Toxic megacolon is a serious and sometimes deadly issue. It arises from inflammation in the colon. This causes the colon to swell without blockage. Usually, it’s linked with a wide-spread body response which is toxic. There are many things that can start toxic megacolon. This includes diseases like ulcerative colitis and Crohn’s, and infections such as Clostridium difficile. Even certain medicines and medical procedures, like colonoscopy, can trigger it. Quick detection and treatment are crucial to avoid severe problems like a burst colon.
Table of Contents
ToggleUnderstanding Toxic Megacolon
Definition and Causes
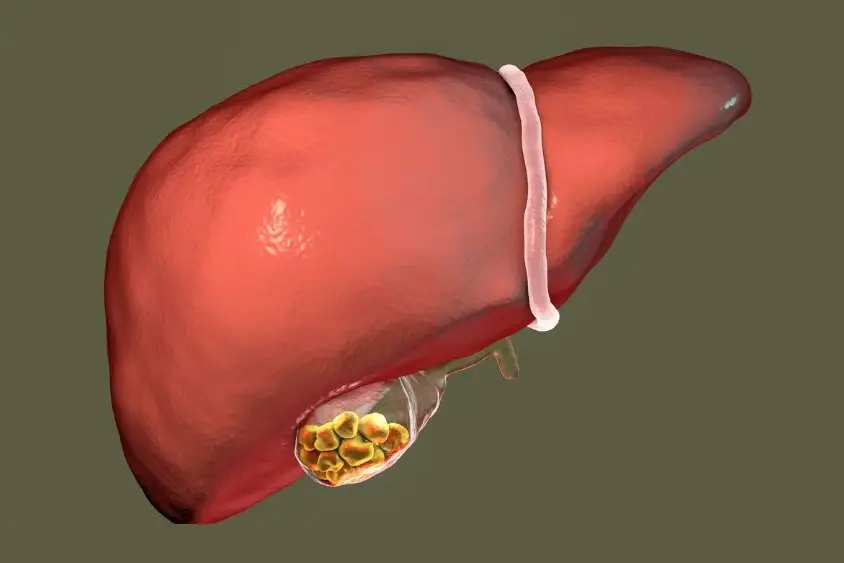
Toxic megacolon is a condition where the colon expands without a blockage. This can happen throughout the colon or in parts. It is linked to overall body toxicity. The main causes are diseases like ulcerative colitis and Crohn’s.
Infections from bacteria like Clostridium difficile and others can also cause this condition. Low potassium levels, some drugs, and even colonoscopies can make toxic megacolon more likely.
Inflammatory and Infectious Etiologies
Ulcerative colitis and Crohn’s disease are the top reasons for toxic megacolon. Infections, including from Clostridium difficile, play a significant role too. So do bacteria like Salmonella and Shigella.
Other infections that can lead to this problem are Campylobacter, E. coli, cytomegalovirus, and Entamoeba. Cytomegalovirus affects people with HIV/AIDS the most. On the other hand, Entamoeba is rare.
Risk Factors and Epidemiology
Those with inflammatory bowel diseases are most at risk for toxic megacolon. This is especially true in the early stages of their illness. The risk is highest in ulcerative colitis cases.
For ulcerative colitis, 8-10% of cases can lead to toxic megacolon. For Crohn’s disease, it’s between 2.3-6.3%. Toxic megacolon because of Clostridium difficile has become more common since 1990.
Before 1990, its occurrence was at 0.4%. After 1990, this rate jumped to 4.3%. About 20% of people in hospitals carry Clostridium difficile without showing symptoms. However, only 1% of hospital patients will develop symptoms from this infection.
Pathophysiology of Toxic Megacolon
The exact cause of toxic megacolon isn’t completely known. It seems to start because of inflammation in the colon’s lining. This inflammation lets out things like inflammatory mediators and bacterial products. It also makes the body produce more of a certain enzyme.
This enzyme, called inducible nitric oxide synthase, causes the colon to make too much nitric oxide. This makes the colon wider. People with toxic megacolon often have a lot of this enzyme in their colon’s deeper layers.
Role of Inflammatory Mediators
Inflammatory mediators and bacterial stuff are important in toxic megacolon’s growth. They start the body making too much of an enzyme. This enzyme is crucial for the illness to happen.
Nitric Oxide and Colonic Dilation
Too much nitric oxide plays a big role in toxic megacolon. It makes the colon’s muscles get wide and weak. People with this illness have more of the enzyme that causes nitric oxide in their colon. This is why their colon gets wider.
Diagnosis and Evaluation
Clinical Presentation and Physical Examination
People with toxic megacolon come in with a swollen belly and a lot of pain. They often feel sick and throw up. Their poop might be bloody or just watery. They also might not be thinking clearly.
When the doctor checks them, they seem very unwell. Their belly hurts a lot when touched. And, the normal sounds of the stomach moving aren’t there. They might be low on fluids and salts, have low blood pressure, low red blood cell count, and their organs might not be working well. Feeling like the belly is sore all over could mean the intestine is broken.
Laboratory Tests and Imaging Modalities
The doctor will look for some key signs on tests to diagnose toxic megacolon. They need to see that the colon is too wide on an x-ray, and then observe at least three of the following: fever, rapid heart rate, a high white blood cell count, anemia, needing more fluids, salt problems, or not thinking right.
A regular x-ray is often enough to show what’s wrong. But sometimes, a CT scan, like a detailed x-ray, is needed to check things better without poking the belly with a scope. Using a scope to look inside the colon is usually a bad idea because it might make a hole in the gut.
Medical Management of Toxic Megacolon
The first step to treat toxic megacolon is being there for the patient. They’re admitted to the intensive care unit. Doctors keep a close eye on their lab tests and how they’re doing. They stop any medicine that might make things worse. And they make sure the patient gets enough fluids through a vein. It’s also key to fix any problems with the body’s minerals, like not enough potassium.
Supportive Care and Fluid Resuscitation
Supportive care is vital in toxic megacolon treatment. It means watching how the patient is doing closely. They’re given fluids through a vein to stay hydrated. And any issues with the body’s minerals are taken care of. Doctors check the patient’s heartbeat, blood tests, and how they look all the time. This helps them notice and deal with problems quickly.
Addressing the Underlying Cause
It’s important to treat the main issue in toxic megacolon. If it’s because of an inflammatory bowel disease, like ulcerative colitis, more intense treatment is used. This might include steroids, drugs that change the immune response, or special biological treatments. If the megacolon comes from an infection, the right antibiotic is needed.
Antibiotic Therapy for Infectious Causes
For infections causing toxic megacolon, quick antibiotic therapy is a must. The right antibiotics should be used based on lab tests and what works best in the area. Starting these medicines early is key. It helps clear the infection and stops complications.

Megacolon Treatment
In treating toxic megacolon, about half of patients find success with medicine. When these treatments don’t work, surgery is often needed. Doctors use surgery if the patient’s condition doesn’t improve, they risk a tear in the bowel, or their colon is too large. The main surgery is to remove most of the colon and create an opening in the front of the stomach.
Indications for Surgical Intervention
When medicine fails to help, or if the patient is at risk of a bowel tear, surgery becomes necessary. This is especially true if the colon has grown too large. Fast surgery is crucial to avoid severe issues and to help the patient get better.
Subtotal Colectomy and Its Variations
The main surgery for toxic megacolon is a subtotal colectomy. This means taking out all the colon but the rectum remains. Other types of surgery are also done, like removing the colon and rectum fully, or creating a new way for the body to pass stool without needing a bag. All these surgeries aim to take out the sick part of the colon to prevent further problems.

Postoperative Care and Complications
After surgery for toxic megacolon, patients need extra care. They are closely watched and supported. This includes checking their signs often and watching for any issues. People are especially looked after for any bleeding, infections, or blocked intestines.
It’s vital to make sure patients get enough fluids and nutritional support. This is key to helping them heal well.
Monitoring and Management
If you have toxic megacolon surgery, expect a lot of support. Doctors and nurses will keep a close eye on you. They’ll check your signs and make sure your body’s minerals are in balance. If there are any problems like bleeding, infection, or a blocked gut, they’ll act fast and help out.
Getting the right amount of fluids and nutrients is very important. It allows your body to recover better and faster.
Potential Complications and Their Prevention
It’s crucial to manage any issues after toxic megacolon surgery. Some common problems are anastomotic leaks, bleeding, infections, and a blocked gut. Doctors take special care during surgery to lessen these risks. They give the right medicines and keep watching over you afterwards.
This care aims to give you the best chance at a smooth recovery from toxic megacolon treatment.

Clostridium Difficile-Associated Toxic Megacolon
Increasing Incidence and Severity
The number of cases of Clostridium difficile toxic megacolon has gone up in recent years. Before 1990, it was only 0.4%, but after 1990 it jumped to 4.3%. The rise is linked to stronger strains of C. difficile, like the NAP1/BI/027 strain.
This severe disease affects some patients with C. difficile infection. They are more likely to get toxic megacolon.
Treatment Strategies for C. difficile Infection
Patients with toxic megacolon need fast treatment. This includes antibiotics and other care. Doctors usually use metronidazole, vancomycin, or fidaxomicin to fight the infection.
Sometimes, surgery is needed if the patient doesn’t get better or if there’s a risk of the intestine tearing.

Toxic Megacolon in Inflammatory Bowel Disease
Toxic megacolon can happen in people with inflammatory bowel diseases like ulcerative colitis and Crohn’s disease. It’s more common in ulcerative colitis, affecting 8-10% of patients, than in Crohn’s disease, which occurs in 2.3-6.3% of cases. A big danger with inflammatory bowel disease is the risk of toxic megacolon, especially in the early stages of the disease.
Ulcerative Colitis and Crohn’s Disease
Studies give mixed results on toxic megacolon rates in inflammatory bowel disease. Some say it’s more often in ulcerative colitis (8-10%) than Crohn’s (2.3%). Others say it’s more common in Crohn’s (1-2.5%) than ulcerative colitis (4.4-6.3%). But, both diseases raise the risk of facing this severe issue.
Management Considerations
Treating toxic megacolon in inflammatory bowel disease calls for various approaches. These include care and addressing the underlying disease with surgery when needed. To reduce inflammation, doctors might use corticosteroids, immunomodulators, or biologics. They will also focus on antibiotics, fluids, and rest for the gut. Surgery, like subtotal colectomy, might be needed for some if their condition does not improve or if they develop serious complications.
Prognosis and Outcomes
The outlook for patients with toxic megacolon varies. It depends on several things. These include the cause, how big the colon has become, if it leads to problems like tearing, and how the person is overall. Those with rough diseases like Clostridium difficile or certain bowel diseases might have a tougher time. Quick spotting and strong treatment can make a big difference.
Factors Affecting Prognosis
For some, the chance of dying from toxic megacolon is 30% to 50%. This happens mostly if there are already serious health problems or if the colon tears. But, if it’s caught and treated early, less people die. What happens later for those who live depends on what caused it. People with certain bowel diseases may need constant care or even more surgeries.
Mortality Rates and Long-term Outcomes
If not managed soon, toxic megacolon can be deadly, with a 30% to 50% chance of dying, especially for those already very sick or if it tears the colon. But, quick management can lower this risk. After surviving, what comes next changes, mostly based on the cause. People with certain bowel diseases might have to keep up with their health very closely or get more surgeries.
Preventive Strategies
Recognizing toxic megacolon early and starting the right treatment fast are key. Doctors must always think about toxic megacolon in patients with gut diseases or infectious colitis. They should watch for its signs. Quickly starting supportive care and fixing the illness that caused it can stop it from getting worse.
Early Recognition and Prompt Treatment
Teaching patients is crucial to stop toxic megacolon. Those with gut diseases need to know what toxic megacolon looks like and why they must get treatment right away. It’s also important to take their medicine and see their doctor often. This way, problems can be caught early.
Patient Education and Compliance
Teaching patients to spot toxic megacolon early and to act fast helps a lot. Reminding them to keep up with their treatment and doctor visits can stop toxic megacolon from happening. This is especially true for those with gut diseases or other risks.
Special Considerations
Toxic Megacolon in Immunocompromised Patients
People with weakened immune systems are more likely to get toxic megacolon. This includes those with HIV/AIDS or in cancer treatment. For them, cytomegalovirus often causes this condition. So, doctors need to be on the lookout for it. Treating the main illness fast and giving strong support is crucial for these patients.
Pediatric and Geriatric Populations
Both kids and older adults can get toxic megacolon. In kids, problems like Hirschsprung’s disease or chronic pseudo-obstruction can cause it. Learning more about the causes is vital in these cases. For older adults, dealing with other health issues can make treating toxic megacolon harder. Doctors must really think about each person’s age and health when planning treatment.
Emerging Therapies and Future Directions
Researchers are looking into new ways to treat toxic megacolon. They are focusing on fecal microbiota transplantation (FMT) and new drugs.
Fecal Microbiota Transplantation
FMT is being studied for C. difficile infections. This infection can lead to toxic megacolon. FMT helps to restore the gut’s healthy bacteria, aiming to stop toxic megacolon from forming.
This method could be key in treating toxic megacolon with a novel approach.
Novel Pharmacological Agents
Other researchers are exploring new drugs for toxic megacolon. Some of these drugs target inflammation and nitric oxide production. There are also new antibiotics to fight infections.
Developing these new drugs and treatments may make surgery less necessary for patients.
By studying these new approaches, better and more personalized treatments might be available in the future.
Interprofessional Team Approach
Handling toxic megacolon well needs a team effort from many healthcare pros. This approach makes sure the patient gets complete care, from first diagnosis to getting better for the long term.
Roles of Different Healthcare Professionals
The interprofessional team for toxic megacolon includes many experts. There are gastroenterologists, colorectal surgeons, critical care pros, infectious disease doctors, nutritionists, and nurses. Each has a big part to play in helping the patient:
Gastroenterologists are key. They figure out what’s causing the problem, be it disease or infection. They lead the team in treatments, like medicine and watching the patient’s fluids and minerals.
Colorectal surgeons get involved when surgery is needed. This could be for a pierced bowel or a last resort when medicine doesn’t work. They might do a subtotal colectomy to remove parts of the colon that’s sick.
Critical care specialists watch over the patient in the ICU. They keep an eye out for problems and provide care to keep the patient stable. Infectious disease doctors help by choosing the right antibiotics if an infection caused the issue.
Nutritionists ensure the patient eats well, especially after surgery. Nursing staff are like the glue, always on top of the patient’s condition, giving meds, and making sure everyone’s on the same page.
This interprofessional team works together for the patient’s best. They use the latest knowledge to win against toxic megacolon, aiming for a great recovery.
FAQ
What is toxic megacolon?
Toxic megacolon is a severe and life-threatening condition. It happens when the colon gets very big without a blockage. This is often linked with a whole-body reaction to the growth.
What causes toxic megacolon?
Toxic megacolon is caused by certain diseases like ulcerative colitis and infections like Clostridium difficile. Other reasons include some medicines and things like colonoscopies.
What factors can precipitate toxic megacolon?
Certain things can make toxic megacolon more likely to happen. These include low potassium levels, specific medicines, and procedures like a colonoscopy.
What are the most common causes of toxic megacolon?
The top causes are diseases like ulcerative colitis and infections from bacteria like Clostridium difficile. These can make the colon severely swell.
Who is at the highest risk of developing toxic megacolon?
People with diseases that cause ongoing colon inflammation, especially when these conditions first appear, are at highest risk.
How does toxic megacolon develop?
Its exact cause is not fully known. But, it seems to start when the colon’s inner wall gets inflamed. This inflammation starts a series of events that make the colon swell.
What are the typical symptoms of toxic megacolon?
Toxic megacolon shows several signs. These include belly pain and getting very full. You might also feel sick and have diarrhea, which could have blood, and your thinking might be confused.
How is toxic megacolon diagnosed?
Doctors look for a swollen colon on scans. Though, to be sure it’s toxic megacolon, you must also have at least three of the following: fever, fast heart rate, high white blood cell count, being low on blood, losing liquids, bad balance of minerals in your blood, or thinking differently.
How is toxic megacolon treated?
At first, doctors focus on intensive care and fixing any body problems. They try to stop inflammation and deal with the reason why toxic megacolon started. Only if this doesn’t work or if there are signs that the colon might break, they might operate.
What is the most common surgical procedure for toxic megacolon?
The main surgery is to remove most of the colon and make an opening in the belly to remove waste. The end of the bowel that’s left is then brought out to the surface.
What are the potential complications of surgical management for toxic megacolon?
After surgery, some risks are leaks, bleeding, the wound sites getting infected, or the gut getting blocked again. These are common but can usually be managed.
How has the incidence of Clostridium difficile-associated toxic megacolon changed over time?
More people are getting toxic megacolon from Clostridium difficile these days, jumping from less than 0.5% in the past to over 4%. This is probably due to stronger forms of the bacteria.
What is the incidence of toxic megacolon in inflammatory bowel diseases?
Toxic megacolon happens at a rate of 8-10% in ulcerative colitis, and 2.3-6.3% in Crohn’s disease. These are the main two diseases that cause toxic megacolon.
What is the prognosis for patients with toxic megacolon?
A patient’s chance of getting better from toxic megacolon depends on many things. This includes what caused it, how serious it is, if it caused other problems, and the overall health of the patient. In some severe cases, toxic megacolon can be deadly.
How can toxic megacolon be prevented?
Recognizing toxic megacolon early and starting treatment promptly can avoid severe outcomes. Education for patients and ensuring they follow their treatment and check-ups can help avoid toxic megacolon.
How do special patient populations, such as the immunocompromised and the elderly, differ in terms of toxic megacolon?
People whose immune system isn’t strong, like those with HIV/AIDS or getting cancer treatment, have a higher chance of getting toxic megacolon. Older adults face more challenges because other health problems and being weak can complicate care for toxic megacolon.
What are some emerging therapies for the management of toxic megacolon?
New treatments include using healthy gut bacteria from someone else (FMT) to treat recurrent Clostridium difficile. There are also new drugs being developed to tackle the root causes of toxic megacolon.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Senior Gastroenterologist & Hepatologist
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.
About Author | Instagram | Linkedin