Are you or a loved one suffering from Barrett’s Esophagus? If so, there is new hope on the horizon. Recent advancements in medical treatments have brought us closer to finding a cure for Barrett’s Esophagus, offering renewed hope and improved outcomes for those affected by this condition.
Table of Contents
ToggleBarrett’s Esophagus is a condition where the cells lining the esophagus change, putting individuals at a higher risk of developing esophageal cancer. For years, finding a cure has been a challenge, but with cutting-edge advancements and dedicated research, scientists and medical professionals have made significant progress in understanding this condition and developing effective treatment options.
Advancements in screening, diagnosis, and treatment modalities provide patients with a glimmer of hope. Early detection plays a crucial role in improving patient outcomes, and innovative technologies, such as radiofrequency ablation and cryotherapy, are offering promising results in removing precancerous cells and reducing the risk of esophageal cancer development.
As we delve deeper into this article, we will explore the prevalence of Barrett’s Esophagus, its risks, pathophysiology, and the importance of regular surveillance. We will also discover the various treatment options available and the role of multidisciplinary care in managing this condition effectively.
Throughout this journey, we will also highlight the significance of lifestyle modifications and prevention strategies. By understanding the importance of managing gastroesophageal reflux disease (GERD) and adopting a healthy lifestyle, we can significantly reduce the risk of developing Barrett’s Esophagus, ultimately working towards preventing its progression.
Stay tuned as we take a closer look at the groundbreaking research being conducted and the future directions in finding a cure. With each passing day, we are one step closer to providing individuals with a permanent solution and a renewed sense of hope.
Understanding Barrett’s Esophagus and its Risks
Barrett’s esophagus is a condition where the cells in the lining of the lower end of the esophagus change, resembling cells found in the intestines. This change is often a result of chronic gastroesophageal reflux disease (GERD), where stomach acid backs up into the esophagus.
People with Barrett’s esophagus are at a much higher risk of developing esophageal cancer. Precancerous nodules, also known as dysplasia, are a common finding in individuals with this condition. It is important to understand the risks associated with Barrett’s esophagus to ensure early detection and timely treatment.
The following table illustrates the risks of Barrett’s esophagus and its potential progression to esophageal cancer:
| Risks | Esophageal Cancer Progression |
|---|---|
| Precancerous nodules (dysplasia) | Possible development of esophageal cancer |
| Chronic gastroesophageal reflux disease (GERD) | Increased risk of developing Barrett’s esophagus |
| Obesity | Higher likelihood of developing Barrett’s esophagus |
| Smoking | Greater risk of esophageal cancer in individuals with Barrett’s esophagus |
Early detection and appropriate management of Barrett’s esophagus can help prevent the progression to esophageal cancer. If you have a history of GERD or other risk factors, it is essential to consult with your healthcare professional to determine the appropriate screening and surveillance protocols.
To further assess the risks associated with Barrett’s esophagus and understand the potential complications, it is essential to explore the prevalence of this condition and its impact on individuals.
The Prevalence of Barrett’s Esophagus
The prevalence of Barrett’s esophagus in the United States is on the rise, affecting approximately 2% to 7% of adults. This increase has been confirmed through a simulation model based on data from the Surveillance, Epidemiology, and End Results (SEER) program, which provides valuable insights into the prevalence of Barrett’s esophagus in the country.
It is crucial to highlight the growing prevalence of this condition to raise awareness and prompt early detection and treatment. Identifying Barrett’s esophagus at an early stage can significantly improve outcomes and reduce the risk of esophageal cancer.

Rising Prevalence in the United States
The data from the SEER program, coupled with the simulation model, reveals alarming trends in the prevalence of Barrett’s esophagus in the United States. The increase in cases highlights the need for proactive measures to address this condition.
The Importance of Increased Awareness
With the rising prevalence of Barrett’s esophagus, it is imperative to increase public awareness about the condition. Educating individuals about the risk factors, symptoms, and available screening methods can encourage early detection and prompt treatment.
Prompt Detection and Treatment Efforts
The findings from the simulation model and SEER data underscore the importance of early detection and intervention for Barrett’s esophagus. Timely screening and treatment can help prevent the progression of the disease to esophageal cancer, significantly improving patient outcomes.
Screening Efforts and Public Health Initiatives
Given the growing prevalence of Barrett’s esophagus, it becomes crucial to prioritize screening efforts and implement effective public health initiatives. These initiatives can help identify individuals at risk and ensure timely intervention, leading to better prognosis and reduced mortality rates.
Pathophysiology and Risk Factors
Understanding the pathophysiology of Barrett’s esophagus is key to comprehending its development and progression. This condition arises from chronic reflux esophagitis, leading to changes in the esophageal lining. Inflammation and specialized intestinal metaplasia play crucial roles in this transformation.
Chronic exposure to stomach acid causes inflammation in the sensitive esophageal tissues. Over time, the constant irritation triggers molecular genetic changes, resulting in specialized intestinal metaplasia. This process involves the replacement of normal squamous epithelial cells with columnar epithelial cells typically found in the intestines.
Furthermore, cell cycle abnormalities further contribute to the progression of Barrett’s esophagus. The disrupted cell cycle allows abnormal cells to persist and accumulate, increasing the risk of dysplasia and esophageal cancer development.
Several risk factors have been associated with the development of Barrett’s esophagus. Caucasian race, male gender, age over 50, central obesity, and a history of gastroesophageal reflux disease (GERD) are common risk factors for this condition. Smoking and a family history of Barrett’s esophagus also elevate the risk.
Key Points:
- Barrett’s esophagus results from chronic reflux esophagitis and inflammation.
- Specialized intestinal metaplasia involves the replacement of normal esophageal cells with intestinal-like cells.
- Cell cycle abnormalities contribute to disease progression.
- Risk factors include Caucasian race, male gender, age over 50, central obesity, history of GERD, smoking, and family history.
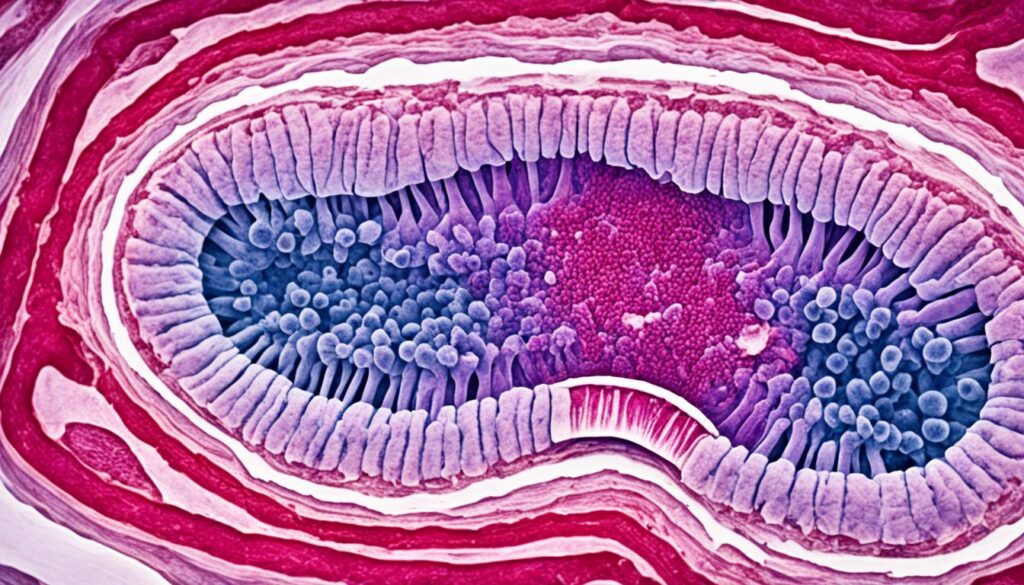
Image:
Advances in Screening and Diagnosis
Screening and early detection play a vital role in managing Barrett’s esophagus effectively. Thanks to advancements in medical technology, endoscopic procedures have become a key tool in the diagnosis of this condition. One commonly used procedure is esophagogastroduodenoscopy (EGD), which allows doctors to visualize the esophagus and detect any abnormal changes.
To standardize the diagnosis of Barrett’s esophagus based on endoscopic findings, the Prague C & M criteria have been developed. These criteria help healthcare professionals accurately assess the extent and severity of the condition, providing them with valuable information for further management decisions. The Prague C & M criteria consider various parameters, including the length and circumference of the abnormal tissue within the esophagus.
| Parameter | Score |
|---|---|
| Maximum circumferential extent of Barrett’s esophagus (C) | |
| Maximum circumferential extent of Barrett’s esophagus occupied by tongues (C) | |
| Maximum length of tongues (M) | |
| Circumference of Barrett’s esophagus at the diaphragmatic hiatus (C) |
These advances in screening and diagnosis have significantly improved the ability to identify individuals at risk for Barrett’s esophagus. With early detection, healthcare providers can implement appropriate management strategies to prevent further progression and ensure better patient outcomes.
Management and Treatment Options
Effective management of Barrett’s esophagus involves various treatment options. These options aim to remove or destroy the precancerous cells in the esophagus, reducing the risk of esophageal cancer development. The following are some of the treatment options:
- Radiofrequency Ablation (RFA): A minimally invasive procedure that uses electrical waves to remove abnormal tissue in the esophagus. RFA has shown promising results in eliminating precancerous cells and improving long-term outcomes. (Keywords: Barrett’s esophagus, radiofrequency ablation)
- Cryotherapy: This treatment option uses extreme cold to freeze and eliminate abnormal cells in the esophagus. Cryotherapy can effectively target and destroy precancerous tissue, offering an alternative to surgical intervention. (Keywords: Barrett’s esophagus, cryotherapy)
- Endoscopic Mucosal Resection (EMR): When the precancerous cells are limited to the surface of the esophagus, EMR may be used to remove the affected tissue. This procedure can be an effective treatment option in selected cases. (Keywords: Barrett’s esophagus, endoscopic mucosal resection)
- Argon Plasma Coagulation (APC): This technique uses ionized gas to destroy abnormal cells in the esophagus. APC can be an effective treatment option for addressing dysplasia and reducing the risk of cancer development. (Keywords: Barrett’s esophagus, argon plasma coagulation)
Individual cases may require a combination of these treatment options based on factors such as the extent of Barrett’s esophagus and the presence of dysplasia. Your healthcare provider will determine the most appropriate treatment plan for your specific situation.

Importance of Surveillance and Follow-up
Regular surveillance and follow-up are essential for individuals with Barrett’s esophagus to monitor disease progression and detect any signs of dysplasia or esophageal cancer. The frequency of surveillance endoscopy is determined by the presence and grade of dysplasia.
For patients with non-dysplastic Barrett’s esophagus, surveillance endoscopy is recommended every three to five years. Patients with low or high-grade dysplasia or stage T1a esophageal adenocarcinoma require more frequent surveillance to ensure timely intervention and improved cancer detection rates.
The Importance of Surveillance
Surveillance plays a crucial role in managing Barrett’s esophagus by allowing healthcare professionals to closely monitor the condition and detect any abnormalities. Regular follow-up appointments and endoscopic procedures enable the early identification of dysplasia and cancer, leading to timely intervention and a higher chance of successful treatment.
During surveillance endoscopy, the healthcare provider examines the esophagus using a thin, flexible tube with a camera attached to it. This procedure allows for a detailed evaluation of the esophageal lining, enabling the detection of any changes or abnormalities.
By tracking the progression of Barrett’s esophagus and identifying the presence of dysplasia, healthcare professionals can intervene promptly to prevent the development of esophageal cancer. Surveillance also provides an opportunity to reassess treatment strategies and make any necessary adjustments to improve patient outcomes.
Follow-up Recommendations
The follow-up recommendations for patients with Barrett’s esophagus depend on the presence and grade of dysplasia. Here is a breakdown of the recommended surveillance intervals for different patient groups:
| Patient Group | Surveillance Recommendations |
|---|---|
| Non-dysplastic Barrett’s Esophagus | Surveillance endoscopy every three to five years |
| Low-grade Dysplasia | Surveillance endoscopy every six to twelve months |
| High-grade Dysplasia | Surveillance endoscopy every three to six months |
| Stage T1a Esophageal Adenocarcinoma | Surveillance endoscopy every three months for the first year and every six months thereafter |
Detecting dysplasia or esophageal cancer at an early stage significantly improves the chances of successful treatment and better patient outcomes. Therefore, it is crucial for individuals with Barrett’s esophagus to adhere to the recommended surveillance and follow-up schedule prescribed by their healthcare provider.
Patient Outcomes and Prognosis
Advancements in screening, diagnosis, and treatment options have significantly improved the prognosis for patients with Barrett’s esophagus. Early detection and intervention are key in achieving positive outcomes. In fact, when esophageal cancer is caught at an early stage, Barrett’s esophagus can be curable, with high survival rates.
Regular surveillance and adherence to treatment recommendations play a crucial role in improving patient outcomes and prognosis. By closely monitoring the condition and following the prescribed treatment plan, healthcare professionals can detect any signs of disease progression or the development of dysplasia, a precursor to cancer. Timely intervention can then be initiated, potentially saving lives and enhancing the chances of long-term remission.
It is important for patients with Barrett’s esophagus to understand the significance of regular follow-up appointments and surveillance endoscopies. These appointments allow healthcare providers to closely monitor the condition, assess the effectiveness of treatment, and detect any early signs of complications. By actively participating in their own care, patients can help ensure the best possible outcomes.
Ultimately, the prognosis for patients with Barrett’s esophagus is dependent on early detection, adherence to treatment recommendations, and regular surveillance. With the advancements in healthcare practices and the collaboration between healthcare providers and patients, the hope for a cure and improved patient outcomes continues to grow.

Importance of Multidisciplinary Care
When it comes to managing Barrett’s esophagus, a multidisciplinary approach is crucial for providing comprehensive care to patients. A collaborative effort between oncologists, surgical oncologists, and advanced endoscopists ensures that you receive the most appropriate treatment options and ongoing support throughout your journey.
By bringing together the expertise of various specialists, multidisciplinary care optimizes your chances of successful treatment and improved outcomes. Each professional plays a vital role in addressing the unique complexities of Barrett’s esophagus, tailoring interventions to suit your individual needs.
Here’s a breakdown of how each specialist contributes to your multidisciplinary care:
1. Oncologist
Your oncologist specializes in the diagnosis, treatment, and management of cancers, including esophageal cancer associated with Barrett’s esophagus. They play a key role in assessing your overall health, determining the stage of the disease, and recommending appropriate treatment options based on the latest advancements in oncology.
2. Surgical Oncologist
A surgical oncologist is trained in performing complex surgical procedures to remove cancerous tumors. In the case of advanced esophageal adenocarcinoma, surgical intervention may be necessary. Your surgical oncologist works closely with other team members to develop an individualized surgical plan and ensure the best possible outcome for you.
3. Advanced Endoscopist
An advanced endoscopist specializes in advanced endoscopic procedures, such as radiofrequency ablation (RFA) and cryotherapy. These minimally invasive techniques are used to remove or destroy abnormal cells in the esophagus. Your advanced endoscopist will carefully evaluate your specific condition and consider the most suitable endoscopic treatment options for you.
By combining the expertise of these specialists, multidisciplinary care addresses the complex nature of Barrett’s esophagus, providing you with comprehensive treatment options and ongoing support. This collaborative approach ensures that you receive the highest standard of care throughout every stage of your treatment journey.
Promising Research and Future Directions
Ongoing research in Barrett’s esophagus aims to identify novel therapeutic approaches and improve patient outcomes. Scientists and medical experts are dedicated to finding new ways to effectively manage and potentially cure this condition. Let’s explore some of the exciting areas of research and future directions in the field of Barrett’s esophagus.
Chemoprevention Strategies
One avenue of research focuses on chemoprevention, which involves the use of medications to prevent or slow the progression of Barrett’s esophagus. Researchers are investigating the potential of drugs like statins and aspirin in reducing the risk of developing esophageal cancer in patients with this condition. These medications may help suppress inflammation and inhibit the growth of abnormal cells, offering hope for better outcomes.
Targeted Therapies
Another area of research involves the development of targeted therapies for specific molecular abnormalities found in Barrett’s esophagus. By understanding the genetic and molecular characteristics of the condition, scientists are exploring innovative treatment options that can specifically target and eliminate abnormal cells without affecting healthy tissue. These personalized therapies hold promise for more effective and precise treatment approaches.
Improving Diagnostics and Screening
Advancements in diagnostic techniques and screening methods are also a focus of current research. Scientists are exploring ways to enhance the accuracy and efficiency of diagnosing Barrett’s esophagus at an early stage. This includes the development of imaging technologies and biomarker-based tests that can detect cellular changes associated with the condition. These advancements can lead to earlier intervention and improved patient outcomes.
Personalized Medicine
Personalized medicine is an emerging field that holds great potential for the future of Barrett’s esophagus treatment. By analyzing an individual’s genetic makeup and other factors, doctors will be able to tailor treatment plans to each patient’s unique needs. This approach can optimize the effectiveness of therapy and minimize adverse effects, ultimately leading to better outcomes for patients.
In conclusion, ongoing research in Barrett’s esophagus is paving the way for novel therapies and improved patient outcomes. Chemoprevention strategies, targeted therapies, advancements in diagnostics and screening, and personalized medicine are all areas of exploration that offer hope for better treatment options and possibly even a cure. As we continue to delve deeper into the complexities of this condition, the future looks promising for those affected by Barrett’s esophagus.
Lifestyle Modifications and Prevention
Making certain lifestyle modifications can help prevent the development or progression of Barrett’s esophagus. By managing gastroesophageal reflux disease (GERD) through lifestyle changes and medications, you can significantly reduce the risk of esophageal damage and subsequent Barrett’s esophagus. Adopting a healthy diet, maintaining a healthy weight, and avoiding known triggers like spicy foods and alcohol can also contribute to prevention efforts.
Lifestyle Modifications
Implementing simple lifestyle modifications can greatly improve your overall digestive health and reduce the risk of developing Barrett’s esophagus. Here are some key recommendations:
- Follow a healthy diet: Incorporate a variety of fruits, vegetables, whole grains, lean proteins, and low-fat dairy products into your meals. Limit your intake of processed foods, sugary snacks, and high-fat meals.
- Maintain a healthy weight: Obesity is a risk factor for GERD and Barrett’s esophagus. Engage in regular exercise and aim for a healthy weight to minimize the risk.
- Avoid trigger foods and drinks: Spicy foods, citrus fruits, tomato-based products, chocolate, coffee, and alcohol can all exacerbate GERD symptoms. Limit your consumption of these items to reduce the likelihood of acid reflux.
- Eat smaller, more frequent meals: Large meals can put pressure on your stomach, leading to acid reflux. Opt for smaller portions and try to eat at least three hours before going to bed.
- Quit smoking: Smoking weakens the lower esophageal sphincter, making it easier for stomach acid to flow back into the esophagus. Quitting smoking can help improve GERD symptoms and reduce the risk of Barrett’s esophagus.
Prevention
Preventing Barrett’s esophagus requires taking proactive steps to minimize GERD symptoms and manage the underlying condition effectively. Here are some preventive measures you can practice:
- Identify and manage triggers: Pay attention to the foods or activities that trigger your symptoms and try to avoid them. This may include certain types of food, physical activity after eating, or lying down immediately after a meal.
- Elevate the head of your bed: Raising the head of your bed by about six inches can help prevent acid reflux during sleep.
- Stay upright after meals: Avoid lying down or bending over for at least two hours after eating to allow digestion to occur properly.
- Avoid tight-fitting clothes: Wearing tight-fitting clothes can increase pressure on your abdomen and worsen GERD symptoms.
- Manage stress: Stress and anxiety can contribute to acid reflux. Practice stress-reduction techniques, such as deep breathing exercises, yoga, or meditation.
By implementing these lifestyle modifications and preventive measures, you can significantly reduce your risk of developing Barrett’s esophagus and improve your overall digestive health.
Conclusion
New advancements in finding a cure for Barrett’s esophagus provide hope for individuals affected by this condition. Through improved screening, diagnosis, and treatment options, the prognosis for patients with Barrett’s esophagus has significantly improved. Regular surveillance and adherence to treatment recommendations are critical for early detection and effective management. With ongoing research and multidisciplinary care, the future looks promising in the fight against Barrett’s esophagus, offering new hope for a cure and improved patient outcomes.
FAQ
What is Barrett’s esophagus?
Barrett’s esophagus is a condition where the cells lining the lower end of the esophagus change, resembling cells found in the intestines. It is often caused by chronic gastroesophageal reflux disease (GERD) and puts individuals at a higher risk of developing esophageal cancer.
What are the risks associated with Barrett’s esophagus?
People with Barrett’s esophagus are at a much higher risk of developing esophageal cancer, with precancerous nodules being a common finding. Early detection and timely treatment are crucial to prevent cancer progression.
How common is Barrett’s esophagus?
The prevalence of Barrett’s esophagus in the United States ranges from 2% to 7% of adults. Recent data suggests that the prevalence is increasing, highlighting the need for increased awareness and screening efforts.
What factors contribute to the development of Barrett’s esophagus?
Factors such as Caucasian race, male gender, age over 50, central obesity, history of GERD, smoking, and family history have been identified as risk factors for the development of Barrett’s esophagus.
How is Barrett’s esophagus diagnosed?
Endoscopic procedures, such as esophagogastroduodenoscopy (EGD), are commonly used for the diagnosis of Barrett’s esophagus. The Prague C & M criteria have been developed to standardize the diagnosis based on endoscopic findings.
What are the treatment options for Barrett’s esophagus?
Treatment options for Barrett’s esophagus include radiofrequency ablation (RFA), cryotherapy, endoscopic mucosal resection (EMR), and argon plasma coagulation (APC). These options aim to remove or destroy the precancerous cells and reduce the risk of esophageal cancer development.
How often should surveillance be done for Barrett’s esophagus?
The frequency of surveillance endoscopy depends on the presence and grade of dysplasia. For patients with non-dysplastic Barrett’s esophagus, surveillance endoscopy is recommended every three to five years. Patients with dysplasia or early-stage esophageal adenocarcinoma require more frequent surveillance.
What is the prognosis for patients with Barrett’s esophagus?
The prognosis for patients with Barrett’s esophagus has significantly improved due to advancements in screening, diagnosis, and treatment options. Early detection and intervention can lead to a cure, with high survival rates if esophageal cancer is caught at an early stage.
What is the importance of multidisciplinary care for Barrett’s esophagus?
Managing Barrett’s esophagus often requires a multidisciplinary approach involving various medical specialists, including oncologists, surgical oncologists, and advanced endoscopists. This collaborative approach ensures that patients receive the most appropriate treatment options and ongoing support.
What are the promising research areas in Barrett’s esophagus?
Ongoing research in Barrett’s esophagus aims to identify novel therapeutic approaches, such as chemoprevention strategies and targeted therapies for specific molecular abnormalities. These advancements hold promise for more effective and personalized treatment options in the future.
Can lifestyle modifications help prevent Barrett’s esophagus?
Making lifestyle modifications, such as managing GERD through lifestyle changes and medications, adopting a healthy diet, maintaining a healthy weight, and avoiding triggers like spicy foods and alcohol, can help prevent the development or progression of Barrett’s esophagus.
Source Links


