Barrett’s esophagus is a condition that occurs when the cells in the esophagus start to resemble those in the intestines due to prolonged exposure to stomach acid. Commonly seen in individuals with gastroesophageal reflux disease (GERD), Barrett’s esophagus can lead to a higher risk of developing esophageal cancer if left untreated. Early detection plays a crucial role in preventing the progression of the condition.
Table of Contents
ToggleIf you experience frequent heartburn, chest pain, difficulty swallowing, or notice the presence of blood in your vomit or in black or tarry stools, it is essential to recognize these symptoms as potential signs of Barrett’s esophagus.
Early detection allows for timely intervention, reducing the risk of complications and providing a better outcome. By being proactive in recognizing the symptoms associated with Barrett’s esophagus, you can take the necessary steps towards early detection and appropriate treatment.
What Causes Barrett’s Esophagus
In order to understand the causes of Barrett’s esophagus, it is important to first grasp the concept of gastroesophageal reflux disease (GERD). GERD occurs when the muscles at the bottom of the esophagus do not function properly, allowing food and stomach acid to flow back up into the esophagus.
Over time, this repeated exposure to stomach acid can lead to the development of Barrett’s esophagus. The cells in the esophagus undergo changes and become abnormal, resembling the cells found in the intestines. This transformation is believed to be a protective response to the acid.
While the exact cause of Barrett’s esophagus is still unknown, it is commonly associated with GERD. The chronic inflammation caused by GERD is thought to play a key role in the development of Barrett’s esophagus.
Aside from GERD, there are other risk factors that can increase the likelihood of developing Barrett’s esophagus. These include:
- Being male
- Being of Caucasian ethnicity
- Being over the age of 50
- H. pylori gastritis (infection of the stomach lining)
- Smoking
- Being overweight or obese
Understanding these risk factors can help individuals recognize their susceptibility to Barrett’s esophagus and take appropriate measures to manage their health.
Recognizing the Symptoms of Barrett’s Esophagus
Barrett’s esophagus itself does not have any symptoms. However, most people with this condition also have gastroesophageal reflux disease (GERD), which can cause frequent heartburn. It is important to recognize symptoms that may indicate a more serious condition.
If you experience any of the following symptoms, it is important to seek medical attention:
- Chest pain: This may manifest as a burning sensation or discomfort in your chest area. It can occur after eating or when lying down.
- Difficulty swallowing: If you find it challenging to pass food or liquid down your esophagus, it may be a sign of Barrett’s esophagus.
- Vomiting blood: The presence of blood in your vomit can be an alarming symptom and requires immediate medical evaluation.
Additionally, if you notice black or tarry stools, it could indicate bleeding in your digestive tract, which also necessitates prompt medical attention.
Remember, early detection is crucial for the proper management of Barrett’s esophagus and the prevention of potential complications. By being aware of these symptoms and seeking timely medical care, you can take control of your health and ensure appropriate treatment.

Example Table:
| Symptom | Description |
|---|---|
| Chest Pain | A burning sensation or discomfort in the chest area, often after eating or while lying down. |
| Difficulty Swallowing | Challenges in passing food or liquid down the esophagus. |
| Vomiting Blood | Persistent presence of blood in vomit, indicating potential bleeding in the digestive tract. |
| Black or Tarry Stools | Dark and sticky stool, suggestive of bleeding in the digestive system. |
Diagnosing and Classifying Barrett’s Esophagus
If your doctor suspects that you have Barrett’s esophagus, they may order an endoscopy. This procedure uses a small camera to examine the inside of your esophagus. During the endoscopy, your doctor may take a tissue sample to further evaluate the condition of your esophagus.
The tissue sample will be examined for dysplasia, which is the presence of abnormal cells. Dysplasia can be ranked as no dysplasia, low-grade dysplasia, or high-grade dysplasia, indicating the level of cell abnormalities and the potential for cancerous changes.

| Dysplasia Grade | Cell Abnormalities | Potential for Cancer |
|---|---|---|
| No Dysplasia | No abnormal cells | Low risk |
| Low-Grade Dysplasia | Mild cell abnormalities | Intermediate risk |
| High-Grade Dysplasia | Severe cell abnormalities | High risk |
Treatment Options for Barrett’s Esophagus
When it comes to treating Barrett’s esophagus, the approach will depend on the level of dysplasia present. Dysplasia refers to the abnormal changes in the cells of the esophagus lining. Let’s explore the treatment options available for different levels of dysplasia.
No or Low-Grade Dysplasia
If you have no or low-grade dysplasia, the focus of treatment is primarily on managing the symptoms of gastroesophageal reflux disease (GERD). GERD is a common condition that often goes hand in hand with Barrett’s esophagus. Your doctor may recommend the following treatment options:
- Medication: Prescription-strength proton pump inhibitors or H2-receptor antagonists can help reduce stomach acid production and alleviate GERD symptoms.
- Lifestyle modifications: Making changes to your diet, such as avoiding trigger foods, eating smaller meals, and maintaining a healthy weight, can help alleviate GERD symptoms.
- Anti-reflux surgery: In some cases, surgical procedures like Nissen fundoplication or LINX device insertion may be recommended to strengthen the lower esophageal sphincter and prevent acid reflux.
High-Grade Dysplasia
If you have been diagnosed with high-grade dysplasia, more aggressive treatment options are typically recommended. High-grade dysplasia indicates a higher risk of progression to esophageal cancer. The treatment options may include:
- Radiofrequency ablation (RFA): This technique uses heat energy to destroy the abnormal cells in the esophagus lining, helping to reduce the risk of cancer development.
- Cryotherapy: Cryotherapy involves freezing the abnormal cells, causing them to die and be replaced by healthy cells.
- Photodynamic therapy (PDT): PDT uses a light-sensitive drug to target and destroy the abnormal cells.
It’s important to note that the choice of treatment will depend on various factors, including your overall health and medical history. Consulting with your doctor is crucial in determining the most appropriate treatment plan for your specific condition.
Remember, the goal of treatment for Barrett’s esophagus is to alleviate symptoms, reduce the risk of esophageal cancer, and improve your overall quality of life. Regular monitoring and follow-up with your healthcare provider are essential to ensure the effectiveness of the chosen treatment and detect any changes in your condition.

Complications of Barrett’s Esophagus
While Barrett’s esophagus itself does not typically cause any symptoms, it can lead to several complications, the most significant of which is an increased risk of developing esophageal cancer. However, it is important to note that the probability of developing cancer is statistically low. Regular monitoring and follow-up with your doctor are crucial to detect any potentially cancerous changes in the early stages and ensure appropriate treatment.
Aside from the risk of esophageal cancer, Barrett’s esophagus can also cause other complications:
- Chest pain: Some individuals with Barrett’s esophagus may experience chest pain, which can be similar to the discomfort felt during a heart attack. If you experience persistent or severe chest pain, it is important to seek medical attention immediately to rule out any serious conditions.
- Narrowing of the esophagus: Over time, the cells in the esophagus can undergo changes that result in the narrowing of the esophageal passage. This can make swallowing difficult and may require additional medical interventions to alleviate the symptoms.
- Cuts or rupture of the esophagus: In rare cases, the lining of the esophagus in individuals with Barrett’s esophagus can become fragile and prone to tears or perforations. This can cause severe pain, difficulty swallowing, and may require immediate medical attention.
It is important to maintain open communication with your healthcare provider and adhere to regular check-ups to monitor the condition of your esophagus. This proactive approach will ensure any complications or changes are promptly identified and managed appropriately.
Outlook for Barrett’s Esophagus
Barrett’s esophagus is a condition that increases the risk of developing esophageal cancer. However, it’s important to note that many people with Barrett’s esophagus never develop cancer. With the right approach, you can effectively manage this condition and reduce the risk of complications.
To improve your outlook, it is crucial to work closely with your doctor to create a comprehensive treatment plan. This plan should focus on managing the symptoms of gastroesophageal reflux disease (GERD) through lifestyle changes and medication.
Lifestyle changes:
- Quit smoking: Smoking can aggravate GERD symptoms and hinder the healing of the esophageal lining. Quitting smoking may help reduce inflammation and improve overall esophageal health.
- Limit alcohol consumption: Alcohol can contribute to acid reflux and worsen GERD symptoms. Cutting back on alcohol or avoiding it altogether can be beneficial.
- Avoid trigger foods: Certain foods, such as spicy or acidic items, can trigger or worsen GERD symptoms. Identifying and avoiding these trigger foods can help alleviate discomfort.
Medication:
Your doctor may prescribe medications to manage GERD symptoms and reduce the production of stomach acid. Proton pump inhibitors (PPIs) and H2-receptor antagonists are commonly used to control acid reflux and promote healing of the esophagus.
Regular follow-up appointments are crucial in monitoring the condition of your esophageal lining. Your doctor may recommend periodic endoscopies to examine the esophagus and detect any cancerous changes in the early stages. By detecting and addressing potential issues early, you can take proactive steps to reduce the risk of complications and ensure proper management of Barrett’s esophagus.

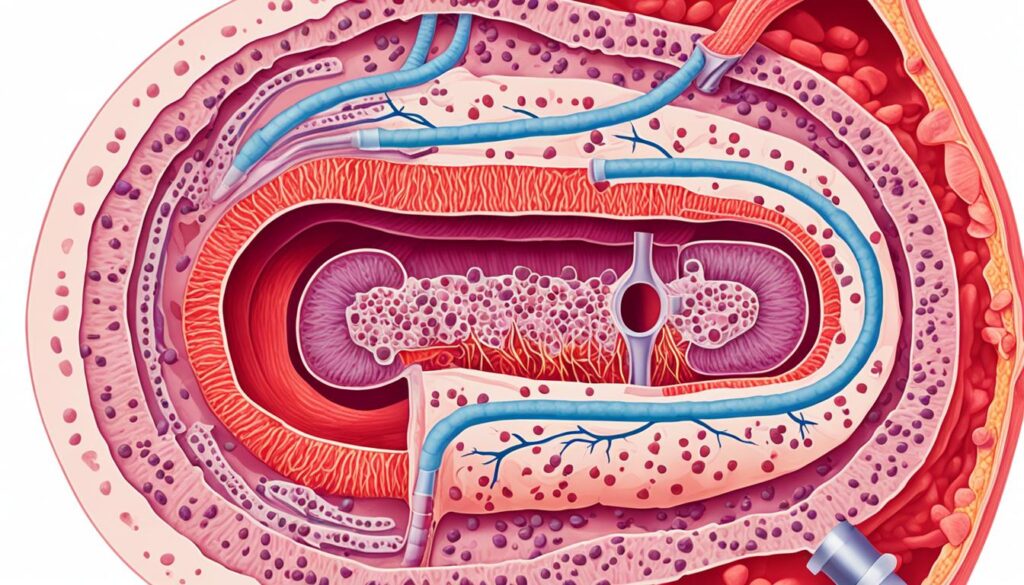
Definition and Pathology of Barrett’s Esophagus
Barrett’s esophagus is a condition where the normal lining of the esophagus is damaged by acid reflux and replaced by a type of cell similar to that found in the intestines. This change is known as metaplasia. The exact cellular origin of Barrett’s esophagus is still unknown. It is considered a pre-malignant condition, as it increases the risk of developing esophageal cancer.
Risk Factors and Prevention of Barrett’s Esophagus
Barrett’s esophagus can develop due to various risk factors. By understanding these risk factors and taking preventive measures, you can lower your chances of developing this condition. Some of the key risk factors for Barrett’s esophagus include:
- Obesity: Being overweight or obese increases the risk of developing Barrett’s esophagus. Maintain a healthy weight through regular exercise and a balanced diet.
- Smoking: Smoking cigarettes significantly raises the risk of developing Barrett’s esophagus. Quitting smoking is essential for both preventing this condition and improving overall health.
- Older age: Barrett’s esophagus is more commonly observed in individuals over the age of 50. Regular screenings and monitoring become crucial as you age.
- Male gender: Men are more prone to developing Barrett’s esophagus than women. As a man, stay vigilant and adopt healthy lifestyle choices.
- Caucasian ethnicity: People of Caucasian ethnicity have a higher susceptibility to Barrett’s esophagus. Understanding your risk profile enables you to take proactive measures.
- Family history: Having a family history of Barrett’s esophagus or esophageal cancer can increase your risk. Be sure to inform your doctor if this applies to you.
To prevent Barrett’s esophagus, it’s important to focus on managing gastroesophageal reflux disease (GERD) symptoms and minimizing exposure to stomach acid. Here are some preventive measures you can take:
- Maintain a healthy weight: Obesity is a significant risk factor for Barrett’s esophagus. By maintaining a healthy weight, you can reduce the risk of developing this condition.
- Quit smoking: Smoking not only raises the risk of Barrett’s esophagus but also increases the likelihood of developing complications. Quitting smoking is crucial for your overall health.
- Manage GERD symptoms: If you experience frequent heartburn, acid reflux, or other GERD symptoms, it’s important to manage them effectively. Lifestyle changes such as avoiding trigger foods, eating smaller meals, and elevating the head of your bed can help. Medications prescribed by your doctor can also provide relief.
- Practice good sleep habits: Elevating the head of your bed when sleeping aids in reducing acid reflux symptoms, potentially lowering the risk of Barrett’s esophagus.
By addressing these risk factors and adopting preventive measures, you can significantly reduce your chances of developing Barrett’s esophagus and its potential complications.
Risk Factors for Barrett’s Esophagus
| Risk Factors | Action Steps |
|---|---|
| Obesity | Maintain a healthy weight through regular exercise and a balanced diet. |
| Smoking | Quit smoking to reduce the risk of developing Barrett’s esophagus. |
| Older age | Get regular screenings and monitoring as you age. |
| Male gender | Adopt healthy lifestyle choices to lower the risk. |
| Caucasian ethnicity | Understand your risk profile and take proactive measures. |
| Family history | Inform your doctor if you have a family history of Barrett’s esophagus or esophageal cancer. |
By implementing these preventive steps and being vigilant about your overall health, you can help reduce the risk of developing Barrett’s esophagus and maintain a healthy esophageal lining.
Conclusion
In conclusion, early detection of Barrett’s esophagus is crucial in order to prevent the development of esophageal cancer. This condition often arises after years of experiencing gastroesophageal reflux disease (GERD), so it is important to recognize the symptoms such as frequent heartburn, chest pain, difficulty swallowing, vomiting blood, or black/tarry stools. Seeking medical attention promptly can lead to early diagnosis and improved treatment outcomes.
Treatment options for Barrett’s esophagus depend on the level of dysplasia present, which is determined through a tissue sample obtained during an endoscopy. Treatment may involve medication or surgical procedures such as Nissen fundoplication. It is essential to discuss these options with your doctor to determine the best course of action for your specific condition.
Additionally, lifestyle changes and regular follow-up appointments are key in managing Barrett’s esophagus and reducing the risk of complications. Making healthy choices, such as quitting smoking, maintaining a healthy weight, and avoiding trigger foods can have a positive impact. With proactive measures and diligent care, you can safeguard your health and improve your chances of early detection and successful treatment of Barrett’s esophagus.
FAQ
What are the symptoms of Barrett’s Esophagus?
Symptoms of Barrett’s esophagus may include frequent heartburn, chest pain, difficulty swallowing, vomiting blood, black or tarry stools.
What causes Barrett’s Esophagus?
The exact cause of Barrett’s esophagus is unknown, but it is commonly seen in people with GERD. Other risk factors include being male, Caucasian, over the age of 50, having H. pylori gastritis, smoking, and obesity.
How can I recognize the symptoms of Barrett’s Esophagus?
Symptoms such as frequent heartburn, chest pain, difficulty swallowing, vomiting blood, and black or tarry stools may indicate Barrett’s esophagus. If you experience any of these symptoms, it is important to seek medical attention.
How is Barrett’s Esophagus diagnosed and classified?
If your doctor suspects that you have Barrett’s esophagus, they may order an endoscopy. During the endoscopy, your doctor may take a tissue sample to further evaluate the condition of your esophagus. The tissue sample will be examined for dysplasia, which is the presence of abnormal cells.
What are the treatment options for Barrett’s Esophagus?
Treatment for Barrett’s esophagus depends on the level of dysplasia present. For patients with no or low-grade dysplasia, treatment may focus on managing GERD symptoms through medication or surgical procedures such as Nissen fundoplication or LINX device insertion. For patients with high-grade dysplasia, more invasive procedures may be recommended.
What are the complications of Barrett’s Esophagus?
The main complication of Barrett’s esophagus is an increased risk of developing esophageal cancer. Other complications may include chest pain, narrowing of the esophagus, and cuts or rupture of the esophagus.
What is the outlook for Barrett’s Esophagus?
Barrett’s esophagus raises the risk of developing esophageal cancer, but many people with this condition never develop cancer. It is important to work with your doctor to create a treatment plan that focuses on managing GERD symptoms and to regularly follow up for monitoring.
What is Barrett’s Esophagus?
Barrett’s esophagus is a condition in which the normal lining of the esophagus is damaged by acid reflux and replaced by a type of cell similar to that found in the intestines.
What are the risk factors and prevention measures for Barrett’s Esophagus?
Risk factors for developing Barrett’s esophagus include obesity, smoking, older age, male gender, Caucasian ethnicity, and a family history of the condition or esophageal cancer. Prevention measures include maintaining a healthy weight, quitting smoking, and managing GERD symptoms through lifestyle changes and medication.
What can I conclude about Barrett’s Esophagus?
Early detection of Barrett’s esophagus is important to prevent the development of esophageal cancer. Treatment options depend on the level of dysplasia present. By recognizing and addressing the symptoms, working with your doctor, and following the recommended treatment plan, you can safeguard your health and take proactive steps towards early detection and treatment.
Source Links


