U.S.-Trained Female Gastroenterologist for IBS, Liver & Gut Health
With Holistic Approach to Healing
U.S.-Trained Female Gastroenterologist for IBS, Liver & Gut Health
With Holistic Approach to Healing

Dr. Nivedita Pandey
Senior gastroenterologist and hepatologist. Obesity specialist
MBBS, Diplomate of American Board of Internal Medicine (Internal Medicine), Diplomate of American Board of Internal Medicine (Gastroenterology)
Dr Nivedita Pandey is a Gastroenterologist, Trained in the U.S and provides pre transplant evaluation as well as post-liver transplant care. At present, Dr Nivedita is Senior Consultant, Gastroenterology and Hepatology, Sitaram Bhartia Institute of Science and Research, New Delhi and Transplant Hepatologist and Consultant Gastroenterologist, Max Super Specialty Hospital, Saket.
Conditions Treated
The disorders of the digestive system affect you in more ways than one. Usually, when we reflect on the human gastrointestinal system, people limit it to the stomach and intestines whereas in reality, gastroenterology examines the normal function and diseases of the esophagus, stomach, small intestine, colon and rectum, pancreas, gallbladder, bile ducts and the liver.

Gut & GI Disorders
- Gastroesophageal Reflux Disease(GERD)
- Irritable Bowel Syndrome (IBS
- Inflammatory Bowel Disease (IBD)
- Peptic Ulcer Disease
- Esophagus Disorders

Liver & Pancreas Care
- Liver Health & Disease Management
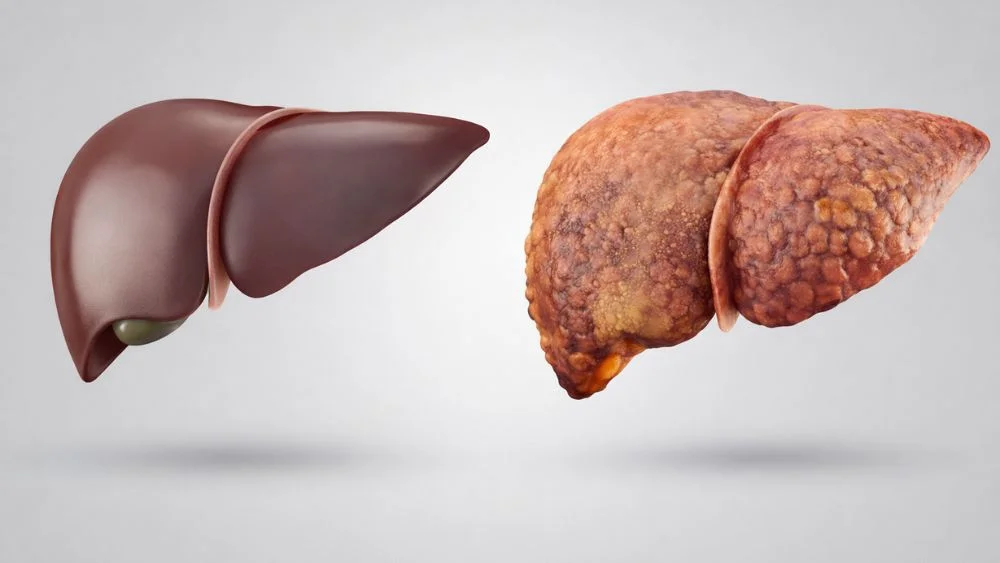
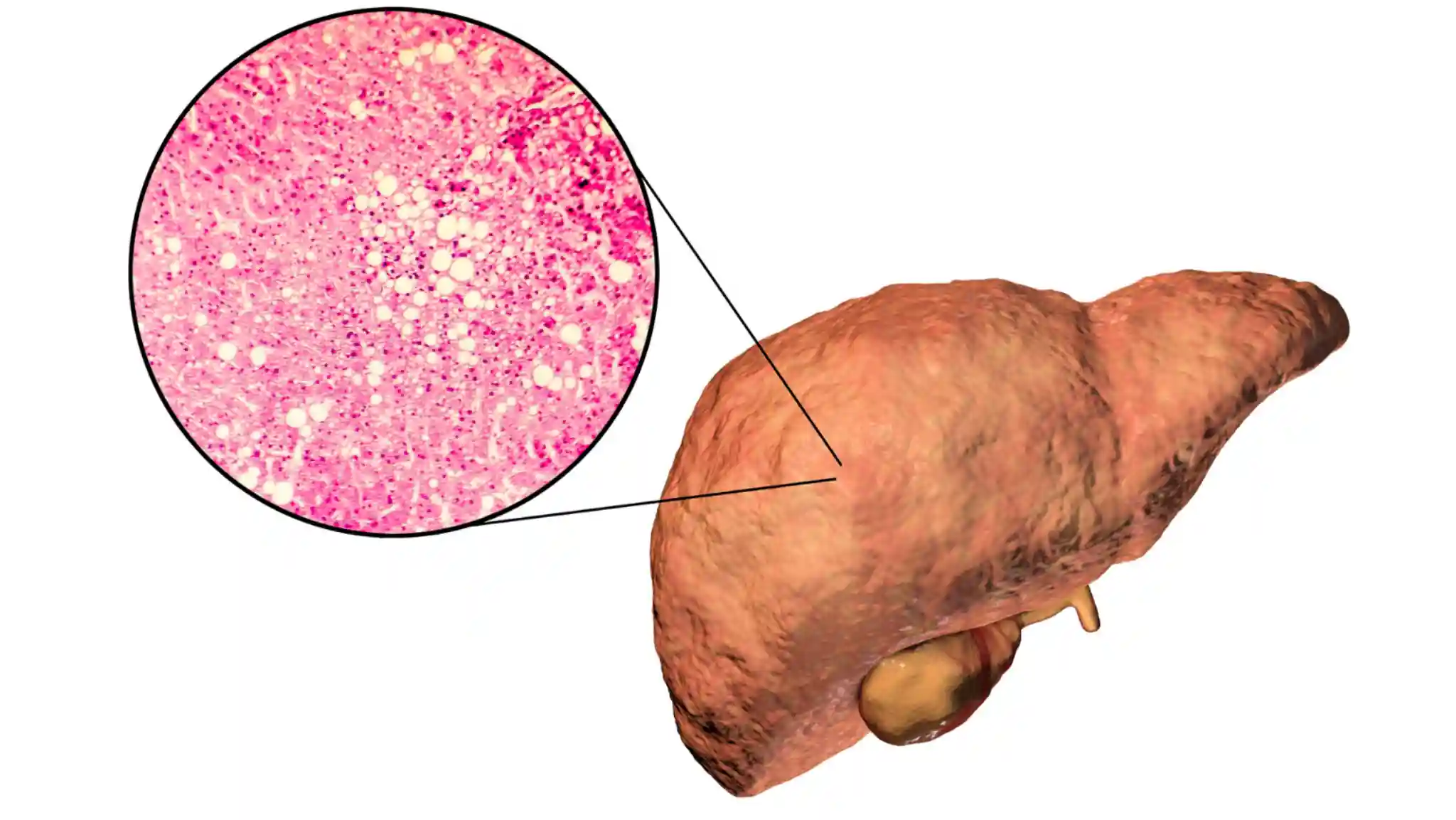
- Liver Cirrhosis
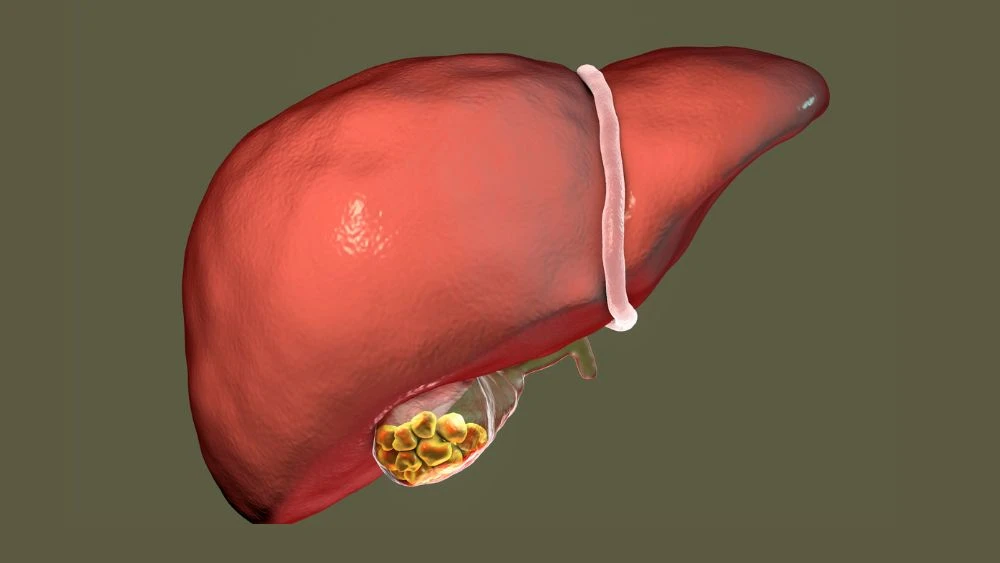
- Fatty Liver Disease (NAFLD/NASH)
- Pancreatitis
- Hepatitis A, B, C

Functional Nutrition & Wellness
- Leaky gut
- Nutrition counselling
- Lifestyle advise
- Colonic dysbiosis
- Weight management
- Supplement counselling
- Lifestyle management

GI Procedures & Endoscopy
- Endoscopic Ultrasound
- Capsule Endoscopy
- Colonoscopy
- Upper GI Endoscopy (UGIE)
- Sigmoidoscopy
Reviews
Trustindex verifies that the original source of the review is Google. God on earth. Can’t say more.Posted onTrustindex verifies that the original source of the review is Google. I came from Assam to consult her and she is Best best and best dont have any words to expressPosted onTrustindex verifies that the original source of the review is Google. I have been seeing Dr. Pandey for the past six years for Ulcerative Colitis and she has patiently helped me navigate through the disease. She never over medicates, and she listens patiently and empathetically. Please be prepared to wait for a while even if you have an appointment - that only happens because she does not rush her patients, and she will give you the same time that she gives to others.Posted onTrustindex verifies that the original source of the review is Google. Post covid-19, I was suffering from stomach issues and went to a lot of doctors but no where I could find complete solution. This was something which was bothering me not just physically but mentally as well. Since I have been seeing Nivedita ma'am, I feel way way way better physically and needless to say I am at peace mentally. I am not scared of what my body is going through now. There are very few doctors I suppose who connect to their patients on such a personal level. Ma'am made sure that my issue is resolved completely and moreover she made sure I am all positive all the time. All I have is genuine gratitude for ma'am, who is the bestest doctor and finest person. I have seen people complaining about her that she makes people wait for long time. I request them to understand the fact that she never ever let's anyone leave her room until the person completely convinced also she gives equal time to people complaining as well. I understand the waiting but yet request them to understand the reason behind it rather than just pointing it as a con.Posted onTrustindex verifies that the original source of the review is Google. I would really appreciate for the time and care Dr Nivedita Pandey gives to patient. I have personally visited and recommended many of relatives and friends for her consultation and all are doing well and are very thankful to Dr Pandey advice and care.Posted onTrustindex verifies that the original source of the review is Google. Top of the line. I have been consulting her for a few years now. I have found Dr. Pandey to be a skilled professional practising evidence based diagnoses and treatment. She correctly diagnosed and treated a long lingering stomach infection that I had. She likewise combines strong humanistic skills with her medical ones in an effective combination for proper treatment. I recommend her without reservations. Prof. SuriePosted on
Comprehensive Care from a Best Gastroenterologist
Gastroenterology is a medical specialty that focuses on the digestive system and its related problems. Gastroenterologist treat problems with the stomach, intestines, bowels, liver, gallbladder, esophagus, and pancreas, among other parts of the digestive system. Performs surgeries and cures cancer, ulcers, stomach pain, diarrhea, and jaundice, among other conditions. Gastrologist in Delhi, on the other hand, are physicians who specialize in treating stomach disorders.
Dr Nivedita Pandey is a best gastroenterologist. She received her medical degree from Maulana Azad Medical College in Delhi before pursuing super-specialisation in the United States. She received her internal medical training at the State University of New York, followed by a fellowship in gastroenterology and hepatology.
Specialisation of Dr Nivedita Pandey
Hepatology: With a focus on liver transplantation
A hepatologist is an expert withinside the department of medication known as Hepatology, which incorporates the observation of frame elements along with the liver, the biliary tree, the gallbladder and the pancreas. A hepatologist manages issues in those areas. Hepatology became historically a subspecialty of gastroenterology, however current advances withinside the information of this subspecialty have made it a discipline of its own.
Hepatologists deal maximum often with viral hepatitis and illnesses associated with alcohol.
Dr Nivedita Pandey has been working with one of the most prestigious clinics specialising in Living Donor Related Liver Transplantation (LDLT). Transplant hepatology necessitates knowledge and proficiency in a variety of medical specialities, including critical care, gastrointestinal surgery, and a solid understanding of pharmacology in order to adjust immunosuppression medications, pathology, interventional radiology, infectious diseases, and palliative care.
Gastroenterology
Gastroenterologists examine the whole digestive tract, from the mouth to the anus. It also includes researching pancreatic disorders. Dr Nivedita is one of the best female gastroenterologists in Delhi, India. There are just five or six female gastroenterologist in delhi. She is also an expert in the study of obesity and its link to stress, which results in unhealthy eating patterns.
Latest Blog Posts

Restore Your Gut Naturally
7 Days, 7 Simple Meals!
Reset your gut in 7 days with 7 simple meals! 🌿💚 Improve digestion, reduce bloating, and feel amazing—one meal at a time!