penicillins, fluoroquinolones, and sulfonamides, as well as antifungal agents, NSAIDs, and anticonvulsants, have been linked to VBDS.
What are the complications of vanishing bile duct syndrome?
Complications of VBDS include ductopenia, cholestasis, liver damage, and, in severe cases, liver failure and the need for a liver transplant.
How is vanishing bile duct syndrome treated and managed?
The treatment of VBDS focuses on addressing the underlying condition, managing symptoms, and preventing further liver injury. Antihistamines, bile acid resins, corticosteroids, ursodiol, and liver transplantation may be used as treatment options.
What is the prognosis for vanishing bile duct syndrome?
The prognosis for VBDS depends on various factors, but with proper management, individuals can achieve improved liver health and maintain a good quality of life.
Can vanishing bile duct syndrome be prevented?
While not all cases can be prevented, certain measures such as vaccination against hepatitis A and B, limiting alcohol consumption, and avoiding exposure to toxins can help reduce the risk of developing VBDS.
How does vanishing bile duct syndrome affect daily life?
Living with VBDS can vary depending on the severity of the condition. While mild forms may have fewer limitations, severe cases may require ongoing medical management and, in some instances, a liver transplant.
What research is being done on vanishing bile duct syndrome?
Ongoing research is focused on finding more effective treatments and understanding the underlying mechanisms of VBDS to improve outcomes for patients.
Source Links


