High bilirubin level means your blood holds more bilirubin than your body can clear. Bilirubin is a yellow waste product. Your body makes it when old red blood cells break down. Your liver changes it into a form that leaves through bile and stool. When this system slows or breaks, bilirubin builds up.
Table of Contents
ToggleA high bilirubin level often signals liver stress, blocked bile flow, or excess red blood cell breakdown. Some causes stay mild. Others need fast medical care.
Normal vs High Bilirubin Levels
Knowing normal values helps you judge risk early. Doctors never look at bilirubin alone. They read it with symptoms and other tests.
Normal Bilirubin Range in Adults
In healthy adults, total bilirubin usually stays between 0.2 and 1.2 mg/dL. Your liver processes bilirubin every day without effort. When lab values cross this range, doctors watch trends. A single mild rise may not matter. A repeated high bilirubin level often points to an underlying problem.
Direct bilirubin reflects processed bilirubin. Indirect bilirubin reflects unprocessed bilirubin. The balance between them matters. It helps doctors tell if the issue starts in the blood, liver, or bile ducts.
Normal Bilirubin Levels in Infants
Newborns often show higher bilirubin in the first days of life. Their liver enzymes are immature. Mild jaundice is common and usually fades. Doctors still track levels closely. Very high values can harm brain cells. In infants, even a short-term high bilirubin level needs careful monitoring.
When Bilirubin Levels Are Considered High
Doctors label bilirubin as high when adult values stay above 1.2 mg/dL. They act faster if levels rise quickly. A sudden high bilirubin level often suggests bile duct blockage or acute liver injury. Slow increases often point to chronic disease or genetic causes.
Causes of High Bilirubin
Bilirubin rises when red blood cells break down too fast, the liver cannot process waste, or bile cannot drain properly. Each cause leaves a different lab pattern, which helps doctors pinpoint whether the problem starts in blood, liver tissue, or bile ducts.
Liver Diseases
Your liver acts as the main filter. When liver cells swell or scar, bilirubin clearance drops. Fatty liver disease can raise bilirubin even before symptoms appear. Cirrhosis causes lasting damage and often leads to a persistent high bilirubin level . Liver tumors can also block bile flow inside the liver.
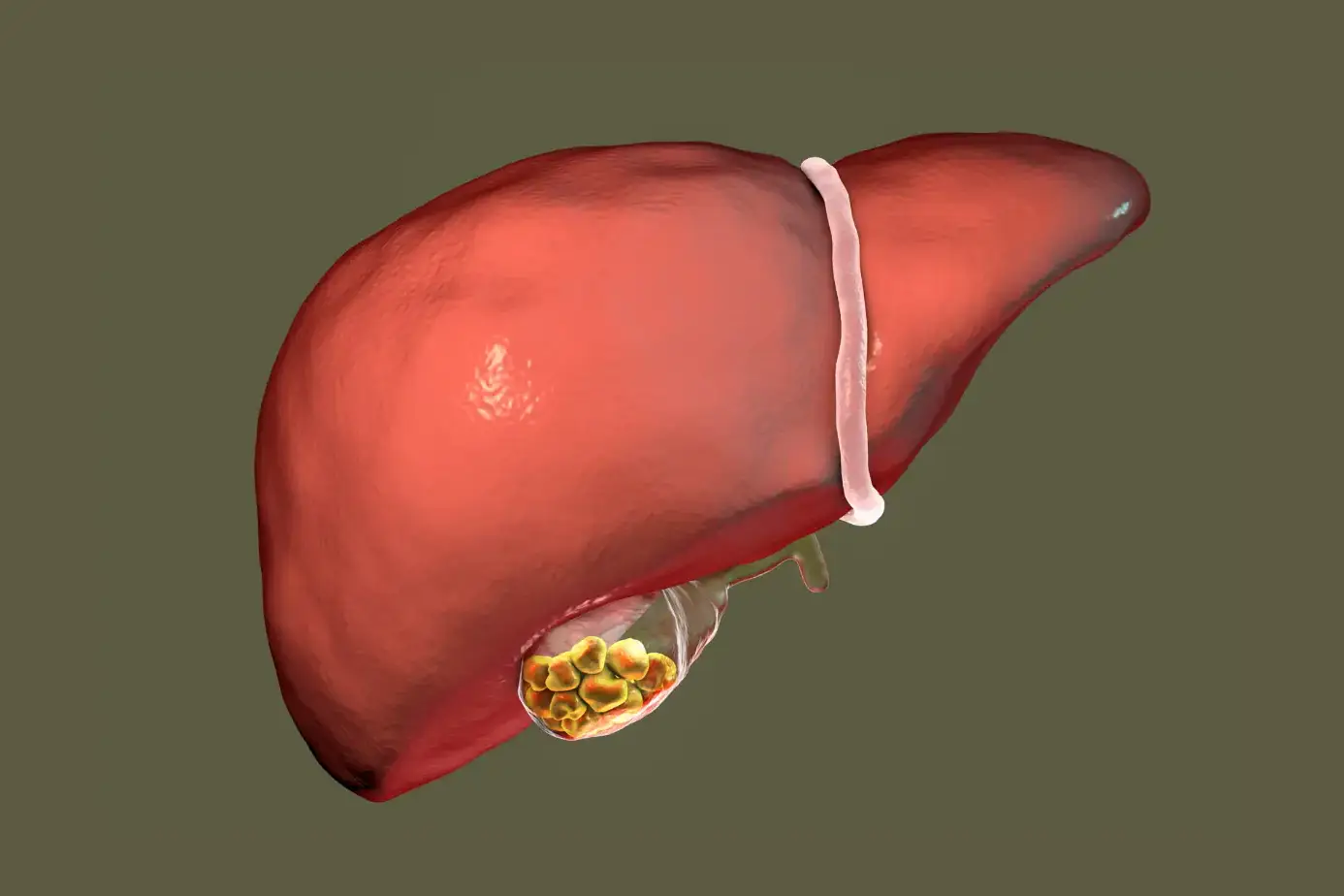
Bile Duct Obstruction
Bile ducts act like pipes. Gallstones, strictures (narrowed ducts), or tumors can block them. Bilirubin then leaks back into the blood. This cause often leads to dark urine and pale stools. Pain under the right ribs may appear. Obstruction can push a high bilirubin level up fast.
Hemolytic Disorders
Some conditions destroy red blood cells early. This floods your blood with bilirubin. Your liver may be healthy, but overwhelmed. Examples include certain inherited anemias and immune reactions. In these cases, indirect bilirubin rises first. This pattern helps doctors separate blood causes from liver causes.
Gilbert’s Syndrome
Gilbert’s syndrome is a common inherited condition. Your liver lacks enough enzyme to process bilirubin quickly. You may feel normal most days. Stress, illness, or fasting can raise bilirubin. This condition causes a mildly high bilirubin level without liver damage.
Viral Hepatitis
Viral hepatitis inflames liver cells. Inflamed cells process bilirubin poorly. Jaundice often appears during active infection. Some viruses cause short-term illness. Others become chronic and raise bilirubin over the years. The pattern of enzyme changes helps doctors confirm this cause.
Alcohol-Related Liver Damage
Alcohol harms liver cells over time. Early damage may show no symptoms. As injury grows, bilirubin clearance drops. A high bilirubin level in heavy drinkers often signals advanced liver stress. Stopping alcohol can slow further damage, but may not reverse scarring.
Medication-Induced Bilirubin Elevation
Some drugs interfere with liver enzymes or bile flow. Certain antibiotics, seizure drugs, and cancer treatments do this. Doctors always review your medication list when checking the causes of high bilirubin . Stopping or switching a drug often lowers levels safely.
Symptoms of High Bilirubin
Bilirubin buildup affects skin, urine, digestion, and energy levels. Symptoms often appear only after levels cross a visible threshold, which means internal stress may exist before signs become obvious.
Yellowing of Skin and Eyes (Jaundice)
Jaundice is the most visible sign. Yellowing starts in the whites of your eyes. It then spreads to the skin. It appears that once bilirubin crosses a visible threshold. A rising high bilirubin level makes jaundice deeper in color.
Dark Urine
Excess bilirubin is eliminated through urine. This turns urine dark brown or tea-colored. Many people notice this before skin changes. Dark urine often appears early in bile blockage.
Pale or Clay-Colored Stools
Bilirubin gives stool its brown color. Blocked bile flow removes this pigment. Stools turn pale or gray. This symptom strongly points to bile duct problems.
Fatigue and Weakness
Toxin buildup stresses your body. You may feel tired even after rest. Energy drops because digestion and nutrient absorption slow.
Itching
Bile salts collect under the skin when bile flow slows. This causes itching without rash. Scratching offers little relief. Itching often worsens at night.
Abdominal Pain
Pain may appear under the right ribs. It can feel dull or sharp. Pain often signals gallstones, liver swelling, or bile duct pressure.
Symptoms of High Bilirubin in Adults
Adults often show broader systemic effects because bilirubin elevation usually links to long-standing disease. Digestive changes, mental fog, and appetite loss often signal ongoing liver strain rather than a short-term issue.
Persistent Jaundice
Yellowing that lasts weeks needs evaluation. Chronic jaundice is often linked to long-term liver disease. It rarely resolves without treating the cause.
Digestive Disturbances
Poor bile flow disrupts fat digestion. You may feel bloated or nauseated after meals. Greasy stools may appear. These signs often track with a sustained high bilirubin level .
Unexplained Weight Loss
Chronic illness reduces appetite and nutrient use. Weight loss without effort raises concern. Doctors take this sign seriously.
Confusion or Cognitive Changes
Advanced liver disease lets toxins reach the brain. This affects focus and memory. You may feel slow or confused. These changes need urgent care.
Loss of Appetite
Many adults with liver stress lose interest in food. This worsens weakness and slows recovery. Appetite loss often appears alongside other symptoms of high bilirubin .
How Is High Bilirubin Diagnosed
Doctors combine bilirubin fractions, liver enzymes, imaging, and clinical signs to determine where bilirubin processing fails and how urgently treatment is needed.
Blood Bilirubin Test
This test measures total, direct, and indirect bilirubin. Total bilirubin shows the overall load in your blood. Direct bilirubin reflects bilirubin already processed by the liver. Indirect bilirubin shows bilirubin is still waiting for processing. This split helps identify the causes of high bilirubin . A rise in indirect bilirubin often points to blood cell breakdown. A rise in direct bilirubin often signals bile flow problems or liver cell damage.
Liver Function Tests
Liver function tests check enzymes and proteins made by the liver. These include ALT, AST, ALP, and albumin. High ALP with high bilirubin often suggests bile duct blockage. High ALT and AST suggest liver cell injury. These tests help confirm when a high bilirubin level comes from liver disease rather than blood disorders.
Imaging Tests
Imaging looks for physical blockages or damage. Ultrasound is usually the first step. It shows gallstones, bile duct widening, or liver swelling. CT or MRI scans give more detail if ultrasound results remain unclear. Imaging becomes critical when pain, fever, or a sudden high bilirubin level appears.
Genetic Testing
Genetic testing helps when common causes are ruled out. Doctors may test for inherited conditions like Gilbert’s syndrome. These tests explain long-term mild bilirubin elevation without liver injury. Genetic causes often explain stable but recurring high bilirubin level readings during stress or illness.
Liver Biopsy
A liver biopsy examines a tiny tissue sample. Doctors use it when blood tests and imaging fail to explain the bilirubin rise. It reveals scarring, inflammation, or rare liver diseases. Biopsy is invasive, so doctors reserve it for complex cases where a high bilirubin diagnosis remains unclear.
Treatment Options for High Bilirubin
Treatment focuses on correcting the underlying dysfunction rather than forcing bilirubin down. Addressing the cause allows bilirubin to normalize naturally while avoiding therapies that may stress the liver further.
Treating the Underlying Cause
Doctors focus on removing the trigger. They treat infections, manage autoimmune disease, or correct blood disorders. When the cause improves, bilirubin often falls naturally. This approach remains the safest and most effective way to correct a high bilirubin level .
Medications
Medications depend on the diagnosis. Antivirals may treat hepatitis. Steroids may reduce immune-driven liver injury. Drugs may also reduce itching caused by bile buildup. Doctors adjust treatment carefully since some drugs can worsen bilirubin levels.
Lifestyle and Dietary Changes
Alcohol avoidance is critical when bilirubin rises. Balanced meals support liver repair. Adequate protein helps healing, while excess fat can worsen symptoms. Hydration supports bile flow. These steps help stabilize a high bilirubin level over time.
Surgical Treatment
Surgery becomes necessary when the bile ducts are blocked. Removing gallstones or tumors can rapidly lower bilirubin. Procedures may be minimally invasive or open, depending on severity. Surgical relief often leads to quick improvement in jaundice.
Hospital-Based Management
Severe cases need close monitoring. Doctors track labs daily and manage complications like infection or bleeding. Very high bilirubin can affect brain function. Hospital care ensures safe correction when a high bilirubin level threatens vital organs.
How to Prevent High Bilirubin
Prevention centers on reducing liver workload and avoiding repeated injury. Long-term habits matter more than short fixes, especially for people with existing liver or blood conditions.
Maintaining Liver Health
You protect your liver by limiting processed foods and excess sugar. Regular activity improves fat metabolism in the liver. Vaccination against hepatitis reduces viral risk. These steps help prevent high bilirubin linked to liver injury.
Avoiding Excess Alcohol
Alcohol directly damages liver cells. Even moderate daily intake can worsen existing liver stress. Reducing or stopping alcohol lowers the risk of developing a high bilirubin level later in life.
Managing Chronic Liver Conditions
People with chronic hepatitis or fatty liver need regular follow-up. Monitoring labs helps catch rising bilirubin early. Timely treatment slows disease progression and helps prevent high bilirubin complications.
Safe Medication Use
Many drugs pass through the liver. Mixing medications without guidance increases risk. Always follow prescribed doses. Inform doctors about supplements. Safe use reduces medication-related bilirubin rise.
Regular Health Checkups
Routine blood tests catch silent changes. Early detection allows simple fixes before damage spreads. Regular checkups remain one of the strongest ways to prevent high bilirubin from becoming severe.
Complications of Untreated High Bilirubin
Persistent bilirubin elevation signals ongoing damage. Over time, this damage spreads beyond the liver, affecting digestion, brain function, and overall survival if left unaddressed.
Chronic Liver Damage
Ongoing bilirubin elevation reflects ongoing liver stress. Over time, healthy tissue turns into scar tissue. A scarred liver cannot regenerate fully, leading to lasting dysfunction.
Liver Failure
When scarring spreads, the liver loses vital functions. It cannot filter toxins or produce clotting proteins. Liver failure is life-threatening and may require a transplant.
Gallbladder Complications
Blocked bile thickens and forms stones. Infection may develop in the bile ducts. These issues cause severe pain and fever and often require surgery.
Neurological Complications
Very high bilirubin affects the brain. Confusion, sleep changes, and slowed thinking may occur. In infants, extreme levels can cause permanent brain injury.
When to See a Doctor
Certain bilirubin-related symptoms indicate rapid disease progression. Early medical evaluation prevents irreversible damage and allows treatment before complications become life-threatening.
Sudden Rise in Bilirubin Levels
A rapid jump often signals obstruction or acute liver injury. Immediate testing helps prevent organ damage.
Persistent or Worsening Jaundice
Yellowing that deepens or spreads needs evaluation. Persistent jaundice often reflects ongoing disease.
Severe Abdominal Pain
Sharp or constant pain under the ribs suggests gallstones or liver swelling. Pain with fever needs urgent care.
Signs of Liver Failure
Confusion, easy bleeding, swelling, or severe fatigue require emergency evaluation. These signs indicate advanced disease.
FAQs
Is high bilirubin dangerous?
A high bilirubin level can be harmless or serious. Mild genetic causes may not cause harm, but persistent elevation often signals liver or bile duct disease that needs medical care.
Can high bilirubin go away on its own?
Some mild cases resolve once the illness or stress passes. Other cases persist until the cause is treated. Doctors monitor trends before deciding if treatment is needed.
Does high bilirubin always mean liver disease?
No. Blood disorders and bile duct blockage also raise bilirubin. Doctors separate causes by checking direct and indirect bilirubin along with other tests.
What foods should I avoid if bilirubin is high?
Avoid alcohol and heavy fatty meals. Focus on balanced meals with fruits, vegetables, lean protein, and enough fluids to support liver function.
How long does it take to lower bilirubin levels?
The timeline depends on cause. Blockages may resolve quickly after treatment. Chronic liver disease may take weeks or months to stabilize bilirubin levels.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin